November 24th, 2014 §
 The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
Whole brain radiation will radiate all of my brain tissue, healthy and malignant. It is usually given in a series of 10-15 sessions, every weekday. It has side effects both short term and long term. In addition there is a claustrophobia-inducing session of mask-fitting where a mold of the face and head must be made for the patient to wear during radiation treatments to immobilize them. Here are some photos that one woman made of her WBR process.
I am meeting with the radiation team on Tuesday to get all of the details and do the scheduling. I haven’t met with them yet. I believe the goal is to start next week. I do not yet know what this means for the radiation procedures I had scheduled for my liver. I will also be continuing with chemo as much as is possible during this time. The most serious side effect will be fatigue. As in: sleep 20 or more hours a day fatigue. Can’t get out of bed fatigue. So I will need to make arrangements to get more help here at home to help with the kids and with driving.
For now that’s all I’m going to report because I want to see what the team says about my particular case and let everyone know the plan for me. It’s obviously not the news I was hoping for. But as always I will do what needs to be done to try to manage it.
November 7th, 2014 §
 This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
Unfortunately, what I learned while reviewing the scan with him is that I don’t just have two tumors in the liver. Instead there are actually many tumors in my liver, with those two being the largest. The fact there are so many tumors is why I am not a candidate for external beam radiation or other non-invasive treatment.
So far I am still a candidate for the Yttrium 90 radioembolyzation procedure where radioactive beads are inserted via a catheter snaked up through the groin into the hepatic artery and subsequently “feed” the tumors radioactive material as the beads work their way into the liver.
It will take three separate procedures spaced about two weeks apart to get this done. I will start the first week of December and finish in January. The first procedure involves mapping things out (in essence, a “dry run” where mock beads are inserted) and the next two are actual placement procedures. This is all a joint approach between interventional radiology and nuclear medicine. Before I start I will need a CT angiogram of the liver and a PET scan. After treatment I will have to monitor progress with PET scans every three months.
In the meantime we need to start on a new IV chemotherapy right away to try to see if we can find a chemo that will work on the liver tumors. We have no way of knowing if we will find one or what it will be. Right now my oncologist is eyeing Cisplatin, a platinum-based chemo like the Carboplatin I was on this summer. We will make the decision by next week and begin then.
The liver situation is serious. The cancer is growing rapidly there and we need to get it under control. Results of using Yttrium 90 for breast mets is pretty good, definitely good enough to proceed with it. To be honest, it is not a choice about whether to do it (I’m not at a point where I would consider doing nothing and stopping treatment, I realize that proceeding with any type of treatment is a choice in and of itself). There aren’t other options to treat these in a “batch” way.
So, there is a lot of adjustment right now. I feel sadness, disappointment, and anger that chemo has worked so well in some areas but the liver has been resistant. Things change so fast with this disease. One day things are relatively stable and within weeks they can be spiraling out of control.
As always, I will continue to educate and do what I can to show what my life with metastatic breast cancer is, what life with the disease can be.
For now, I will begin a new chemo and proceed with plans and pre-surgical testing for December. I’ve appreciated the emails and comments so much and I thank you all for your concern and wishes. I am sorry that I can’t respond to them all individually.
November 2nd, 2014 §
 Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Monday I saw my cardiologist to try to get some information about some symptoms I’d been having. My echo (and later in the week, the CT scan) showed there is some excess fluid around my heart. For now it is not causing any effect on heart function but we can’t rule out that it is a problem. I’ll have to repeat tests in a few weeks to try to see if it grows in volume (this would indicate a more sinister issue, and we would need to rule out a malignancy). For now, though, that goes on the back burner.
Tuesday I had bloodwork and IV fluids. The bloodwork is still a bit unclear about if the current chemo (Navelbine) is working. The rise in tumor markers is slowing but we need some definitive results this week, I think, to feel confident in interpreting them. The bloodwork also revealed I was anemic again, so on Thursday I went to New York City and got a transfusion of two units of blood.
On Friday I had a CT scan to compare to my last scan and help us make decisions about treatment. The CT showed both some good news and some concerns. While the lymph nodes and malignant tissue in my chest have resolved (chemotherapy in the last six months has worked and reduced those areas), my liver unfortunately shows two tumors.
The best thing at this time would be to biopsy portions of them (to gather tissue for future testing; my cancer has rarely been in areas that we can actually get samples, so this presents a rare chance to grab some) and also do ablation on them. Ablation is a localized procedure that when successful, destroys tumors of a particular size with very few side effects.
So, a lot is up in the air at the moment.
Because it is only Monday morning I don’t know what this week will bring in regards to chemo. We also don’t yet know if the interventional radiologists will decide that I am a good candidate for the ablation. For now, I wait.
Palbociclib, a drug I received through the expanded access (formerly “compassionate use”) program from Pfizer should arrive this week. That process took approximately 9 weeks and usually takes longer than that. I am fortunate my oncologist kept the process moving in such a timely manner (all applications and documents for such use must be done by the physician, not the patient).
I’m not feeling that well and have been primarily staying home for the last month. Now that I think about it, though, I’ve been basically staying home for the last ten months. Many days my half hour in the morning driving the older two kids to school is my only outing of the day. But I am patient.
At this point the options are still very reasonable and typical for this stage of the disease. I’m waiting for the next treatment proposal and then onward we go.
October 17th, 2014 §
My last post (“The Hardest Conversation”) showed you what a conversation with my teen daughter was like when we talked about my diagnosis of metastatic breast cancer in 2012. Today I wanted to share a conversation with my youngest child (now 8) that happened last year so you can see the variation in what their concerns were and how I dealt with each one.
As always, with cancer, age-appropriate explanations are important. Another vital piece of advice I’d like to share is that with all children, but especially young children, it is important to talk more than once about the topic. At the end of the first conversation I recommend asking young children, “Can you tell me what we talked about today?” to see if they have absorbed the most important pieces of information and that these pieces are correct. A day or two later it is always a good idea to ask, “Now that you’ve had time to think about our chat, do you have any questions?”
The following post was written in late 2013 on the eve of the surgery to put my medi-port in.
………………………………………………
 “Why do you have to have surgery tomorrow?” seven year-old Tristan asks from the back seat after we drop off his 11 and 15 year old siblings this morning.
“Why do you have to have surgery tomorrow?” seven year-old Tristan asks from the back seat after we drop off his 11 and 15 year old siblings this morning.
“Because I need to have something put in my body called a port. It’s a little container made of something cool called titanium that lets the doctors put some of my medicines into my body in an easier way.”
“Can you see it?”
“Yes, you will be able to see that there is a lump under my skin, about the size of a quarter. But you will only see the lump. You won’t see the actual thing because that will be inside my body. You know how I have the scar on the front of my neck? It will be like that, here, off to the side, same size scar but with a bump under it.”
“Is it like the bubble I had on my neck when I was a baby?”
“Well, that was a skin tag, so that was a lot smaller. And they were taking that away. This is something they are putting in to help make it easier to get some of my medicines. And you know when you go with me and I have blood taken from my hand? Well now sometimes they will be able to just take it from there instead. So it helps with a few jobs.”
“Will you have it forever or do they take it out when your cancer goes away?”
(Driving the car, trying to keep tears in check, knowing this is a vitally important conversation. I’ve explained this to him before but I know it’s hard for him to understand.)
“Well, honey, remember I had cancer when you were a baby? Well, this time the cancer is different. A lot of the time you can have cancer and the medicines and surgeries make it go away and it stays away for a long, long time. Maybe even forever. Sometimes any cancer cells that might be left go to sleep and just stay that way. Sometimes you have bad luck and they wake up. Mine woke up after six years. And now the cancer cells are in places that I won’t be able to get rid of them all for good. I am always going to have cancer. This time my cancer is the kind that is always going to be here.”
“You’ll always need medicine. And the thing they are putting in?”
“Yes, honey, I will always need medicine for my cancer. And I will probably need to have the port in forever too.”
Long silence.
“I am glad you are asking me questions about it. I want you to always ask me anything. I will try to explain everything to you. I know it’s complicated. It’s complicated even for grownups to understand.”
Long silence.
“Mom, did you know people whose eyes can’t see use the ridges on the sides of coins to tell which one they are holding? So if you have a big coin with ridges that person would know it is a quarter?”
“That makes sense. How did you learn that?”
“At school. And so if it’s smooth you know it’s a nickel or penny. It’s important that they know what coin it is.”
“I think you’re right. That is very clever.”
( I stay quiet waiting to see where he will take the conversation next.)
“Remember when my ear tube fell out and was trapped in my ear and the doctor pulled it out and I got to see it? It was smaller than I thought it would be.”
“Yes, I thought the same thing.”
“I really wanted to see it. I wanted to see what it looked like.”
“Me too.”
“Can you show me a picture of it?”
“Of what?”
“The thing for tomorrow.”
“The port?”
“Yes. Or don’t you know what it will look like?”
“I know what it will look like. Sure, I will show you on the computer after school.”
“Okay.”
“It’s time for school but I am glad we talked about this. I want you to keep asking questions when you don’t understand something. I love you, Tristan. I hope you know how much. I know this is hard for all of us. I wish it were different. But we are going to keep helping each other. And talking about all of this is good. We can do that whenever you want.”
October 15th, 2014 §
 From the time my oldest child, Paige, was born everyone kept telling me, “Just you wait.”
From the time my oldest child, Paige, was born everyone kept telling me, “Just you wait.”
When she made it through the terrible twos without much of a tantrum everyone kept telling me, “Just you wait.”
When she made it through elementary school and a move from NYC without trouble they kept saying, “Just you wait.”
“Just you wait,” they said, “girls are drama. You got lucky before. But the teen years? Oh boy… just you wait.”
Today she prepared me a bowl of soup and brought it up to my bedroom. I was resting after my surgery to remove malignant lymph nodes and tissue for testing yesterday, the room was dark. I invited her to come snuggle with me in the big bed. We’ve never let our children sleep in our bed so they think climbing in is a big treat.
I asked her if she wanted to talk about what was going on, about my news about having metastatic breast cancer. She did.
And so it began: an hour-long talk that started with her first question, “Are you scared?”
She asked questions about genetics and risks of getting cancer to what kind of treatments I might need.
She asked me again, as if to confirm for herself, “It’s not curable, right?”
We talked about my writing, about being public with my health status, about being open and honest with her and her brothers.
I told her that yes, I was scared. I explained that my fear usually comes from the unknown, in this case just how I will respond to treatments. I told her it was okay to be scared. That it’s normal, that sometimes fear makes you brave enough to do things you don’t think you can otherwise do.
I told her that I understood that sickness could be scary, that I didn’t want her to be afraid of me as I got sicker someday. “I would never be afraid of you, Mom. I’m only afraid of cancer,” she said. My heart squeezed and thrashed and the tears flowed.
We talked about her desire to be a doctor, a surgeon. She wanted to know what all of my surgeries and treatments had done. She wanted to know the difference between cancer “stage” and “grade.” We talked about the genetics of breast cancer and discussed the BRCA-1 and 2 genes (which I do not have). We talked about hormones and their role in puberty, menopause, and cancer. She wanted to know why outcomes are so variable. How will we know if treatments are working? I told her about the importance of her monitoring her own health, how hopefully we will have better screenings down the road.
I told her that for now I want her to live her life, for our house to be as normal as it can be for as long as it can be.
I told her she should try to focus on her schoolwork, her sports, and her friends. She told me that I was more important.
I told her that eventually I might need someone to help take care of me. “I will take care of you, Mom. You’ve always taken care of us,” she said.
We talked about her brothers, ages 11 and 6 and how she was going to have to help them. And her dad too. “I’m really good with hospitals and medical things, Mom… I’m just like you.”
She said she liked that I was open about it. That people knew. She thought it was best to be honest and appreciated the offers of support she’d received from friends and adults she knows.
I told her that what we were doing, lying there talking for an hour together about this, was the most important thing we could be doing today. I told her there wasn’t anything more important to me than my family. My job is to help them deal with this. Whatever this is.
I explained that what she needed from me would likely differ from what her brothers need; she is older and each of them would have different needs along the way. It’s my job to figure that out and address it. And my husband’s job now, too. How I take the lead on this will be important.
She asked if that was a lot of pressure, to have so many people reading my words, watching what I was doing. I told her it was. I told her it was my way of trying to help people. The same way that she wants to be a doctor to help others… well, I have always tried to see if I could help in my own way. And the way we talked before about the unknown being what’s scary? Well, my writing here means it’s less mysterious. Knowledge helps. Even if the knowledge is not what you want to hear, knowing is better.
Denial won’t change the course of things, and often makes things worse.
Secrecy is bad. Sharing and supporting are what I champion. And I know that de-mystification is a constant effort. I will continue to teach my children daily. I said I hoped that somewhere in all of this she could see how important science and medicine are in my world. And that if she does decide to be a doctor that is a noble effort. She will make me proud in whatever she does. As will my boys.
The funny thing is how much better I felt after we talked. The conversation was the hardest one I’ve had. The topics are gut-wrenching. But shining the light on them, on this disease, on what happens next, is the only way I know to cope, to help, to keep going.
We talked on and on as I combed my fingers through her long hair. I stroked her smooth, soft cheek. She was giving me strength.
And what I realized about people saying I should just wait because she’s going to eventually act out:
Waiting is a luxury.
Waiting means having time.
And that’s what I want most in this world right now.
October 6th, 2014 §
 One of the most common questions I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a practical gift for someone who has just been diagnosed and it is a necessity if you are the patient or a caregiver.
One of the most common questions I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a practical gift for someone who has just been diagnosed and it is a necessity if you are the patient or a caregiver.
Being organized is one of the best ways to help yourself once you’ve been diagnosed. When you first hear the words, “You have cancer” your head starts to swim. Everything gets foggy, you have to keep convincing yourself it’s true.
But almost immediately decisions need to be made — decisions about doctors, treatments, and surgeries. Often these choices must be made under time constraints. You may be seeing many different doctors for consultations. Medical oncologists, surgical oncologists, radiation oncologists, recontructive surgeons, internists— there are many different voices that you may hear, and they may be conflicting. It’s hard to keep it all straight in the midst of the emotional news. Not only are you likely to be scared, but also you are suddenly thrust into a world with a whole new vocabulary. By the time you are done with it, you will feel you have mastered a second language.
You can help your care and treatment by being organized. You can also have the psychological bonus of feeling that one part of your care is within your control. Especially if you are juggling different specialists and different medical facilities, you must remember that the common factor in all of this is you. It’s your health. It’s your life. I believe it’s important to travel with a binder of information about your medical history and treatment, as well as notes and questions.
This binder will mean that all of your information about your cancer will be in one place. This will be your resource guide. I cannot tell you how many times physicians have asked about my binder and when I was able to instantly produce test results, pathology reports, or other information they needed, they said, “I wish every patient had one of those.”
I suggest the following:
A heavy 3-ring binder
I think a 1.5″ binder is a good size to start. This size will allow you to easily access reports and pages and have room for the calendar. It will look big at first but you won’t believe how quickly you will fill it up.
Colored tab dividers
I like these to be erasable. I think 8 is the minimum number you will need. If you have a lot of specialists you will need more. The categories you think you will need at the outset may change. It’s easy to erase and reorganize them. Put the categories you will be accessing the most in the front so you aren’t always having to flip to the back. Once the binder is full it will make a difference.
Some starting categories:
- schedules (dates of appointments you have had, when the next ones are due, and how often you need certain tests done)
- test results/pathology (it’s very important to keep copies of MRI, CT, and pathology reports so that you correctly tell other doctors what your diagnosis is. For example, new patients often confuse “grade” with “stage” of cancer)
- insurance (keep copies of all correspondence, denial of claims, appeal letters, explanations of benefits)
- articles and research (handouts, post-surgical information. Ask if there are any websites your doctor does approve of. My own oncologist said, “Do not read anything about cancer on the internet unless it comes from a source I’ve told you is okay. There’s a lot of misinformation out there.”) Keep your post-surgical instructions, any info given to you about aftercare.
- radiation/chemo (keep records of exactly what you had done, number of sessions, dates, drug names, etc. I also asked how my dose was calculated so I knew exactly how much of each drug I received in total)
- medications (drug names, dates you took them, dosage, side effects). I also keep a list of all of my current medications as a “note” in my iPhone. That way I can just copy it down and won’t forget anything on the list. You should always include any vitamins or supplements you take.
- medical history (write out your own medical history and keep it handy so that when you fill out forms asking for the information you won’t forget anything. As part of it, include any relatives that had cancer. Write out what type it was, how old they were at death, and their cause of death. Also in this section include genetic test results, if relevant)
Loose leaf paper
Perfect for note-taking at appointments, jotting down questions you have for each doctor. You can file them in the appropriate category so when you arrive at a doctor your questions are all in one place.
Business card pages
These are one of my best ideas. At every doctor’s office, ask for a business card.Keep a card from every doctor you visit even if you ultimately decide not to return to them. If you have had any consultation or bloodwork there, you should have a card. That way, you will always have contact information when filling out forms at each doctor’s office. For hospitals, get cards from the radiology department and medical records department so if you need to contact them you will have it. Also, you want contact information for all pathology departments that have seen slides from any biopsy you have had. You may need to contact them to have your slides sent out for a second opinion.
This is also a good place to keep your appointment reminder cards.
CD holders
At CT, MRI or other imaging tests, ask them to burn a CD for your records. Hospitals are used to making copies for patients these days and often don’t charge for it. Keep one copy for yourself of each test that you do not give away. If you need a copy to bring to a physician, get an extra made, don’t give yours up. If you need to get it from medical records from the hospital, do that. You want to know you always have a copy of these images.
Keep a copy of most recent bloodwork (especially during chemo), operative notes from your surgeries (you usually have to ask for these), pathology reports, and radiology reports of interpretations of any test (MRI, CT, mammogram, etc.) you may have had. Pathology reports are vital.
Calendar
I suggest a 3-hole calendar to keep in your binder. This will serve not only to keep all of your appointments in one place but also allow you to put reminders of when you need to have follow-up visits. Sometimes doctor’s offices do not have their schedules set 3, 6, or 12 months in advance. You can put a reminder notice to yourself in the appropriate month to call ahead to check/schedule the appointment. Some people like me prefer to use their phones for this, including reminders.
Similarly you can document when you had certain tests (mammograms, bone density, bloodwork) so you will have the date available. I usually keep a piece of lined paper in the “scheduling” section of my binder that lists by month and year every test/appointment that is due and also every test I’ve had and when I had it.
Sticky note tabs
These can be used to easily identify important papers that you will refer to often, including diagnosis and pathology. These stick on the side of the page and can be removed easily. As your binder fills up, they can be very helpful to identify your most recent bloodwork, for example.
Plastic folder sleeves and sheet protectors
These are clear plastic sleeves that you access from the top. They can be useful for storing prescriptions or small notes that your doctor may give you. The sleeves make them easy to see/find and you won’t lose the small slips of paper. Also a good place to store any lab orders that might be given to you ahead of time.
The above suggestions are a good working start to being organized during your cancer treatment. If you want to do something for a friend who is newly diagnosed, go out and buy the supplies, organize the binder and give it to your friend. He or she will most likely appreciate being given a ready-made tool to use in the difficult days ahead.
I also believe a modified version is equally useful for diagnoses other than cancer. When our youngest son was born with defects in his spine and hands it took many specialists and lots of tests to get a correct diagnosis. Having all of his tests and papers in a binder like this was instrumental in keeping his care coordinated. In fact, at his first surgery at The Children’s Hospital of Pennsylvania they gave us a binder to assist in this process. I know some hospitals do this for newly diagnosed patients already.
Maybe my tips will help you or a friend know how to better use the one you already have. You may not need all of these elements depending on the complexity of your case, but I hope you will find some of these suggestions useful.
July 9th, 2014 §
 Now that all three of our children are at sleep away camp I get asked a lot “what I’m doing with all of my free time” and “what fun things I have planned.” Clearly what people think life is like for me are a bit skewed. I have nothing planned. I can’t travel and haven’t been able to take a trip for over a year. I’ve missed family celebrations, holidays, and get-togethers. I’ve eschewed visits from family and friends because I’m not well enough. What others consider “free time” is recovery from chemotherapy and struggling to do day-to-day functioning including the many medical appointments. Being able to make it out for a coffee date is a thrill and isn’t possible many days. Most of the rest of the time my “free time” is spent in bed fighting nausea or fatigue or pain or other side effects.
Now that all three of our children are at sleep away camp I get asked a lot “what I’m doing with all of my free time” and “what fun things I have planned.” Clearly what people think life is like for me are a bit skewed. I have nothing planned. I can’t travel and haven’t been able to take a trip for over a year. I’ve missed family celebrations, holidays, and get-togethers. I’ve eschewed visits from family and friends because I’m not well enough. What others consider “free time” is recovery from chemotherapy and struggling to do day-to-day functioning including the many medical appointments. Being able to make it out for a coffee date is a thrill and isn’t possible many days. Most of the rest of the time my “free time” is spent in bed fighting nausea or fatigue or pain or other side effects.
For the last few weeks my blood counts were sliding and I couldn’t do anything without huffing and puffing in a much more severe way than usual. I struggled to bend over to pick something off the floor without needing to sit down to catch my breath. My hemoglobin levels had been hovering around 8.2 for months and I pushed through but they dropped to 7.2 and by then it seemed I needed a boost to be functional. Ten days ago I received two units of red cells in a transfusion that because of some problems with the samples and testing and a five hour infusion ended up being a ten hour marathon day. It was so worth it. Red counts came up within days and I felt better starting about 24 hours after receiving the cells and that continued to increase within two to three days. My platelets were also very low at 24 but regenerated on their own (low platelets are a predictable result of this chemo regimen) and I was able to avoid a transfusion of those. This was, by the way, the first time I had ever had a blood transfusion in my life.
I had chemo yesterday: Carboplatin and Gemzar cycle #6 (that means I’ve had 6 infusions of Carboplatin and 11 of Gemzar so far). Starting now, but especially with cycle 7 and every time after that, there is a risk (reported at 27% for round 7, here is an article for anyone interested) of an anaphylactic reaction to the Carboplatin (and the other platinum-based chemotherapies like it). We are being conservative and premedicating with drugs that will hopefully help blunt or avoid this type of reaction altogether. There isn’t any reliable way to predict if it will happen to any individual patient. I did have a reaction to Taxol when I received it in the metastatic setting (after not having a reaction the first time I had 4 cycles of it seven years ago) but that is not a reliable indicator of a reaction to platinum-baed drugs.
It will be time for a scan soon I think, we are watching my tumor markers which have dropped consistently in the last few months which is fantastic but on yesterday’s test just stabilized without a drop. We’ll have to see if this is just stabilization (fine) or if this is the start of the chemo losing its effect. It is unsettling to think about losing another chemo combination that has been working, even though it’s a tough regimen to tolerate.
My voice has returned to almost normal unless I use it on the phone or talk a lot. With the kids gone I really am not talking much. I had an extra five days off chemo because my oncologist was on vacation and that allowed me to get things done I usually don’t have enough rebound time to do. The transfusion timing helped too.
 I haven’t been outside much, the humidity and heat have been too oppressive for me, but I am hopeful it will break soon. I do try to make it to the beach once a week to get a change of scenery.
I haven’t been outside much, the humidity and heat have been too oppressive for me, but I am hopeful it will break soon. I do try to make it to the beach once a week to get a change of scenery.
We will get to see the kids this weekend and I can’t wait to hug them and hear all of their stories before they go back. They love camp, always have. They look forward to it year-round and now that they all go it’s great they can share these stories and experiences (they are 15, 12, and 8. Last year the youngest begged to go for a week to try it out. We said yes, knowing his siblings would be there and he would have a blast. Five days in he called in tears, begging to stay. That repeated every week until after a month we said it was time to come home!).
Some may wonder why, at this time, I let them go instead of keeping them home with me. I do it because it’s not about me. It’s about them. It’s something they love. It’s an important routine, tradition (this is the sixth year for the oldest). In my eyes, it’s important that they have a change of scenery, freedom to be kids, get away from the ways my cancer and its chronic treatment limit what I can do, and therefore what they can do. It’s a gift I can give them and I also feel it reassures them that I am doing better than I was a few months ago. This is important.
 I love having them away from electronics, away from wondering if asking me to take them somewhere or do something with them will be “too much” or “bothering me” which I know the older ones are always concerned with. I want them to be with friends old and new, having fun with young and energetic counselors, trying new things. There are so many (most/all) physical activities I cannot do with them that they can do there. So many new games to play, achievements, laughs, experiences. I never hesitated when they were ready to sign up last October for this summer. I knew that no matter what, they needed and deserved it. On the left is my favorite photo from camp so far: Tristan getting hooked in to try rock wall climbing for the first time. It makes me laugh every time I look at that facial expression!
I love having them away from electronics, away from wondering if asking me to take them somewhere or do something with them will be “too much” or “bothering me” which I know the older ones are always concerned with. I want them to be with friends old and new, having fun with young and energetic counselors, trying new things. There are so many (most/all) physical activities I cannot do with them that they can do there. So many new games to play, achievements, laughs, experiences. I never hesitated when they were ready to sign up last October for this summer. I knew that no matter what, they needed and deserved it. On the left is my favorite photo from camp so far: Tristan getting hooked in to try rock wall climbing for the first time. It makes me laugh every time I look at that facial expression!
That doesn’t mean it’s easy for us to be apart. We are very close. Especially the older kids worry about me I am sure. But I stay in touch by email, will see them on visiting days, and I send them weekly care packages.
But the truth is that separation is good. It’s a selfless act for me to teach them how to to be without me. One of the most important things, in my mind. Coddling them and making them stay home is not what I feel is best for them right now. It is part of our job as parents to teach our children how to be independent, how to solve problems on their own, how to go off in the world without us for whatever reason. I will always want more time with them. It will never be enough for me. But this is my old age. I must teach them as many lessons as I can, while I can, for as long as I can. And that is true for everyone, but of course I have not only the urgency to do it NOW but also I have no idea how long I have and will likely be debilitated in some form until that time comes.
Yes, it’s true no one knows how long they have to live. But those diagnosed with a terminal disease know what is most likely to kill them. And that their time is not just going to be shortened, but consumed daily with the treatment and effects of that disease. It’s not having a normal, healthy life that is relatively good and healthy until a sudden accident happens. It’s just not the same as the general worries of growing older or aches and pains. It’s never-ending. I don’t get to count down how many chemotherapy (or other treatment) sessions until I’m done this time. Being done will mean there is nothing left for me to try. Anyone who has had chemo or radiation or some other type of therapy knows how important it is to have an endpoint, a countdown. Knowing that will never happen (and in fact what you’re really hoping for is a lot of them, because that means you still have options) is one of the mental struggles each week, since it isn’t just spending one day a week getting chemo, it’s how it makes you feel each day after that.
My hair is growing slowly back on this current combo. I know many people mistakenly think this means I’m “better.” I do like that soon I won’t be covering my head and that means I can be more invisible in public. But I also know how many comments I get on the occasions I have done it that people think I am done with chemo or all better. Not all chemotherapies cause hair to come out. My hair will come and go numerous times by the time we are done with this. Its presence or absence only indicates something about which chemo I’m on, not its success or failure.
Someone on Twitter asked for my piece on what to say and how to be a friend to someone who has cancer/serious illness. Here is a link for anyone that missed it and is interested (it’s too long to include the text in this post).
Also, I am including two posts from last year at this time. One on the eve of the kids’ departure for camp and one written while they were away. Of course I was doing even better than I am now, my thoughts were similar, but not as urgent, strong, painful as they have been the last seven months.
I’ll post again with an update if there is anything to report on change in treatment, scan results, etc. For now we stay the course which is not easy, but is the best possible choice of the options I have right now. And that’s the best I can do.
I appreciate the support, as always!
…………………………………………….
In these last remaining hours (Camp) original post here
In these last remaining hours
Before my children disappear
One,
Two,
Three…
In these last remaining hours before they go and spread their wings again,
Leave this nest,
I miss them already.
I put the dinner pots and pans away.
Wipe the crumbs from the table,
Load the dishwasher,
Play fetch with the dog.
I sit in the garden,
Listen to the wind in the trees,
The birds settling down before nightfall,
As we settle, too.
I tuck them in one last time,
Hear their doors click shut.
One,
Two,
Three.
Tomorrow night there will be no mess to clean,
No yelling upstairs that the TV has been left on again,
No trunks piled high with carefully labeled belongings in the dining room.
I will cry, I know.
Not because I am sad that they are going– no, that gives me great joy.
Children being children.
Forgetting stress at home and doing new and varied things.
I cheer their independence.
I will cry because I know they will always need me somehow and I just wish I could be there for them to outgrow
by choice,
by time,
by age.
I hear the mother bird in the tree calling out.
I don’t know to whom.
I will be like that tomorrow,
calling out,
with no child to hear.
……………………………………………………….
Like dollhouse rooms left abandoned (original post here)
Like dollhouse rooms left abandoned,
The rooms stay tidy:
Beds made tight,
Pillows square,
Hampers empty.
It’s been one week since the children left for camp.
Littlest Tristan was due back yesterday but a few days ago he said he was having so much fun he wanted to stay another week.
I realized this week that after being sick for the previous two that I needed this time to catch up, to rest, to regroup.
I miss them but am so glad they are having fun doing what they love.
I pack up care packages,
write letters,
wake in the middle of the night and mentally picture our children sleeping in cabin beds.
Our dog Lucy follows me, sleeps in my room now, not Paige’s.
She doesn’t want to be alone and stays within feet of me every moment.
I tell her it’s okay:
The kids will come back.
The rooms will get messy again.
There will be crumbs dropped at the dinner table and car rides galore.
Paige and Colin and Tristan will come back tired and dirty and happy.
They will come back.
They will.
That is the key.
I think of absence like a hole:
How different it is when it’s temporary and filled with happiness,
Rather than when that hole is a pit of grief. Of ache. Of loss.
The way it will someday be for them.
March 4th, 2014 §
 Hi everyone, an update to briefly say hello since my posts are still infrequent. It’s been about three months now since this particular acute metastatic breast cancer episode started. First I was stuck at home in pain with tumors in my spine and hips before and during the holidays. Then I was in the hospital for three weeks at the start of 2014 getting pain under control and having two weeks of radiation. Now I’ve been home for another six weeks since leaving the hospital.
Hi everyone, an update to briefly say hello since my posts are still infrequent. It’s been about three months now since this particular acute metastatic breast cancer episode started. First I was stuck at home in pain with tumors in my spine and hips before and during the holidays. Then I was in the hospital for three weeks at the start of 2014 getting pain under control and having two weeks of radiation. Now I’ve been home for another six weeks since leaving the hospital.
After such a long period of time many people will start to assume you “must be back to normal by now.” Each day they anxiously wait for news that someone “feels better.” It doesn’t work like that all the time, just the way with metastatic cancer you don’t “beat it.” A good day or two may come, but they are often followed by a bad one, or two, or three. Add chemo to the mix and you start to realize the good days are relative and elusive in incurable cancer. Support is always so appreciated as the days, weeks, months go by. It’s friendship for the duration.
There are many situations where isolation may be a real danger including examples of infertility, chronic illness, and grief. Those who must deal with these problems start to feel isolated. Additionally, they may start to actively separate from others when they feel that life is just moving on without them. As time goes on, they may hesitate to talk about their problems because they fear that friends will have grown weary of hearing about it/ still can’t relate to it. More and more, they keep these things to themselves. This leads both to further isolation and also the faulty notion from their friends that the person is “over it.”
The truth is that it’s very hard when difficult situations of all kinds linger. I think we all do better when tough times are brief. Being in one of these situations has shown me the depth to which this is the case.
Today I had to miss Tristan’s Spring music show at school. It broke my heart to tell him I couldn’t attend. They were able to videotape it and I know we will watch it together and have a special time doing that. If it were just one thing it would be different. But as any parent can imagine, saying, “I’m so sorry but I can’t…” again and again for months is difficult. The truth is that if I knew it were temporary it would be easier. But I know that there will be more and more things I can’t do with the kids. And that’s what weighs on me: this thing is part of a whole.
I tried driving last weekend but unfortunately, for now, the verdict is that I am still unable to do more than go to the bus stop at the end of the street if needed. So I continue to be housebound.
I’m working with my doctors to adjust my medications and try to manage the vertigo, sedation and pain. I am using less pain medicine (hooray) but unfortunately I still feel so rotten I sometimes can’t get out of bed and most often can’t go anywhere except to chemo. It is a cruel balance. This weekend I was stuck in bed for three days. It saddens me to lose so much time.
I still long to write here more. I miss the creative part of my brain working the way it used to. I miss poetry and photography and so many things. I will bring them back though! The orchid photo above is one I took in the kitchen this week. My friend Alex brought me lunch and a beautiful potted orchid. I even ordered daffodils with my groceries this week to remind myself of the garden outside and what’s waiting under this snow.
Winter break at school came and went. I know it’s a very busy time for everyone as Spring approaches. It’s hard to see life outside passing me by while I wait for Spring so I can at least get fresh air here at home. It has continued to be cold and wintery over the past few weeks. If you’re able to be outside today doing anything: errands, standing at the bus stop, or waiting the train platform on your way to work: think for a moment what it would feel like not to do any of that for three months. It’s a very long time. Mundane things can be sweet when viewed in a different light.
I am so grateful for the offers of help and meals that continue to come. Let me assure you they are so needed and appreciated. I will have chemo again this week. In two weeks’ time the plan is to do scans to see if there is any visible evidence about whether radiation and chemo have shrunk the cancer.
My daily reminder: Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
In case you need a bit of beauty I will leave you with one of mine, a good laugh this week from Tristan. With a very serious expression on his face he says to me quietly from the dinner table, “Mom, I have something to tell you and you’re not going to like it. It’s something I learned. I was reading it in a book. But I think you will be upset. The book was about Albert Einstein. It said that for a while he didn’t want to go to school. He didn’t want to learn things in school that they wanted him to learn. He just wanted to learn what he wanted to learn. He stayed home for a while and didn’t go to school. See? I think you would not think that was very good that Albert Einstein didn’t want to go to school.”
February 23rd, 2014 §
 Sunday morning.
Sunday morning.
A different kind of strength: shave the few soft but strong hairs that are finally ready.
Now gone to the floor.
No tears.
Necessity.
……….
You’ll be seeing more posts here in the near future about some of my feelings over the last two months. I’m starting to feel more like myself. The vertigo is lessening with the decrease I’ve been able to make in the pain medication, as we’d hoped. I’ve reduced the pain meds by 20% and the hope is that as the radiation effects start to kick in I will be able to decrease more. It’s been five weeks now since I finished radiation. I needed these Fentanyl patches desperately while the tumors were out of control. I could not have done it any other way. But certainly we all want me only using the amount I need to control my current level of pain.
I will be going back to meet again with my palliative care doctors this week to reassess my pain meds and talk about the plan for the next few weeks. I was thrilled to see that my last post about the importance of early palliative care and its definition (not end-of-life pain management… but instead total patient care pain management) was so well-received by patients and doctors alike. I encourage both sides to really form a team and focus on all side effects that patients are having with all kinds of treatment.
Patients function better not only emotionally but also physically in that they will heal better if their bodies are not weakened by pain. It takes trial and error to find the right drugs and the right amounts. It takes patience. Most palliative care doctors are experts in patience, I have fortunately found. I know that is not always the case and I always receive emails and comments from people who have had distressing experiences with their care. I am so sorry for that. I am hoping by relaying my own experiences, readers who have not yet found help with pain will have strength to ask again or pursue help if they’ve been unable to.
I’ve started my second month of chemotherapy (Taxol). I do three weekly treatments in a row and then have one week off each month. I had my first infusion of my second month on Thursday. I haven’t had any additional reactions to the chemo so I’ve been able to have the sessions done rather quickly (30 minutes for the 3 pre-medications and then 60 minutes for the actual Taxol). Sometimes I go alone and sometimes I have a friend join me. I am developing a routine and it has worked well so far.
 We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
For today I’m sporting a head scarf and getting used to seeing a new reflection looking back at me in the mirror.
………
Make the most of this day. Whatever that means to you, whatever you can do. No matter how small it seems to you. Don’t waste it.
February 7th, 2014 §
 It’s hard to believe how many days went by when I was in the hospital. It’s hard to believe how many days have gone by since I’ve been home.
It’s hard to believe how many days went by when I was in the hospital. It’s hard to believe how many days have gone by since I’ve been home.
I have wanted to write a blogpost so often. I sat down at the computer many times in the last few weeks to update you on what has been going on.
Most often what happened when I did that is simple: I got very tired and fell asleep. Sometimes my vertigo was really distracting. Sometimes the distraction was something wonderful: one of the kids wanted to tell me something. Frequently it was Tristan in his little voice saying, “I love you, Mama.” That one always takes priority, of course.
I’m on a lot of pain medication at the moment. I have been since leaving the hospital almost three weeks ago. The positive effects of radiation haven’t quite kicked in yet. I still have many of the negative effects of radiation. These will go away soon. But right now I’m still waiting. This is totally normal for radiation that is used in the way I used it, I should point out; it takes weeks, and in fact months, for the positive benefits of radiation to be fully realized. During that time the negative side effects of radiation can linger.
They radiated my spine in the T9/T10 areas from both the front and back and also radiated my pelvis through from the left and right sides for ten sessions over two weeks. The side effects that I have are related to the particular lines of radiation and what areas the beams hit while also hitting their targets. For me, esophagus, stomach, intestines, colon, pelvis, sacrum, and spine were the main areas hit. Esophagitis which makes eating and drinking painful is starting to decrease (but the raspy voice continues). Problems with digestion continue. Lowered blood counts continue. Pain and inflammation in nerves and tumor sites continue. Heartburn and colitis have decreased. I do not have radiation burns right now and they really didn’t get too bad over the course of those two weeks, just some sensitive pinkish/brownish areas.
The pain that was so debilitating is finally under control with pain patches. It takes quite a high dose to keep it managed right now but we will try decreasing this amount as the weeks go on. I will meet with the palliative care team in a few weeks to talk through a strategy for the reduction. The team is always available by phone for any fine tuning or questions that I have until that time.
Again I’d like to remind readers that palliative care is not synonymous with end-of-life care. Palliative care is for pain management and side effect management at any point of treatment for cancer or other diseases. If you have pain or other problems that are bothering you or a loved one, I encourage you to talk to the specialists in palliative care. They will be able to help.
Patients and their families often wait too long to consult with these specialists because they think talking to them implies something about death. It does not. In fact, if you wait too long (until the very end of life) the palliative team will probably be less likely to fully help you or your loved one because they won’t know how the patient responds to different medications, what their side effects are, what doses they respond to, etc. Palliative care doctors can help better if they know the patient and their particular side effect profile. I implore you to use them sooner rather than later. Time and again, studies have shown that healing occurs better when patients are not in pain.
We aren’t quite sure where it’s coming from, but my vertigo is quite the problem right now. We know it is from one of my medications, presumably the pain one. Of course for now I still need to make my pain medication the priority. As I said earlier, as soon as I can, I’ll be decreasing that dose. We know from a scan a few weeks ago that I do not have any metastases in my brain causing the vertigo. Of course that was a natural concern and it’s nice to have that possibility off the list. I still can’t drive because of the vertigo. So I’ve been housebound for the three weeks I’ve been home. Before that I was in the hospital for almost three weeks. I don’t have cabin fever too much because of the bad weather we have been having. But I’m probably getting close.
I’m still trying to figure things out. I’m still adjusting to the new information about the tumors and the progression that’s been happening in my body over the last few months. I’m learning about the genomic mutations that are present in the metastases and what they mean for future chemotherapy and clinical trial choices. I did not start the clinical trial I was planning to, obviously. Instead, we needed to do more aggressive and surefire treatments rather than investigational. Therefore, I did the radiation and then started chemotherapy 5 days after the completion of radiation (a bit of a fast track but I felt up for it and my bloodwork and exams indicated to my oncologist that I was ready).
I started chemotherapy two and a half weeks ago. I’ve had three infusions so far of Taxol. This is an intravenous chemotherapy that works on rapidly dividing cells of all kinds. One ramification of that action is that it will make my hair, eyebrows, and lashes come out in the next few weeks. I received it in a different regimen six years ago as many people do with early stage breast cancer following the use of Adriamycin and Cytoxan on a dose-dense schedule (every 2 weeks). It’s a popular drug.
The way it’s used now in the metastatic setting is different in terms of dose and frequency of infusions. In the metastatic setting there are different doses that are used. I’m using the highest right now. It is done in a “three weeks on, one week off” schedule. That means I get it once a week for three weeks and then I get a one week break. Though I never had a bad reaction to it in 2007, I did have a reaction to the drug the first time I got it a few weeks ago. I won’t go into the details of it here. I’ll just say that with increased amounts of steroids as pre-meds I’ve done just fine with the Taxol since that first episode.
For now I’ll close by saying I’m grateful for the friends that have been lending a hand with rides and playdates and meals while I’ve been housebound and unable to drive. I’m thankful for all of my readers who have been checking in on me and waiting patiently for this update. I am so happy to see so many new blog readers and Twitter followers in the past few weeks!
I want to give special recognition to all of the doctors, nurses, aides, therapists, and everyone else I came in contact with at Sloan-Kettering while I was hospitalized. Yes, there are always ways to improve, but I can truly say that I felt fortunate to be in such a caring environment for those weeks. I never doubted that it was the right place and that everyone there had my health and overall well-being first and foremost in their minds. It was always a team effort and for those of you who helped me in every way, I thank you. The fact that I miss so many of the you who cared for me shows that you made an impression on me.
The blogposts will return to a mix of updates, practical advice, and poetry as the weeks go on and I feel more and more like myself. Most posts will be shorter than this one but I know most of you have been wondering how I am and what I’ve been up to. I think this brings you up to date.
*Please note that I do not need suggestions for my side effects. I haven’t gone into the details here of what I’m taking, but I do have what I need from my team. Thank you!
Find a bit of beauty in the world. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
January 9th, 2014 §
No matter where you are
There is always beauty in the delicate unfurling of the morning as
It and its inhabitants come to life for the day.
A chair scrapes on the floor upstairs,
An electric bed adjusts,
An IV pump sounds,
A shade gets lifted to see the twinkling city.
A soft voice enters the room,
Two pills in a plastic cup down the hatch without disturbing a keystroke.
Vital signs are taken, the velcro cuff rips.
Vials of blood from my port,
The soft tapping of the tubes as the tech manipulates them deftly in one hand to keep refilling constant.
An IV pole whines like a morning toddler standing in her crib, anxious for first attention of the day.
Toilets flush,
Breakfast orders placed.
Young doctors starts to trickle in to find out how each patient’s night went.
And then some of the real business of the day starts.
Decisions made each day about life and death.
Who has surgery today,
Or a chemo change,
A transplant,
Biopsy.
Some will go home, some will not be ready.
News will be given.
Each person has a life unfolding here today. But remember it is a life.
Not a diagnosis, not a body part.
But just as the tide goes in and out,
Gives and takes,
So does metastatic breast cancer.
It progresses, taking more,
You hopefully have an arrows left in the quiver to try.
You tame it back and do the dance again. And again.
Leapfrog through treatments trying to stay one step ahead.
There is always adjustment.
It is a shifting target. You’d best be on your toes.
I am at the beginning of what treatments are available for me.
Don’t you count me out yet. Far from it.
Just because this disease can’t be cured doesn’t mean there isn’t a lot of life left in me; there is still so much for me to do.
I am living with cancer.
I want to count the days until I can be home and me again. But we do not know exactly how many are left. Getting closer I hope.
When I get back home it will be a different me, but that is not the point.
This is part of metastatic breast cancer and now I’ve had my first introduction.
It’s been 15 months since I received my diagnosis.
This is the first time I’m needing any type of radiation.
I will have to pull out some more aggressive weapons in chemotherapy options.
 But as I’ve done each time, my oncologist and I will research and discuss.
But as I’ve done each time, my oncologist and I will research and discuss.
She and I took this photo last night in my room as we talked about what the treatment plan will be for this week to get me out of the hospital. Once we have a short term plan then we will know what the next few months will look like. There is defiance in setting out on a new path.
The first step should be a confident one, not a toe dip into the shallow end.
For now the hospital is where I need to be as we finish evaluating exactly where the cancer is how to best target it. Additionally, we are still are fine-tuning pain control via the pump. It is a process to convert from using IV pain medication (rapid and adjustable help) to oral ones. The excruciating pain that comes from the tumors in my hips and spine demands serious pain management until we can allow time for the effects of radiation and chemo to settle in. That’s been a main focus. The pain will get worse before it gets better in those spots it seems. Radiation pain will precede improvement in many cases like mine.
The discovery in the past two weeks of more metastases was a curveball. But it’s standard practice for metastatic breast cancer. Totally typical.
I have quickly come to care for the people who work on the floor. There is so much care and assistance and tenderness every day. I look forward to sharing some of those stories in the weeks and months ahead. I could not be more grateful for the daily affection mixed in seamlessly with medical care.
Each room has a story.
My room has smiles and laughs and love. It has tears and anger and bewilderment. It has every part of life.
As I attack the cancer cells in my body I must always search for ways to bridge to the outside world. My family and friends have made that easy. They are my heart and soul. The supporters I have online help so much too. Your words of compassion and care keep me going and remind me why what I’m doing is so important. Using the time I have now while I am able to be functional is precisely the point… continue to give those too weak or unable to share the true experience of daily life with this disease a voice. To teach, to enlighten, to share, to support, to fundraise for research… and to always honor those who have died.
As always I could not do any of this without my oncologist Dr. Chau Dang. I love this photo we took last night in my room.
There’s always so much more to say. But I’ve got some time to do that.
So for now, my dad is here for a visit and I’m going to go have a cup of coffee with him… thanks again for the support I receive from so many of you. You know how much I treasure it: it’s my beauty.
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
January 8th, 2014 §
 I add another ball of surgical tape to the back of the photograph of my family hanging at foot of my bed.
I add another ball of surgical tape to the back of the photograph of my family hanging at foot of my bed.
Don’t fall.
Stay there.
Just stay.
Together.
…………………….
I wake up fettered, chained, restrained in body and mind.
The room is cold and yet it stifles:
Choking, pulling, grabbing me back, reeling me in.
I start to shake, fear manifest in movement,
Waiting for Reality,
The next interloper…
Another who will not be pushed away,
Ignored,
Wished or willed or
Bargained for.
I search for powers to rise above, get out, fly away.
Those dreams cannot escape that reality.
That shaking cannot stop.
When repeatedly pushing the button of narcotics is an act of acceptance,
A realization of what is,
In part an impotent attempt to eject myself from the room, the bed, my body.
The tears which accompany my pathetic try stay safely tucked away,
Hiding with hope and mental acuity and certainty.
Like middle school children the fear starts to divide, partners off, chooses a companion for the evening.
Two by two, hands on hips, turning tightly into a circle
Guarding spots of possession,
Declaring ownership,
This is mine.
The fetters must remain and yet I will not budge.
I have my spot.
Small perhaps,
But it is still mine.
I have my life.
I watch it shrink.
I have my words.
But now I see them dissolve around the edges
Like watercolors they bleed as they search for pristine lands to conquer
As they stretch that lifeline.
The words of disease become words my brain gravitates to.
The ebb and flow of cancer,
Of life.
And so too,
Inevitably,
Of death.
Each night when I return to my room after radiation now it happens:
My voice instantly is quiet, reverent.
I am resepectful of what I ask that beam to do,
I ponder the magnitude of something I cannot see.
And so I affix that photograph, one more piece of tape just in case.
Holding on to all that matters,
Doing as much as I can for as long as I can.
Day by day,
Storing up bits of beauty wherever I can find them.
January 6th, 2014 §
 The last weeks have not gone as planned.
The last weeks have not gone as planned.
I had the liver biopsy and PleurX drain put in my left lung on 12/31/2013. I was going to only stay one night for observation and to try to address the pain that I was having. Further tests revealed more information. The pain that we thought was coming from my lung and spine wasn’t just coming from my lung and spine. In fact I have some tumors in my bones in the left hemisacrum and right femur too. The spine tumors are now in more vertebrae than we’d thought.
I’ve actually been in the hospital for 6 days now trying to get the pain under control and formulating a treatment plan with my team. I will need to be here for a while longer. I am starting 10 sessions of radiation later tonight after being mapped this morning. We had hoped to do it in five sessions but for reasons I can’t go into now they have decided this is a better route and will be more effective for the future.
This treatment will stop the current progression of pain, but the way this radiation works for me is that it won’t provide true pain resolution for probably about 2 weeks and then improve further over the next few months. The pain reduction will be cumulative and take a while (long after the radiation is actually over) to see final resolution in my case. I’ll have to deal with this for a while yet.
The side effects because of where they are targeting the beams in my spine will be irritated esophagus, trouble swallowing, nausea, vomiting, and heartburn. The other radiation site in my hips will potentially cause decreased blood counts, pain, irritation, gastrointestinal pain and dysfunction and the like.
My pain is still not under control and I’m on a Fentanyl pump system that allows me to dispense medication as needed in accordance with the pain levels. I will convert over to oral medication and patches when it’s time for me to go home once we can figure out my needs. The pain and palliative care team here is unbelievably caring and devoted. So are the physicians and nurses. I have created an expanded family here already and can’t say enough nice things about the quality of care and total commitment to the patient.
I think for now that’s enough news.
Please, please respect my declaration that I do not want uninvited visitors, any gifts, or any flowers sent during this time. I know the intent might be good, but I appreciate so much those who have opted to instead donate to my Sloan Kettering metastatic research fund instead of purchasing anything for me. I haven’t been able to send thank you emails for those recent donations but trust me, they are appreciated. Good thoughts are also always just fine and have the right price tag!
This is a time when I am dealing with severe pain, a medical diagnosis that is unfolding and serious, and needing rest as much as possible. I do read emails but I am not responding to most at this time.
I was not able to start the clinical trial because of these newest announcements. We will see if I am eligible for it again in the future but for now we have to get the disease and pain under control. I did go on chemo for a few days but it now needs to be stopped during radiation. I will resume chemo after radiation is over and about a week of recovery time has elapsed.
Things change hour by hour, day by day. I’m adjusting the best I can. I hope this will at least let you know where we are, a long way from where I thought I’d be in the first days of this new year. Welcome to the world of metastatic breast cancer.
December 29th, 2013 §
 No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
Everyone kept telling me how great I would feel after the thoracentesis. I did feel like I was breathing easier, but I didn’t feel great. In fact, I had quite a bit of pain. They checked for an air leak by x-ray as they always do after this procedure. There were no visible complications. But there was still tremendous pain starting that day and increasing into the next. It was more than the pain from the reinflation of a lung that had been compressed by half its size. But exactly what it was we weren’t sure.
By Thursday when I had to go back to Sloan-Kettering for my PET scan, echocardiogram, and EKG I was in agony. One of the doctors I met with could see how much pain I was in and prescribed some narcotics. I can’t take anti-inflammatories because I am having a liver biopsy next week and they put patients at risk for bleeding. I am so grateful a doctor seeing me about paperwork reached out to offer assistance and relief.
My father met me in the city. After I completed the required tests he drove me home. I can’t think of anyone better qualified to keep an eye on me than a retired cardiothoracic surgeon. Unfortunately, the pain continued. In all likelihood it is a combination of the cancer causing inflammation in the pleura and some nerve inflammation now that some of that fluid is gone and the lung is reinflated. It’s really all conjecture. We will see if the scans and tests reveal any additional information.
Oxycodone couldn’t keep the pain under control so yesterday I had to combine it with a Fentanyl patch. This duo is definitely helping me more; I’m still in pain but it’s more manageable today (Sunday). Each of these patches lasts for 72 hours and will deliver a constant stream of medication to me. I am pretty much bedridden.
It’s looking like Tuesday (New Year’s Eve) will unfortunately be a tough day. I was already scheduled to have a liver biopsy (This is not to check for malignancies; we already know there are metastases here. This procedure will be for repeated genomic sequencing analysis and other testing to make the best choices about chemotherapy and future clinical trials). Now, given all of the events this week, the team has decided that I need to have a PleurX catheter put in. This is a drainage system that will allow me to remove excess pleural fluid at home rather than having to have it tapped with a needle each time it builds up. The catheter will stay in place only as long as I need it, which will be as soon as treatment starts working and the fluid stops being produced in such copious amounts. I assume this will be at least a few weeks.
Having these two procedures and pain control issues means I will need to stay overnight in the hospital for observation. It’s amazing the lengths some people will go to to be in NYC for New Year’s Eve fireworks, isn’t it? Maybe Anderson Cooper will swing by while I’m recovering.
Once we see the results of all of the tests I’ve had and have these two procedures behind me, we will re-assess the plan to start the second clinical trial on Thursday. The most important immediate tasks at this point are to treat the two symptoms and get my breathing and pain under control. Immediately after that we go to work on the metastases to stop the problems at their source.
Thank you for all of the support I’ve had over the last few days including local friends who have been so kind and some friends who came from quite a distance to keep me company this weekend. I’m just putting one foot in front of the other and doing everything I can to gather all of the information I need to make a decision about what the best next step is.
Of course, as much as I can, I’ll keep you posted. Twitter is always the best way to keep up to date on daily happenings. It’s a lot easier for me to get quick bursts of info out in that medium. So many have asked: I have all of the help that I need and respectfully ask for no visitors or gifts during this time.
I would like to wish you all a happy and healthy 2014 if I don’t post again here before we all ring it in.
December 18th, 2013 §
 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
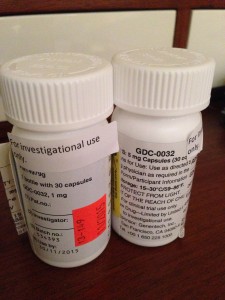
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.
December 12th, 2013 §
 Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Before each meeting with the Principal Investigator on the trial (an oncologist) I usually meet with a research nurse. On Monday I had the added pleasure of meeting with the Fellow assigned to this trial. She is a fabulous doctor: thorough, curious, caring. We spent more than 45 minutes going over a checklist of symptoms we must review at each appointment. I need to answer if I am having any of those symptoms, describe them in detail, and rate if they are better or worse than at the last visit. Then we discuss what to do to help alleviate the symptoms. Certain medications are allowed and others are not because they could conflict with the investigational drug.
At this visit my main issues were muscle pain in my back, fatigue, occasional bone pain in my collarbone, continued loss of appetite (though my weight has stabilized), occasional shortness of breath, dry skin and cracked heels, and some minor GI issues. My blood pressure and heart rate are elevated. My pleural effusion has stayed at the reduced level, fluid continues just in the lower left lung lobe.
In general, I feel quite good on the combination of GDC-0032 and Fulvestrant. I’m quite happy with my current quality of life on the combo especially compared to other options like IV chemo. I hope that it will continue. I have historically tolerated targeted therapies very well. I have not had any issues so far with mouth sores, rashes, or serious GI issues which are some of the more common side effects with the investigational drug.
I was able to ask all of my questions, most having to do with the coming two weeks. Next week is a big milestone: I will have my first CT scan and that will be the basis for determining if I can continue in this clinical trial. At least two radiologists will examine the CT. One radiologist from the hospital will read the images, while a second, separate radiologist assigned to the trial will make his/her own determination as to how much disease there is compared to the baseline CT 7 weeks ago. If the cancer metastases are considered stable or decreased, I will continue in the trial. If the cancer has progressed (grown) by 20% or more, I will need to stop taking the drugs and be removed from this trial. There are defined days that are the days I must have this scan done so that all of us taking part in the trial are assessed at comparable points in treatment.
Next I met with the Principal Investigator on the trial. This is the oncologist who is the point person for the trial and supervises all of the patients in the trial at Memorial Sloan-Kettering. We reviewed how I am doing in general, what the plan is for the coming 2 weeks, and discussed bloodwork. I told her that am anxious to hear how the other people enrolled in the study nationally are doing. Because we all started within a few weeks of each other, there aren’t many reports yet.
Because I have completed my loading doses of Fulvestrant (an extra dose of the drug is required in the first month of treatment), I did not have to get those injections this week. That was a treat. I will now receive the two injections monthly.
My medication diary documenting the time I stop eating each night and the time I take my medication in the morning was checked as were my pill quantities. I scheduled my next visit (adjusted a few days earlier because of holiday schedules there, I have a +/- 3 day window for the appointments now) and headed up to the third floor to have my blood drawn.
My port incisions are healing beautifully. I’ve toyed with posting a photo of what it looks like but haven’t decided about that yet. The nurse and I donned the requisite masks for port access and the blood draw was easy. I was then allowed to take my GDC pills and start the clock on the 60 minutes until I could eat and drink (I must always wait one hour after taking them). I left the hospital about 3 hours after I arrived.
We’ve been watching my tumor markers and aren’t quite sure what to make of them. They’ve been rising a lot in the past month but I am also getting varied results from my two testing sites. Of course, the key piece of data to look at is the scan. But it’s been a challenging few weeks emotionally as I see where the markers are, watch them rise, and wait for the scan to tell me what’s truly going on inside by body. In a few days I’ll have answers. And then I’ll either be continuing on the trial for another two months or moving on to plan B (which my team and I have already identified).
I continually try to bring my focus back to the distinction between worrying and planning. Worrying is anticipatory. The way I look at it is that worrying is spending time thinking about things that may or may not be/come true. Planning is taking strategic action to set things in place and control things that I can control in the midst of so much uncertainty.
Having a backup plan or a next step if the scan brings bad news next week is planning. It means if this trial isn’t working I know what I will do next and make sure those steps are in place so I’m not suddenly reeling and trying to cobble together a plan. But worrying about the results next week won’t do me any good. The cancer is doing what it is doing. These drugs are either working or they are not. And my sadness or frustration about that won’t change the reality of the cellular processes.
And so I have been quieter this week, choosing carefully how to spend my time. I’m searching for joy each and every day and finding beauty in the small moments: our dog Lucy playing in the first snowfall of the season, Christmas shopping with Paige last weekend, puzzling through math homework with Tristan, Colin and I getting haircuts together and going Lego shopping.
We hug a lot.
We say “I love you” a lot.
We always have done this.
But now I hold on for an extra second each time and I squeeze just a little tighter.
………………………………….
For those readers new to my posts about this clinical trial, you can see my reports about Cycle 1, Day 1 here and Cycle 1, Day 16 here and my port placement and Cycle 2, Day 1 here.
November 27th, 2013 §
 Next week I am meeting with a group of oncology Fellows at Sloan-Kettering to talk about care of the metastatic breast cancer patient. I have many ideas of how I think patients and doctors can better be “partners in care.” I have thoughts about how patients can be better in their interactions but this particular session focuses on the physician side of it.
Next week I am meeting with a group of oncology Fellows at Sloan-Kettering to talk about care of the metastatic breast cancer patient. I have many ideas of how I think patients and doctors can better be “partners in care.” I have thoughts about how patients can be better in their interactions but this particular session focuses on the physician side of it.
I will spend my time there emphasizing the things doctors can do in their future careers that will be most appreciated by their metastatic breast cancer patients. Having a supportive, educational partnership is essential.
I have pages and pages written on what I think makes a good oncologist but am not writing about them here yet. I really want to use today’s post as a forum to let you have input. Patients vary in what they want from their doctors. There isn’t necessarily a formula that will work every time. This is part of the message. It is important to find the right chemistry between a doctor and patient especially when you know this relationship will probably be taking you until the end of your life. Some oncologists start to distance themselves from their patients when they know they can no longer “fix” them. I am fortunate that mine are supportive. The balance between quality of life and quantity of it instantly becomes the metric after a diagnosis of incurable cancer. Everything is filtered through this lens.
I encourage you to comment on the post rather than email me. Even if you comment as Anonymous or with initials or even using your diagnosis as your name… I think reading what others think is important for this one. If you feel comfortable doing so, please indicate whether you have metastatic cancer.
So, without sharing my suggestions I’m asking for your input. Feel free to use these questions as jumping off points. Answer one, answer more that one, suggest something I haven’t even brought up.
I am interested in hearing from you what you think about some of the following topics and please be as specific as possible:
What is your preferred method of delivery of test results (ranging from the initial diagnosis to routine followup bloodwork and scans and biopsies)? Some results are given when only the patient is present. How do you feel about that? If you are called and told to “bring someone with you” you would that make you even more upset? In regards to bloodwork, scans, biopsies: do you always want those results in person even if it means waiting longer for those results? Do you mind if the results are by phone if that gets you answers quicker? Do you want the doctor to “cut to the chase” or do you feel more comfortable with small talk first?
How do you want a doctor to respond if you get emotional when you hear bad news?
Do you mind if your doctor gets emotional when delivering bad news or discussing your treatment? Does that make you more upset/scared or do you think that shows compassion?
A new report showed that patients don’t like when doctors talk about their own situations to try to show compassion (“self-disclosure to show empathy”). How do you feel about doctors sharing their personal stories of their own cancer or medical conditions, that of their family members?
Do you like when a doctor admits that he/she isn’t sure which treatment option is best for you or does that bother you?
Do you like when your oncologist presents the one treatment option he/she thinks is best or do you like your oncologist to present a few choices and then you decide together?
Do you like when your doctor asks you questions about your personal life/family/interests? Does your doctor do this regularly?
Does your oncologist talk about your prognosis and if so, what are ways you prefer those discussions to happen?
Do you want a doctor to give you a life expectancy prognosis even though we know those estimates are right only about 20% of the time? Do you want them to discuss it only if you bring it up? Do you like to hear statistics about treatment success and odds of survival?
How much monitoring do you like? Does your doctor give you a choice in how often to conduct tests? Do you feel that tests get in the way of living the life you have left or do you need the results to know where you stand in your treatment?
What is the best way a doctor has communicated bad news to you? The worst? (having a few examples of what not to do can be instructive here)
In the metastatic community in particular there seems to be so much of a focus on treatment and the nitty gritty of all that’s demanded to just treat the disease week to week, month to month. That is only one part of managing it. Have you been offered counseling for services like mental health? Palliative care? Family services? Physical therapy? End of life counseling? Would you like those to be offered to you?
How important are things like scheduling, having phone calls returned, having ways to contact your physician/office that are reliable, even after-hours?
If your doctor asked you to fill out a questionnaire with some of these questions on it would you find that impersonal or an attempt to learn more about you and how to best help you?
Would you like your doctor to have printed material with general definitions of terms and words important to your care (drugs, procedures, tests)?
Would you like them to discuss support groups? Have you asked? Have you been told there isn’t one for your kind/stage of cancer?
And finally: If you could give young oncologists one piece of advice, what would it be?
…………………………….
Thank you for your input. My advice on these topics could probably fill a book. I have a feeling yours could, too. I will try to address some of these topics in future posts.
By the way, I may not be posting over the next few days because of the Thanksgiving holiday.
As always, thank you for your daily support here, on Facebook and on Twitter.
November 24th, 2013 §
 I could not have known at that time the path my life would take. I could not have known how my words were reaching into the future, knowingly, achingly.
I could not have known at that time the path my life would take. I could not have known how my words were reaching into the future, knowingly, achingly.
I originally wrote about Katie Rosman’s book If You Knew Suzy in 2010. The blogpost was written before my diagnosis with metastatic breast cancer but years after my diagnosis of stage II breast cancer. My fears, articulated below, of my cancer returning and taking me from my family have now come true. It is interesting to read my words now through this new life lens.
Katie and I have grown so close since I first wrote about her book, her mother, and their effect on me. Our friendship runs deep. I treasure Katie’s thoughtfulness, her compassion, her devotion to her family, her laugh, and yes, I’ll say it: I am very jealous of her curly hair and ability to do handstands.
………………………..
November is Lung Cancer Awareness Month. Misinformation and stigma are still linked with lung cancer.
I get asked all the time, “Why do you think you got cancer so young the first time? Why do you think it metastasized?” I think people are searching desperately for identifiable reasons so they can feel “safe” from the fate I have (Clearly she must have done something to be seeing it once again, right? That won’t happen to me, right? If I just eat this or drink that it won’t happen to me, right?).
There is one question almost universally asked of those diagnosed with lung cancer: “Smoker?” There are many risk factors for lung cancer that have nothing to do with smoking. In fact, I only learned after having an oophorectomy in 2008 that surgically-induced menopause significantly increases the risk of lung cancer (one paper here).
Yes, current smokers are those most likely to be diagnosed with lung cancer. But there are increasing diagnoses of those who have never smoked and many who stopped decades ago. We need much more research into the spectrum of causes of lung cancer (including radon and asbestos exposure) and effective treatments. The stigma associated with it, however, is a barrier to raising money for research compared with other cancers. It is the deadliest cancer; more than 25% of cancer deaths are from lung cancer (more than from colon, breast, and prostate cancer combined) yet receives only a fraction of research funding.
I wanted to share this post again during Lung Cancer Awareness Month to highlight one life. Writing is powerful. Across time and space, without ever having heard each other’s voices or shaken each other’s hand, I have learned so much from Suzy.
Katie’s mother, Suzy Rosin, died from lung cancer.
……………………….
There comes a point in your life when you realize that your parents are people too. Not just chaffeurs, laundresses, baseball-catchers, etc.– but people. And when that happens, it is a lightbulb moment, a moment in which a parent’s humanity, flaws, and individuality come into focus.
If you are lucky, like I am, you get a window into that world via an adult relationship with your parents. In this domain you start to learn more about them; you see them through the eyes of their friends, their employer, their spouse, and their other children.
Yesterday I sat transfixed reading Katherine Rosman’s book If You Knew Suzy: A Mother, A Daughter, A Reporter’s Notebook cover to cover. The book arrived at noon and at 11:00 last night I shut the back cover and went to sleep. But by the middle of the night I was up again, thinking about it.
I had read an excerpt of the book in a magazine and had already been following Katie on Twitter. I knew this was going to be a powerful book for me, and I was right. Katie is a columnist for The Wall Street Journal and went on a mission to learn about her mother after her mother died in 2005 from lung cancer. In an attempt to construct a completed puzzle of who her mother was, Katie travels around the country to talk with those who knew her mother: a golf caddy, some of her Pilates students, her doctors, and even people who interacted with Suzy via Ebay when she started buying up decorative glass after her diagnosis.
Katie learns a lot about her mother; she is able to round out the picture of who her mother was as a friend, an inspiration, a wife, a mother, a strong and humorous woman with an intense, fighting spirit. These revelations sit amidst the narrative of Katie’s experience watching her mother going through treatment in both Arizona and New York, ultimately dying at home one night while Katie and some family members are asleep in another room.
I teared up many times during my afternoon getting to know not only Suzy, but also Katie and her sister Lizzie. There were so many parts of the book that affected me. The main themes that really had the mental gears going were those of fear, regret, control, and wonder.
I fear that what happened to Suzy will happen to me:
my cancer will return.
I will have to leave the ones I love.
I will go “unknown.”
My children and my spouse will have to care for me.
My needs will impinge on their worlds.
The day-to-day caretaking will overshadow my life, and who I was.
I will die before I have done all that I want to do, see all that I want to see.
As I read the book I realized the tribute Katie has created to her mother. As a mother of three children myself, I am so sad that Suzy did not live to see this accomplishment (of course, it was Suzy’s death that spurred the project, so it is an inherent Catch-22). Suzy loved to brag about Katie’s accomplishments; I can only imagine if she could have walked around her daily life bragging that her daughter had written a book about her… and a loving one at that.
Rosman has not been without critics as she went on this fact-finding mission in true reporter-style. One dinner party guest she talked with said, ” … you really have no way of knowing what, if anything, any of your discoveries signify.” True: I wondered as others have, where Suzy’s dearest friends were… but where is the mystery in that? To me, Rosman’s book is “significant” (in the words of the guest) because it shows how it is often those with whom we are only tangentially connected, those with whom we may have a unidimensional relationship (a golf caddy, an Ebay seller, a Pilates student) may be the ones we confide in the most. For example, while Katie was researching, she found that her mother had talked with relative strangers about her fear of dying, but rarely (if ever) had extended conversations about the topic with her own children.
It’s precisely the fact that some people find it easier to tell the stranger next to them on the airplane things that they conceal from their own family that makes Katie’s story so accessible. What do her discoveries signify? For me it was less about the details Katie learned about her mother. For me, the story of her mother’s death, the process of dying, the resilient spirit that refuses to give in, the ways in which our health care system and doctors think about and react to patients’ physical and emotional needs– all of these are significant. The things left unsaid as a woman dies of cancer, the people she leaves behind who mourn her loss, the way one person can affect the lives of others in a unique way… these are things that are “significant.”
I woke up in the middle of the night thinking about the book. My head spun with all of the emotions it raised in me. I think that part of the reason writing has become so important to me is precisely because I do realize that we can die at any moment. And if you don’t have an author in the family who might undertake an enormous project as Katie did, where will that explanation of who you were — what you thought — come from?
Is my writing an extension of my desire to control things when cancer has taken away so much of this ability?
Is part of the reason I write an attempt to document my thoughts, my perspective for after I am gone… am I, in a smaller way, trying to do for myself what Katie did for her mother?
If I don’t do it, who will do it for me?
And in my odd way of thinking, am I trying to save anyone the considerable effort of having to work to figure out who I was– deep down?
[My original blog had] the title “You’d Never Know”: I am telling you things about myself, my worldview, and my life, that you would otherwise have no knowledge of. One of the things people say to me all the time is, “You’d never know to look at you that you had cancer.” After hearing this comment repeatedly I realized that much of our lives are like that:
If we don’t tell someone — share our feelings and experiences — are our lives the proverbial trees falling (unheard) in the forest?
What if you die without being truly understood?
Would that be a life wasted?
If you don’t say things for yourself can you count on others to express them for you?
Further, can anyone really know anyone else in her entirety?
After a loved one dies, there always seems to be at least one mystery person: an individual contacts the family by email, phone, or in person to say, “I knew her: this is how I knew her, this is what I remember about her, and this is what she meant to me.” I know that this happened when Barbara (my beloved mother-in-law) died suddenly in 2009. There are stories to be told, memories to be shared. The living gain knowledge about their loved one. Most often, I think families find these insights comforting and informative.
Katie did the work: she’s made a tribute to her mother that will endure not only in its documentation of the person her mother was (and she was quite a character!) but also in sharing her with all of us. Even after her death, Suzy has the lovely ability to inspire, to entertain, to be present.
I could talk more about the book, Katie’s wonderful writing, and cancer, but I would rather you read it for yourself. I’m still processing it all, making sense of this disease and how it affects families, and being sad that Katie’s children didn’t get to know their grandmother. Katie did have the joy of telling her mother she was pregnant with her first child, but Suzy did not live long enough to see her grandson born. In a heartwarming gesture, Katie names her son Ariel, derived from Suzy’s Hebrew name Ariella Chaya.
I thank Katie for sharing her mother with me, with us. As a writer I learned a lot from reading this book. I had said in years prior that “we don’t need another memoir.” I was wrong. That’s like saying, “I don’t need to meet anyone new. I don’t need another friend.” Truth is, there are many special people. Katie and Suzy Rosman are two of them.
November 14th, 2013 §
 Tuesday was a full day for me at Memorial Sloan-Kettering for Cycle 1, Day 16 of my current clinical trial.
Tuesday was a full day for me at Memorial Sloan-Kettering for Cycle 1, Day 16 of my current clinical trial.
With snow flakes and rain mixing in the morning rush, I decided to skip the train and go early with my husband as he made his usual morning commute to New York City by car. I knew this would get me to the office quite early. I was the first to arrive in the waiting room and didn’t mind the long wait. It gets very busy and noisy later in the day and I’m always happy to sit in warmth and comfort of a quiet room. I arrived at about 7:20 and my first appointment wasn’t scheduled until 8:30. I was fasting, so I did miss my morning coffee quite a bit while waiting, though, especially as other patients began to arrive and use the coffee machine!
I meet with the research nurse first. She weighs me (down 2 pounds from two weeks ago), takes my blood pressure (oops, very high using the machine, we’ll retake it manually, oh that’s much better, thank you very much), pulse (in the 90s), oxygen saturation (better than last time, now normal).
We review how I am feeling on the Faslodex and GDC-0032 combination. This is the first time I am discussing it with the team since starting the protocol. She goes through a list of symptoms and asks about each one. The list ranges from gastrointestinal issues (very important to monitor on this investigational drug) to neuropathy to dizziness to fatigue to rash. I am pleased to report that I feel quite good on the combo. I experienced a few days of hot flashes and night sweats from the first injections of Faslodex two weeks ago, I tell her, but that was it. From the GDC I really only have had appetite loss, metallic taste in my mouth, a bit of muscle pain, and slight fatigue as the most noticeable issues. In general, we both agree, I am tolerating it very well.
The biggest change I’ve experienced in the last two weeks is a drastic change in my breathing– for the better. I’m quite sure, I tell her, that my pleural effusion (excess fluid in the lining around the lungs) is almost resolved. This is great news and I am anxious to find out if my doctor hears the change. I also tell her that after much thought I have decided to have a port placed to make my blood draws and tracer injections for CT and bone scans easier.
Next I meet with my own oncologist. Usually I would meet with the Principal Investigator for this appointment. She was not in the office on the usual days this week, though, and I must have my check-ins on certain days in the cycle. I was told about the switch in schedules well in advance. The plan for the long term anyway is that I will transition back to my own oncologist for monitoring. The two doctors work closely together and there is no problem in doing this.
I haven’t seen my oncologist in what seems like a while (probably about one month) and we are happy to be “reunited” for this appointment. We review how I am doing clinically. She also gives me a physical exam and listens to my lungs. Yes, she agrees, there is a big change for the better. We discuss the port, and she orders the needed additional bloodwork for it.
We talk about the trial and other topics. As always, she asks about my family and writing. I tell her about the song I wrote and promise to send her a link to it. I tell her I have been invited to come talk to the class of Fellows at Sloan-Kettering in a few weeks about caring for the metastatic breast cancer patient. I am truly excited about this invitation. There isn’t anything I can think of that is more important than talking to young physicians about ways to make doctors and patients partners in care in light of a metastatic cancer diagnosis. I’ll share more about that visit as the time approaches.
Next I do scheduling for the next appointment in 2 weeks. That will be a much shorter day than today. Each appointment in the first 8 weeks on the protocol has different elements. Today will be a long day. Next time will just be a visit with the Principal Investigator and a blood draw.
 Next I head upstairs to the chemo suite where they have a room waiting for me. They have already called downstairs while I am doing scheduling to tell me which room to go to so I don’t even need to check in. The nurse I had last time comes in to the chemo room. I immediately tell her that she did a wonderful job with the two huge injections of Faslodex last time. I tell her the slow injection rate seems to have worked; I was sore for days (expected) but no bruising or welts. I always try to give as many compliments as I can; I think these oncology jobs must be very stressful and I would bet the complaints come often. If possible, I try to find something good and comment on it. Everyone likes being appreciated.
Next I head upstairs to the chemo suite where they have a room waiting for me. They have already called downstairs while I am doing scheduling to tell me which room to go to so I don’t even need to check in. The nurse I had last time comes in to the chemo room. I immediately tell her that she did a wonderful job with the two huge injections of Faslodex last time. I tell her the slow injection rate seems to have worked; I was sore for days (expected) but no bruising or welts. I always try to give as many compliments as I can; I think these oncology jobs must be very stressful and I would bet the complaints come often. If possible, I try to find something good and comment on it. Everyone likes being appreciated.
Today I will need to have my blood drawn, take my GDC-0032 pills, wait four hours, and have my blood drawn again. I must always wait one hour after taking the pills to eat. By the time I do all of this today it will be noon. The nurse gets a vein in my wrist easily for the required 12 vials and when we see it’s a good flow we agree to leave the line in and try to use it four hours from now and avoid another stick. I’m reactive to adhesive so she wraps me up carefully and I slide my sweater sleeve back down.
I take my pills with a full glass of water and document the time in the medication diary that I am required to keep. Then it’s time to drop my trousers for the two big Faslodex injections. I am not too nervous about this part now that I’ve done it once already. I will get these today, again in two weeks, and then monthly thereafter. I have mastered the art of muscle relaxation for these shots and use a trick of putting all of my weight on one foot while they inject the opposite side. Again the shots are uncomfortable because the viscous liquid is getting rammed into a muscle. But she does it slowly again as she is supposed to, and we’re done quickly. I still am self-conscious as the lightly-frosted sliding glass doors are all that stands between my tush and the hallway, but I’m already over that. I think the idea of facing the wall and clutching a table as needles are jabbed in my backside is probably more laughable.
I put on my coat, knowing the worst is over for the day and go meet a friend for lunch after waiting the required time to eat.
Later, I return directly to the same room I was previously in at the appointed time. The line still in my wrist yields a good flow, a few more tubes are drawn, and we’re done for the day.
Seven hours after first entering the building I am free to go. I still have two more weeks’ worth of the GDC-0032 in my bag and so I do not need to visit the pharmacy. At the next visit my medication log will be checked and my remaining pills will be counted and confiscated before I am given another 30 day supply.
…….
Over the last two days I have ended up needing two more blood draws, met with my local oncologist, and got my monthly Xgeva shot. After 7 needles in 3 days I’m glad to now have a few days off. I ended up needing to repeat one of the tests required for the port placement procedure (Tests related to clotting are routine before any surgical procedure. One of these was slightly elevated and I needed to repeat it. The second test came back just fine).
I also had my tumor markers done. This blood test is not a part of the clinical trial requirements. I’ve decided to watch these to see what they do while taking the drug. I’m sure some people would not choose to do this. This week’s test showed the numbers were quite elevated over previous weeks. We don’t know what that means. I have no increased pain, none of my other bloodwork shows any reason for concern. The numbers sometimes rise on new therapy before they drop. My breathing is significantly improved. So, we focus on the clinical signs and will just have to see what the markers do. I wish they had dropped, but I’ve seen the imperfect nature of this test time and again. I am able to realize this is only one piece of the puzzle right now. It doesn’t affect anything about my treatment plan. A reminder: in this trial success is measured by doing CT scans at varying intervals. My first one will be five weeks from now, at the seven week mark. Only then is a determination made about whether it is working, which would be disease stability or reduction. If the overall “quantity” of cancer is seen as growing by 20% or more, I would discontinue the trial and need to move to something else; it would be considered ineffective for me.
I was sore far more quickly after the Faslodex injections this time even though they weren’t any more painful at administration time. By the time I was on the train back home in the late afternoon I was hurting. For three days now I’ve had a heating pad on as much as possible. It just feels good. The seat heater in my car is getting a workout too. I know it will only be another day or two so I am not too bothered.
I don’t yet have a date scheduled for the port placement. That could be as soon as next week. I also have meetings with my cardiologist (these inhibitors can drastically change lipid levels. My cholesterol and triglycerides on my previous drug, Afinitor, went quite high. Thankfully they are coming down rapidly now but we still need to watch them carefully.) and my endocrinologist (my thyroid levels are now abnormal again. I have Hashimoto’s Disease which is usually very easy to manage but chemo does sometimes cause changes). I’m not in a huge rush to get the port, I just would like to have it in by the time I need to do the next round of scans.
I’m glad to finally be done for the week with appointments, hard to believe the weekend is almost here. I will see what next week brings and then it will be time to be back at MSK on the 25th of November for Cycle 2, day 1.
November 11th, 2013 §
 Today is Veterans Day.
Today is Veterans Day.
Each year on this special day and Memorial Day my letter to troops stationed overseas is similar. Each year I question whether I should write something new, if it’s “cheating” to say the same thing. In the end I realize that thank you never gets old, it never needs to be re-written. Thank you doesn’t have an expiration date.
November 11, 2013
Dear Servicemen/women,
My family and I want you to know that we have not forgotten you or the sacrifice you are making every day to be away from your own families and in harm’s way. It’s not much, but perhaps knowing you are in our hearts and minds will help.
Six years ago I was diagnosed with breast cancer. I was in remission for more than five years and now my cancer has metastasized to my bones and lymph nodes. It is not curable.
As I go through treatment, people called me brave. I don’t think I deserve it. “Brave” is not a word you used about someone like me. I have gotten cancer by chance and I am dealing with it, the best I can.
But soldiers? You are brave. You have a choice—you put your lives on the line after making a conscious decision to do so. You know the danger and you do it anyway. To me, that is true bravery, true heroism.
Seeing danger and making the choice to proceed anyway is precisely how I define bravery. We all find ways to deal with the fear of death. We know the uncertainty that lies ahead. We see the bravery in others before we will see it in ourselves.
What underlies bravery: chance or choice? Can both?
Are we just hesitant to see the quality in ourselves? Are we just modest? Do we just act the way we need to, to get the job done?
I think when you choose to throw your hat in the ring, that choice counts for something.
That makes you brave.
That is what makes soldiers heroes.
To all of our veterans, thank you for your continued service to our country.
Lisa Bonchek Adams
(The photo above is of a needlepoint project I started work on long ago. Instead of doing a traditional flag I decided to stitch it as a sampler. It is obviously only partly finished but I love how it ties in to this post.)
November 6th, 2013 §
 Even when I am alone
Even when I am alone
I teeter precariously over the right hand side of the bed.
On my left shoulder when I can,
When the pain is bearable,
When I can settle in for the night.
I still approach the precipice
Rather than opt for the safety of the middle place.
I act as if he is there with me
Taking space
And I, trying to make room,
Move to outer orbit,
As if that extra inch or two would matter.
Even on the occasions I am alone
I pretend as if I am not.
I go to places in my mind,
Wondering what it will be like
When that opposite side of the bed is empty
For him
And he teeters precariously near the edge unnecessarily,
Without me there to take up space.
October 30th, 2013 §
 There is so much to say about the start of the phase 2 clinical trial earlier this week. I think it’s important to be as complete as I can on the main parts. I really want readers to get a sense of what it’s like to go through this and also what to expect if they decide to enter a trial themselves.
There is so much to say about the start of the phase 2 clinical trial earlier this week. I think it’s important to be as complete as I can on the main parts. I really want readers to get a sense of what it’s like to go through this and also what to expect if they decide to enter a trial themselves.
That said, it is obvious to me (and hopefully to you) that my experience is very unique. I have no earthly clue what other trials are like. I just want to make all of the disclaimers that I think you all know already: this is my experience only. If that helps in some way, great. But it can’t possibly tell you what another clinical trial might be like.
I still think it’s valuable. And I know I would have wanted to read posts like these a few weeks ago when I was signing up for the trial. So that’s my guide: if I think it would have helped me, I’m going to share it.
Twitter friends have been telling me that they are interested in five main topics: 1) what is the science behind this drug? 2) what does the treatment consist of/logistics 3) how did I choose this trial out of the ones available 4) side effects physically 5) effects emotionally. The last two will obviously be the ones we follow over time. I won’t be able to address all of those topics here but I’m getting a good jump on them.
This post is long. I’ve opted to just publish it and not divide it up. If you want to read it in chunks you can decide how to divide it up. If you want to skim the science parts, you’ll still have my report of my day at the end. I look forward to hearing your questions and comments. If you have questions I will try to answer them.
First, a bit about the drugs and the science behind them. My trial has me taking 6 mg of an investigational drug called GDC-0032 made by Genentech every morning. I receive two injections of a drug called Faslodex every month, with an extra dose halfway through the first month.
It is important to understand that these particular drugs for metastatic breast cancer are not traditional (cytotoxic) chemotherapy drugs. What I mean by that is that most people think about chemo as being drugs you receive, most often via IV, that makes you feel rotten and your hair fall out. That’s the type most people are familiar with and that class of drugs includes what I had when I had treatment for stage II breast cancer in 2007 (Adriamycin, Cytoxan (least creatively-named drug of all), and Taxol).
Those drugs are cytotoxic (cyto= cells, toxic= poisonous). So, the drugs kill the cancer cells but they kill other cells too. That’s why your hair falls out, you feel sick, your blood counts drop and a host of other issues.
With my kind of cancer (estrogen receptor positive, progesterone receptor positive, HER2 negative) there are other types of drugs to use to try to slow the cancer’s growth down. This is not the case for all types of breast cancer. With some you can only use traditional chemotherapy. In addition, and most importantly for this trial, my cancer shows a mutation in the Pi3k pathway. I know this is getting very science-y. But I’ll try to explain the rationale for this drug.
Many people with my kind of breast cancer (and other types of cancers, we’re learning) show a mutation in this pathway. You might have heard of genomic sequencing. It is testing the tissue of your cancer to see if your particular cancer has any mutations in its coding that facilitate the cancer’s growth (I’m oversimplifying here). This pathway, which is called the Pi3K/AKT/mTOR pathway, can become overactive and drive the cancer’s growth.
I have one mutation in the Pi3k section of the pathway. There are many forms of mutations in the Pi3k pathway. There can be other mutations in other areas as well. Mine is called a Pi3k-alpha mutation.
So what the investigational drug is targeted to do (hence the term “targeted therapy”) is to block this Pi3k/AKT/mTOR pathway that has been over-activated, potentially by this mutation.
This all sounds great. But it’s not so easy. It isn’t as easy as “find the mutation, create the drug, block the pathway, cancer goes away.” We don’t have indications it will ever be like that. The signaling pathways of cancer are highly complex, variable at any given point, and also change over time.
In addition, not everyone with the same mutation responds to the same drug. And combinations of drug seem to work better. Think about doing clinical trials of endless permutations of drug combinations with different mutations, different cancers, in different bodies… well, this is why science seems to move at lightning speed but our advances in treatment just don’t mirror that in all cancers. We have no way at the moment to predict what the best course of treatment is for any individual person. For now, you throw the pasta at the wall and see if it sticks. Unfortunately, our lives are the test cases.
To return to the science, I’ve already tried an mTOR inhibitor in my last treatment phase. That was called Afinitor (combined with another drug called Aromasin). But that targeted a different end of the pathway, and not the mutation. The problem with all of these right now is that the cancer figures out a way around the blockages. It develops feedback loops. If you’ll allow me to anthropomorphize cancer for a minute, it says, “Hey, okay, so you want to block the road? I’ll just detour and still get the end point. I’ll get fuel to the cancer somehow. If you block me, I’ll just keep finding a new way to deliver the goods.” And that’s why metastatic breast cancer is incurable. It keeps finding a way to find fuel and becomes resistant to each thing you throw at it. I became resistant to that Aromasin/Afinitor combination after about six months.
In terms of side effects, unlike traditional IV chemo, with this investigational drug you don’t “feel rotten” right after treatment. It can take weeks and potentially months for side effects (especially some of the serious ones) to take hold. So that’s one way this differs from what people might think. My phone has been buzzing non-stop since Monday: “How do you feel? How do you feel?” I will have some effects from the injections (which are hormonal agents, this one is an estrogen receptor agonist) quickly. I already have some of those. Other side effects from the pills (the GDC-0032) will come later.
So… here we go.
Monday was Cycle 1, Day 1.
If you are interested, my trial protocol is here (I am in the phase II group). This tells you exactly what this study is. If you want to read a bit about the early results of this drug in phase 1 trials you can see that here.
On day 1 I received my GDC-0032 pills for the month (and took the first dose), received two injections of Fulvestrant (Faslodex), and had about 8 vials of blood drawn.
The logistics of getting to the city were a bit of a challenge this week given fatigue and the lingering pleural effusion. The train, subway, and walk were tough but I always try to push myself. Knowing I’d be stuck inside for a few hours definitely had me enjoying the cool crisp fall air on the walk to the hospital.
Because of train times I arrived one hour early for my appointment. I wasn’t sure if I was doing this blood draw before seeing the doctor or after so I settled in. After only a few minutes I was surprised to be called back to an exam room. There I had a long meeting with research nurse whom I’ve spoken with by phone but not met in person. It was an extremely thorough meeting. She answered questions, reviewed the protocol, went through my current medications again, noted all physical symptoms I’m having now. We also discussed my most recent bloodwork (my lipids changed drastically during the 3 week washout period. My prior chemo had raised my cholesterol significantly. My LDL dropped a whopping 100 points in a two week period once I stopped the old chemo, for example). Blood pressure, pulse, oxygen saturation, height, weight. Other research assistants on the protocol come in and talk to me, discuss things, physical exam, as eventually does the Principal Investigator (the doctor in charge of the trial).
It took about two hours to complete these meetings, exams, tests, questions, medication review, etc. Everyone was very thorough and I was offered every opportunity to ask questions about not only the trial but also about any symptoms I was having and how they could be helped.
They also stressed how important it is to call with any and all side effects. As the more serious side effects become more possible/likely, it’s important to report any issues right away so they can be managed before they get too serious. Communication is key in clinical trials. I’ll talk about the side effects more in the future.
For some questions about side effects we needed to refer to the protocol of the trial (Can I get radiation to a bone if my bone pain continues: Yes, but not within the first two weeks of the trial start. Can I get the fluid around my lung tapped if it becomes too troublesome: Yes, at any time).
We also discussed a port for my blood draws/access for radioactive dye injections for CT and bone scans that I will need to have done every 8-12 weeks on the trial. I am still undecided about the port. We agreed to see how it goes in the next few weeks with the blood draws. I can only use my right hand which doesn’t allow for easy access or many misses. They tell me there is a “three miss rule.” If they can’t get the blood they need within three tries, they stop. I have a terrible feeling this rule will come in handy.
At the end of the meetings they handed me many sheets of paper.
First, I received a medication diary where I need to document the time I stop eating every night and the time I take my GDC-0032 pills (the “investigational drug”) the next morning. The pills must be taken on an empty stomach one hour before food, with a full glass of water at approximately the same time every day.
Second was a list of drugs and supplements I cannot take while I am on this protocol.
Finally, there was a schedule for the next 8 weeks of what will happen at each appointment, what tests and drugs I will receive, what I need to do to prepare, and what I need to bring to each appointment. The pills are given in quantities of 30 but I will probably be at appointments every 28 days. The surplus pills must be traded in and counted before I can receive the next month’s supply. Though it is only one drug it is dispensed in two capsules, one dark red, one pine green. One is a 5 mg, one is a 1 mg for a total of 6 mg.
I was then sent to do scheduling for my next appointments. I will need to return in two weeks (plus or minus 2 days) to do vital signs, exam, fasting blood draw (but this time it must be done twice: before taking my pills and then again 4 hours after), and my two injections.
I then went to the hospital pharmacy to collect my pills. They are labeled with my name, the drug name, instructions, and so on, just like a regular prescription. The protocol number is labeled on the bottles too. The bottles also say “Cost $0.00” on them.
This drug is provided free of charge to me but my insurance company is billed for the injections of Faslodex, lab work, and all scans. Trials differ in what is covered. In this case, only the investigational drug is provided free of charge. The rest of the expenses including the visits with the doctors are not provided for free. I am fortunate. My insurance will help pay for those things. Your care is not necessarily fully covered when you are in a trial, contrary to popular belief.
The pharmacy cashier placed the two bottles (one bottle of the 5 mg, one bottle of the 1 mg) in a brown paper lunch bag and handed it to me. In that moment I feel like I have something very valuable and secret in my possession, perhaps even magical. I don’t know if these pills will do anything for me. They could do me more harm than good. They could do nothing. But they might buy me time. Those are, for now, mysteries.
The brown paper bag with the drug bottles inside seems very wrong, far too flimsy for the weight of the hope that lies within.
I then left the pharmacy and headed upstairs to the chemo floor where I had my fasting bloodwork done (by now it was past 11 AM and I was glad I started early. I really don’t mind not eating, it’s the lack of coffee that gets me. Also, the longer I wait the harder the blood draw is likely to be).
In this room I will also receive my two injections. As I enter the room, I’m wondering about those and anxious. The number of needles I have in a month is astounding sometimes. I was the girl so afraid of shots as a kid I once ran into the parking lot to try to run away to avoid getting a vaccination at a pediatrician’s visit.
One chemo room is dedicated to this trial. I have gone to the same room each time so far. The trial tech doesn’t even try to draw my blood. He calls in the reinforcements. Eight or so vials of blood are taken by a nurse who goes after my hand vein with a vengeance. Unfortunately I receive a call the next day that two of the vials are unusable (hemolyzed). This happens sometimes when large blood draws require a lot of work (suction) to get. I was able to go locally the next day to have the two vials redrawn.
After the blood draw it was time for the “standard of care” drug. This is part two of my clinical trial protocol. The “standard of care drug” means I am given not just the experimental drug, but also a drug that is a reasonable option for treatment for this stage of my disease.
On its own (“single agent”) Faslodex works for some people but seems to have a better track record when combined with another agent. My trial is one that combines Faslodex injections (standard of care) with the GDC-0032 (the investigational drug). There is no placebo. This is a phase II trial. I will get both. We will see if taking the GDC-0032 provides a better result than the historical success rate of those who have received the Faslodex injections alone. There will be 60 people nationally doing this combo, about 10 of them at Sloan-Kettering. I am the fourth person, I believe, to get started on it (the trial just opened a few weeks ago at Sloan).
Faslodex is given by injection, intramuscularly, in your rear. No fancy fun way to say it. You drop your trousers and they have syringes that are over 4″ long (can’t find any literature that states exact measure. I’m going to ask to measure it after my shots next round. I confess I saw them when we were done and they made me a bit nauseated and I didn’t want to be precise!). The needles are thick because the liquid that has to be inserted is very viscous and doesn’t go into the muscle easily. I was fortunate and the nurse did a great job. I tried to remember the tip to keep your muscles relaxed during an intramuscular injection, but it’s hard when you know the size of the needle that’s taking aim for your ass.
The first injection really wasn’t worse than a regular shot. The second one hurt more than the first but still less than I had expected. I opened my bottles of pills, took out one of each, drank my water as directed. I noted the time in the diary.
At this point I was free to go. The injection sites were not immediately painful and I was sent on my way.
Everything was incredibly efficient and while I was exhausted, I was relieved. I kept thinking to myself: “Once again after three weeks of not being actively treating my cancer because of the mandatory ‘washout’ period, I am doing all I can. Action feels good.”
I celebrated getting through day 1 by having lunch with my friend Julie Klam which was such a luxury after the poking and prodding of the morning. I took the train home and felt a sense of accomplishment.
So, in case it wasn’t clear, my next appointment will be two weeks after my start date (“Cycle 1, day 15 +/- 3 days” in protocol speak.).
I think the word that most defines metastatic breast cancer to me is “uncertainty.” You have to figure out a way to live with it. My coping mechanisms are research and action. I can only hope these will serve me well.
I thank you for your support and encouragement this week.
October 26th, 2013 §
 I know I shouldn’t always attach explanations on posts like this but today I feel the need to. Whenever I post a dark piece I get many messages of concern (and criticism) from people. Sometimes they say “Lighten up.” Most often readers are worried. I want to say that these pieces capture only a fraction of the spectrum of feelings I have.
I know I shouldn’t always attach explanations on posts like this but today I feel the need to. Whenever I post a dark piece I get many messages of concern (and criticism) from people. Sometimes they say “Lighten up.” Most often readers are worried. I want to say that these pieces capture only a fraction of the spectrum of feelings I have.
My days are not spent wallowing in sadness. When I need to rise to the occasion I do. It’s often easier for me to write about the world of the dark places though… in some ways I think those are the ones that need light the most. These words are often the ones which go unwritten and unexplored.
I always find joy in the small moments each and every day. Today I tweeted, “I find beauty in the flowers in my room, the sight of the leaves through the window, the sound of the wind, the loyalty of my dog.”
There is shimmer in each and every day. Some days we just have to look hard for it, dig deep. And some days there is just a darkness overhead. I find that giving a voice to the those depths, shedding light on them, is important. There are many who live in this land. Today’s post comes from the feeling of doom that accompanies test results, that awful waiting period.
………………………
I wait for the burlap bag over my head,
Wait for the rope round my neck.
I wait for the chair to be kicked out,
The floor to drop open,
Snapping the rope’s length and my body with it.
This is what it feels like each time I drive to the office,
Head into the building,
Take a seat.
Usually I hate traffic
But when it slows my journey I find myself grateful these days.
Stretch out that time.
Make it longer until I hear words I don’t want to hear.
They are tricks, of course,
Silly childish games I play.
I turn on the heated seat and press my back against the core
Burning relief into my spine.
I am at war with myself.
I ready myself to smile, to say good morning,
To greet the office staff with a brave and carefree smile.
“How are you?” one will ask,
Letting the words roll off her tongue the same way
The lady with the Irish accent ringing up my groceries asks me
Without waiting for an answer.
I’m not fine.
I’m anything but.
There is no time for that, though.
It’s time for results and plans and tests and exams.
It’s time to steel myself again,
Stand up straight,
Pretend there is no fear,
No ache,
No catastrophe.
For minutes at a time this is how I get through the day.
I walk at a clip, slightly faster than that executioner with the bag and rope who chases me,
One step behind or maybe two,
Telling him
No.
Not today.
Just stay the hell away from me.
Just for a little while longer.
October 18th, 2013 §
 I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I had CT scans of my chest, abdomen, and pelvis. I also had a bone scan of my body. I had bloodwork and an EKG and a urine test. These are all tests that need to be done before I can start the clinical trial and will be used as my baselines. Monitoring will happen at frequent points throughout my treatment. Bone scans and CT scans will be done every 8 weeks for the first 6 months and every 3 months thereafter for as long as I am on the protocol. I’ll write more about the trial and the drugs (fulvestrant and GDC-0032) when I get underway on the 28th. I had a lot of trouble with with the blood portion as I only have my right hand and forearm for blood. It took six needles in that area (which included two blown veins) to get all of the radioactive tracers in and blood out. I will be discussing the option of putting in a port at my next appointment.
So the short story is that results were not as I’d have hoped. I wanted it to be clear that the cancer was still confined to my bones and lymph nodes, even if it were in more bony locations. This, however, is not what it seems to be.
First I need to explain about the tests. I’m going to briefly try to explain why it’s a bit of apples and oranges to compare my test from August with my tests last week and why all of it is a bit jumbled. In August I had a PET scan. In oversimplified terms this test picks up on high activity metabolic areas. So, cancerous tumors (and also some false positive areas on occasion) “light up” because they have a high number of rapidly dividing cells. It measures activity. CT tests, on the other hand, are static. They are like x-rays. They just take a picture without regard to whether the nodule/lump/tumor etc. is malignant. It shows there is something there but can’t necessarily tell you what it is in terms of metastatic breast cancer. CTs are very precise visually. PETs are not necessarily so. CTs in my case can’t tell us for sure if a spot is malignant.
I now have a small spot showing up on my liver that wasn’t visible on the PET in August. So is it a new metastasis? Or is it a benign spot that just didn’t show up on the PET because it’s not cancer? Who knows. We will have to wait and see if it changes when we do the next scans 8 weeks after the trial start (10 weeks from now). There are also nodules in my lungs and pleura. These are potentially (likely) malignant but the ones in my lungs have not changed size in 8 weeks.
I think that’s as much detail as I need to go into. The worst spots in my bones are my T12 vertebrae and my first rib/clavicle area. There are many spots but those are the ones that cause the most pain.
Unfortunately and most significantly at the moment, the scans also showed that the small pleural effusion (fluid in the lining around the lungs) has grown.
So we have many question marks with a few new areas of concern. For now we watch and wait. The pleural effusion will need to be drained if it grows or continues to cause breathing problems. For now any physical exertion gives me trouble. I need rest throughout the day but am trying to conserve energy for activities with the kids.
None of this news changes anything about my planned start of the clinical trial. Whatever these spots are and wherever the metastases are, the drugs I will start in ten days have the best chance to keep the spots stable and eventually perhaps shrink them. Reports from the phase 1 trial participants showed that often there was a stability period of about 8 weeks before some achieved some tumor shrinkage. I have ten more days to go chemo-free before I begin. I am counting the days. That start day is the most important day I have. A few of us in the trial are starting on that day so hopefully I will get to meet some of the other participants. There are 60 nationally in this phase 2 trial, approximately ten people will be at my location. There is relief in knowing there is no placebo in this trial. I may not respond but it won’t be because I received a placebo.
I wish I had better news about the scans but I also am resigned. This is what this disease does. I must do the best I can given my daily symptoms. There are questions marks and only time will give us answers. I try to have as much normalcy as I can, which often just feels like sleepwalking through the days and a bit of play-acting. But it’s important.
I keep coming back to a few lines I wrote recently:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
I can’t do anything more to change what’s happening inside. I have a plan and I just need the days to go by to get started. My quality of life is suffering at the moment but I hope that this will change. It is a rollercoaster, one I have been strapped inside unwillingly. Some days are good, some days are not. These happen to be some of the icky ones, but as always, I press onward.
Every morning I say to myself:
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be tough to do. Persevere.
October 12th, 2013 §
 Hi all,
Hi all,
The interview on Al Jazeera America last night was not available to many who wanted to see it (even we don’t receive the channel). Thanks to my brother Mark I now have a link that you can use to watch it and/or download it. I am not sure how long it will be active so if you are reading this a few weeks or months from now I can’t guarantee they will still be active.
I think the show was great, I was so happy to be featured with Gayle Sulik and Dr. Susan Love… we definitely could have continued the coversation for another half hour. Kudos to AJA for giving us the time.
The photo above is of two of my nieces watching me on TV. Love it!
I welcome your feedback in the comment section. I wish I could have said more about metastatic disease but that wasn’t the true focus of the show.
Hope you all are enjoying your weekend.
October 7th, 2013 §
 There comes a moment in many conversations,
There comes a moment in many conversations,
I can see it:
They reach their limit.
Ten minutes in, or maybe only five,
They start to drift off,
Squirm,
Just want to be done with it.
Sometimes they even say,
“Let’s talk about something else” or
“Let’s change the subject”
Every so often they go as far as to say, “This is depressing.”
Being done with it is something I would love to do.
I’d love to tell the inner me to forget about it.
But that’s not possible.
It’s not mind over matter when that matter is making you sick, as are the treatments you need to fight it.
Metastatic cancer is background music, but it is a cacophonous roar.
I put it in its place,
But it has a place.
And the fact that it even has a place,
Well, that is just the way it is.
I try to keep its place as small as possible.
For as long as I can.
But I don’t have the luxury of changing the subject or forgetting about it for a while.
Like a greedy child metastatic cancer demands attention.
I tell it to wait,
Give me a bit of a break.
First I demand it.
Then, worried, I ask again contritely.
Then I downright beg.
Please, just give me some more time.
But I don’t believe there is anyone who hears me.
I don’t believe there is a god listening,
And I don’t believe cancer gives a damn about it all.
And so the plea evaporates as quickly as it came,
The tree in the forest with no one to hear.
I can only do my research, try to make the best decisions.
But in the end,
These cells will do what they will,
As they have,
Without respectful regard to all of my attempts to banish them.
That’s not how it works:
You can’t wish them away,
Hope them away,
Love and light them away.
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
And in those conversations now I am grateful there can be other subjects to move on to,
Share the lives of my friends and support them,
Even if I am simultaneously pretending I can’t hear the roar.
The greedy child still tugs at my hem,
Will not be denied.
I needn’t let that noise drown us out,
And it won’t silence me just yet.
October 4th, 2013 §
 Once again Facebook games about breast cancer are making the rounds now that it is October. I posted this last year and got some flack from people who thought anything that “raised awareness” about breast cancer was good and couldn’t understand why I am critical of these messages.
Once again Facebook games about breast cancer are making the rounds now that it is October. I posted this last year and got some flack from people who thought anything that “raised awareness” about breast cancer was good and couldn’t understand why I am critical of these messages.
My point is that this isn’t awareness.
There probably isn’t anyone on Facebook who doesn’t know that breast cancer exists. But there certainly is a lot of myth-busting to be done. This is not how to do it. Topics that do need attention include male breast cancer, the underfunding of metastatic research (30% of people with breast cancer will eventually have metastases yet less than 5% of breast cancer funding overall goes to metastatic research), the fact that for many breast cancers 5 years in remission does not mean you’re free from risk of recurrence, not all breast cancer presents with a lump (inflammatory breast cancer)… the list goes on and on.
There’s a lot of work to be done educating. Education is awareness, these Facebook posts are not.
A friend asked me, “What can I do to help? I can’t donate money to your research fund but would like some ideas on things I could do instead.” What a great question. Rather than post these messages on your Facebook page here are a few easy ideas:
1. Make sure you are properly vaccinated from vaccine-preventable illnesses. This includes your family (kids and your parents if applicable), friends, and anyone else you can get involved (nag). Boosters like those for pertussis are very important. Get your annual flu shot. People over the age of 65 and some others at high risk should also talk to doctors about the pneumonia vaccine.
2. If eligible, donate blood and platelets. These products are needed by cancer patients constantly.
3. If eligible, get tested to be a bone marrow donor. Go to BeTheMatch.com to see the requirements. The initial registry just requires a cheek swab. It’s easy as can be.
4. Read blogs/follow tweets by people living with cancer. I think understanding the day to day lives of those of us living with it is a great way to truly become more aware. It’s one of the reasons I spend so much time writing here. I try to bring you the science, the experience, the thoughts of a mother trying to cope with raising a family and managing an terminal diagnosis.
Now on to the Facebook posts… here is a slightly modified version of the post from last year. You can go back to the original if you want to see comments made then.
……………………………
I don’t usually rant, but something has me steaming. Today the following exact message appeared in my Facebook inbox:
So here is the time of year again when we try to raise awareness for breast cancer through a game. It’s very easy and I would like all of you to participate. Two years ago we had to write the color of our underwear on our wall. Men wondered for days at what was going on with random colors on our walls. This year we make references to your love life status. Do not answer to this message just post the corresponding word on your wall AND send this message privately to all the girls in your contact list!!!!!! BLUEBERRY = single; PINEAPPLE = it’s complicated; RASPBERRY = I can’t / don’t want to commit; APPLE= engaged; CHERRY= in a relationship; BANANA=married; AVOCADO= I’m the better half; STRAWBERRY= can’t find Mr. Right; LEMON = want to be single RAISIN = want to get married to my partner. Last time the underwear game was mentioned on tv, let’s see if we get there with this one !!!!!Copy and paste this message into a new one and send to all your girly friends and update your status with your answer. DO NOT RESPOND TO THIS CONVO, just leave and participate.
One version I received yesterday says this:
Hello Ladies, Without replying to this message, put a heart on your wall; no comment, just a heart. Next, post a heart on the wall of the person who sent you this message. Then send this message to your women friends, only women. If anyone asks you why you have so many hearts on your wall, don’t tell them. This is only for women, because this is breast cancer research week. One small act of solidarity between women. PS to type a heart, first type < then 3 It will turn into a heart as soon as you post.
………………………
I’m going to keep my reaction short. I’m hoping writing something down like this will allow people who are as infuriated as I am with these silly requests to have something to react with.
First, I give you permission to ignore this crap. Better yet, write back to the people who have shared it. Let’s do some real awareness here.
The above instructions are not awareness. This is offensive. Breast cancer is not a joke, awareness does not come from sharing the color of your underwear or your marital status (the whole “tee-hee, wink-wink” attitude adds to my disgust). Even if it ended up on TV, that still would not be educating people about breast cancer they didn’t know before. All it does is show the world that lots of people are willing to post silly things as their status updates.
Let’s do a piece of education right here. The status update says “only send this to your girly friends.” Men get breast cancer too. Men are also the husbands, fathers, sons, brothers, and some of the friends, coworkers, nurses, and doctors who care for and are left grieving for people (men and women) who die of breast cancer. We should not exclude them from ANY discussion of cancer.
Just because it says it’s about breast cancer awareness doesn’t mean you have to agree. Go ahead. Ignore it. Or write back and tell them why you don’t want to be included in these things anymore. Another blogger, Susan Niebur, wrote about her take here. She was an astrophysicist, by the way. She died of metastatic breast cancer.
Anyone who has breast cancer and uses your FB status update as an indicator of whether you support their cause is not very enlightened. When I rank “how to help those of us with cancer,” sharing one of these paragraphs as a status update is the lowest possible method of showing support. There are endless ways to do that. I think it actually is the opposite; sharing these status updates makes people feel they are doing something real for breast cancer causes when they aren’t.
I’ve also had it with the I’ll bet most of my friends won’t share this post attempt to guilt me in to sharing something like “share this if you think domestic abuse is awful.” “Share this if you think autistic kids are special.” Well yes, actually, I believe both of those things. And just because I didn’t share them as my status update doesn’t mean I do NOT agree with the statements.
Education underlies awareness. To even call something a game and honestly believe it’s doing anything to help any aspect of this disease is delusional.
And why would awareness be correlated with something being done secretly?
I think that those of us who have had breast cancer have an obligation to speak out if we disagree with these posts. People look to us to see how we react. If we not only read these updates but share them, it does constitute endorsement. It says we agree. It says it’s okay to think of breast cancer awareness this way.
I say: count me out of these Facebook games.
I have stage 4 breast cancer and it is no game to me.
October 1st, 2013 §
 This is the last photo I took before I found out I have metastatic breast cancer.
This is the last photo I took before I found out I have metastatic breast cancer.
This photo was taken in the final days of September when I went to visit my surgical oncologist for my annual checkup.
I’m wearing a hospital gown with those boots. The contrast of the gown and boots made me laugh.
I snapped the photo.
The actual diagnosis came one year ago today.
It came on the first day of Breast Cancer Awareness Month (a month which has always driven me batty).
It came more than five years after I finished treatment for stage II breast cancer (no, five years without a recurrence does not mean you’re cured, let’s just bust that myth right now. Hormone receptor positive breast cancer in particular can return after 5, 10, 15 years or more).
……
I went to my surgical oncologist annually so she could check on how I was doing after she surgically removed both breasts in January of 2007. After the active post-surgery period, the visits consisted mainly of a physical exam and a talk about how I was doing and what post-chemo treatments I was on.
At this particular visit I complained of some rib pain in a place where I’d broken two ribs in a fall a few years prior. Nothing else was bothering me that day. While I was changing into my street clothes she phoned downstairs to my medical oncologist who said he would put orders in to repeat my bloodwork a month early. It was a test he did every six months at that point.
None of us were worried.
Flash forward a few days to Monday, October 1, 2012.
One of my medical oncologists (I have two, one is a general hematologist/oncologist and one is a breast oncologist) walks into the room with a concerned look on his face and says hello and goes straight to the computer. He starts punching things in to log into the system.
I ask him, “How are you?” “Not so good,” he says. I am sure he’s talking about himself, his family, his favorite sports team perhaps.
“Your markers are elevated,” he says. And only then does he turn to make eye contact with me. I know now, looking back on it, it was too hard from him to tell me. He really didn’t want to deliver that news that day.
When he tells me, he knows I know what that means. We’ve been a team for more than five years by then. He knows I know. It doesn’t need to be explained.
He looks at me while I crumble. And swear. A lot. He comes over to comfort me. I am alone in that room with him. No one expected this to be anything but routine. I didn’t bring anyone with me for the appointment, I almost never had company with me at any of my appointments over the years. That’s how I liked it most of the time. I still do, actually.
But today’s visit rapidly becomes the farthest thing from routine.
……
I wasn’t expecting it. I confess that. The pain I’d complained about a few times during those five years? That pain had never turned out to be anything.
And oh… by the way, that rib pain that I complained about? It actually was nothing. It was just sore ribs from the old fractures.
I was sent across the street to the hospital immediately for a chest x-ray. This looked clear. My PET scan the next day showed no cancer where I’d complained of soreness. But there was cancer elsewhere: in multiple bones and lymph nodes. It really was what we feared. We were lost, falling, reeling, grieving.
Within three days I was having a surgical biopsy through my neck to gather malignant tissue and lymph nodes. Within two weeks of the news I had the true sign that would have taken me to a doctor anyway: bone pain in my collarbone area from a fractured first rib caused by cancer breaking through the marrow into the bone.
I’d have found out within a few weeks that I had metastatic cancer anyway when the pain in my shoulder got severe… which is why some doctors don’t even use tumor marker tests. The marker tests don’t reflect cancer activity for everyone. Physical symptoms are usually quite reliable. And let me also point out that a lot of muscular pain can be hard to distinguish from bone pain depending on location. I’ve had both. And it’s not easy to tell them apart in my opinion.
I went and met with my other oncologist a few days after that.
I started chemo within ten days of hearing my diagnosis.
Things moved fast.
Life changed forever.
……
The weather is changing now. It’s warm this week so I don’t think I’ll be reaching for those boots.
But when the cool air comes again in a week or two or more I am not sure how I will feel when I reach for them.
Right now they just make me feel sick.
September 23rd, 2013 §
 It takes a leap of faith every day.
It takes a leap of faith every day.
Not one of religion– no that’s not in my play book.
But there is a leap that comes when you think to yourself each night,
“The world will be here tomorrow, and I in it.”
Statistically it is likely to be so.
But what about the day after, and the day after that?
How many days do you think ahead?
Have you bought plane tickets for next year?
Planted bulbs for Spring?
Bought an extended warranty on the washing machine?
Three years ago, without even a thought, I took a three year car lease.
Nine months later I received my diagnosis of metastatic breast cancer.
Fifteen months from now that lease will come due.
Will I take another?
I have a car in mind I would love to have…
But can I think of my life in fifteen months,
What it will be,
What will I be?
No, I cannot.
I talk of taking trips in Spring. I have a friend down South I want to visit.
I do believe I will be alive.
But what will my quality of life be?
What chemo or radiation or surgeries will I need by then?
What regimen will I be on and how will I feel from it?
Just being alive is not always enough.
I don’t buy those tickets,
But I do still think the thoughts.
I don’t make promises because I don’t want to cancel.
I say, “Let’s play it by ear,”
“Let’s see how it goes,”
Because to plan, to get hopes up,
To think it could come true…
And then to have them dashed
Would be too hard for me.
I know not everyone shares this view.
The thing with incurable cancer is I don’t have a particular kind of hope anymore:
I can’t have the confidence the suffering will end because it is temporary.
It is not temporary.
I do keep pressing forward though, in my own way:
With strength, with dignity, and yes, still with great hope for more time.
Many days that is one of the hardest things about it all:
I can’t just mark the time and get through
Knowing the hardest parts will soon be over.
Because I know the hardest parts are yet to come.
September 19th, 2013 §
 I’m not about to let myself go.
I’m not about to let myself go.
I’m not about to stop wearing makeup or dressing nicely or styling my hair each day.
I’m not about to relax my standards or let my children get away with things they shouldn’t.
I’m not about to stop being a friend, a daughter, a mother.
I’m not about to stop having dreams.
I’m not about to stop learning, growing.
I’m not about to stop sharing.
I can’t just give up.
I can’t stop moving.
I can’t change who I am.
I know some of these things will change.
I know someday soon I won’t have choices about what I do each day.
I know there will be a day I won’t have hair to style again.
I push myself too hard each day.
I feel I am in a race against a clock.
I must pack as much into each day as I can.
I am in constant motion,
Like a summer child waving her arms to keep the mosquitoes away…
I dance and thrash and run away,
Looking for a place to escape injury where there is none.
I can’t control so many things about having metastatic cancer.
This feeling is one of the hardest things about this disease.
But those things I still can?
I’m holding on tightly onto those,
And I’m not about to let go now.
August 29th, 2013 §
 Remember me pretty,
Remember me pretty,
Remember me whole.
Remember me the way I am today
While friends still honestly say, “You’d never know.”
Let me tell you:
It’s not what it looks like,
It’s not what it seems.
Those times are long over,
Now I am on my own.
The beggars have all ridden.
My wishes: horses gone.
I float above it all,
Watching as I do.
Surrounded by people,
Feeling so alone.
Head down,
At the stoplight tears come,
A young man pulls up next to me
Glances once… twice…
With an engine rev, he’s gone.
I hide it pretty well, you see.
They say, “You look so good,”
“You are so strong,”
But in the space that’s in between
I fall apart
I kick and scream
I claw and grab on for dear life.
Because really,
Truly,
What is happening here:
Choice is gone,
Chance is Queen,
Luck will run right out.
Everyone placed their bets?
Let’s see how far we can go.
August 24th, 2013 §
I had my PET scan on Thursday morning and received the results yesterday. I suppose the best way to simply summarize it is that it’s a mixed bag.
There is mild progression from my scan in April. This means there are more sites of cancer in my bones that are large enough to be detected on these scans (“hot spots”). One hip, one side of my pelvis, one thigh, more tissue and some nodes in my upper chest are all newly affected. Many ribs and one vertebrae continue to be pretty plagued as well but were already lighting up on previous scans.
That said, it is good news that the metastases are still confined to my bones and nodes (honestly, I can’t believe the things I call “good news” these days!). There is no evidence on the scan that it has spread yet to my liver or lungs.
So the scan is overall worse than April but still better than October in that the spots are in the marrow and not eroding bone itself (the fracture I had in my collarbone has healed and the cancer diminished there). This is good and also has the benefit of keeping me mostly pain-free. My chemo causes muscle inflammation which hurts but it’s surely preferable to bone pain. Most other side effects have been the same as before.
So here is where it gets tricky. And if you haven’t figured it out by now, this whole business is quite complicated and full of guesswork. My tumor markers had been rising and it looked like we would need to move to a different chemo. At that point (about a month ago), we decided to increase my chemo dose and see if we could get a response. After two weeks my markers dropped. That was right before the scan.
So, one takeaway is that we are learning that my bloodwork is quite accurately reflecting the cancer’s response to chemo. This is not the case for everyone.
So the million dollar question is: is the scan reflecting the peak progression this time and now that I am on a higher dose of chemo if I continue to have lower markers will we see the scan reflect this in another few months? That is, is the scan showing the worst it got and now with the recent increase in chemo it is actually on a downward trend? That’s the hope: continue to see response. Only time will tell where on that dynamic process this static measure is.
This information puts me in limbo yet again. But that’s really what this world of metastatic breast cancer is. And you know, I would rather have limbo than definite bad news (again, I chuckle at the straws I grasp at here…).
I won’t go into details because this post is growing long, but I did meet this week to discuss possibly enrolling in a clinical trial at Sloan Kettering. This would be a phase 1 trial and would be a strict chemo protocol. I will do a separate post about trials in the future because I think there is a lot to learn about them and also a lot of misinformation about their use with this disease. Bottom line on this particular trial: it wasn’t one I would definitely jump to enroll in. Some additional time to explore it and other options some more would be nice. So “limboland” helps with that, too.
For the next few days (and likely the next few weeks) I will continue taking the higher dose of chemo daily, monitoring the bloodwork every two weeks. I’m having shortness of breath for the first time this week and that is quite unpleasant. It is a side effect of the chemo.
The results are not what I hoped for. But onward I go.
I deal with what is, I adjust to new information as quickly as I can and forge ahead into the unknown.
I thank you for your care and concern this week. As always, it takes some time for me to gather, interpret, and process the information before coherently getting it out to you all.
August 6th, 2013 §
 Hi all,
Hi all,
I may not be posting much this month. Now that all three of our children are home from camp the house is busy and we are readying for school. Public school here starts the last week of August so we have less than three weeks remaining of lazy summer days. I will make sure to post anything important news-wise.
My tumor markers have not climbed any higher in the last two weeks though they still remain slightly elevated from levels a few months ago. Both of my oncologists feel my current chemo regimen of Aromasin + Afinitor is still working. Nonetheless, we would like to see if we can drive the number down further and erase that gain. We are still getting a sense of how much variation is normal with this imprecise test.
Side effects on this Aromasin/Afinitor combo are cumulative in severity, so the longer I am on it, the worse they will become. Currently my major issues are fatigue, immunosuppression (making travel and being in public places risky), mouth and tongue sores, joint pain, muscle aches, skin breakdown, itchy scalp, sun sensitivity, high cholesterol, high triglycerides, increased blood pressure and rapid heart rate. Loss of appetite and associated weight loss are also factors. Yes, I know: to look at me you’d never know all of these plague me. I try not to talk about them too much but they are there.
Because I know many readers will be interested in potential remedies for some of these problems, I should say that I do have all of the treatments I need to deal with these side effects. Some of them are just the way it is, and you have to just adjust if possible. Others like mouth sores and skin/scalp issues can be very successfully treated with topical steroid ointments and liquids (some believe coating the Afinitor pills with food prevents mouth sores but this is actually just a coincidence. It’s not the contact with the mouth that causes the sores, it’s the mechanism of action that does. Blocking the mTOR pathway causes oral mucositis and stomatitis. Starting initially on a smaller dose and working up to the final one does seem to help with the initial outbreak of sores though). Walking helps both the joint pain (despite initial pain) and fatigue, while occasional Ativan helps the blood pressure, heart rate, loss of appetite, and some muscle issues. These are some of a few of the things that my oncologists and I have found to help.
One of my oncologists told me I was “at the precipice” with my side effects; my body could not tolerate a higher dose (currently I take 25 mg of Aromasin and I alternate 5 and 10 mg doses of Afinitor to average 7.5 mg/day). A meeting with my other oncologist today yielded a decision between that I would increase my chemo dose ever-so-slightly to see if I can tolerate it while hopefully get a response.
This type of situation is where the art of oncology comes in. I give a liberal interpretation to the term “art.” I think it’s educated guesswork, creative thinking. The science is the foundation but the application and choices are sometimes educated guesses.
We don’t know if a small increase will affect the tumor markers. It might. It might not. Can my body handle more? That’s an unknown too.
I think of it like the old fashioned scale in the doctor’s office– the one with the weighted bars that you slide left and right until they balance. The nurse gets close to the target, then nudges the bar bit by tiny bit until just the right balance is achieved. This is what we are trying to do: balance quality of life (side effects) with maximum efficacy. Where that line is, we do not know. It varies for each person.
We’ll test again in another week (two weeks since my last one), but it’s unlikely we would see any result that quickly. At least we will see if the markers are continuing to hold steady.
As far as this website, I have many ideas brewing for blogposts soon. Readers have also contributed some great ideas and asked questions that I will do my best to answer.
As always, thank you for the continued support.
July 29th, 2013 §
 A flash of red amidst the green summer grass:
A flash of red amidst the green summer grass:
a lone leaf, blazing in autumn clothing, a vivid premature announcement of a change of season.
Perfectly waxy, thick and juicy, it could not have been there long.
It is, I realize, the color of my mother’s lipstick. The color she has worn every day of my life. Perfectly fitting for the moment…
I turn 44 today.
I do not know how I feel about this fact.
The day I turned 43 was a lifetime ago, surely not just one year. I did not know I had metastatic breast cancer then. I was ignorant and blissful.
I had no idea what my life would be when I reached this birthday.
I have no way to know what it will be when I reach the next. I do believe I will see it though.
I am in limbo at the moment, waiting in the next few weeks to see if my current chemo has stopped working. I do not know if I will need to move on to something else to try to buy myself some time.
That is, you see, my only wish: more time. That is what I wish for today.
Time with my husband. Time with my children. Time with my parents and brother.
Time with my friends.
Chances for memories.
Opportunities for more.
I will keep trying to give a face and a voice to this disease.
There is poetry in the human experience.
I will keep trying to find it, document it, and also help others.
One way I have tried to help is by setting up a research fund at Memorial Sloan-Kettering.
If you can spare a few dollars and want to donate them to research on metastatic breast cancer, you can do so here. I don’t directly ask for donations often, but on this day I will.
I am glad to see 44. But there is inherent sadness in birthdays now.
Cake,
balloons,
the wish that comes true if you just close your eyes and blow out the candles…
if only it were so.
And so there is an anachronistic flash of red,
a moment of color.
I am that leaf,
released from the tree before its time,
floating downward,
coming to rest where it has no earthly business being,
nestled in the green summer grass.
July 5th, 2013 §
 Something happened to my brain when I heard the words “Your breast cancer has metastasized.” Suddenly, irreparably, it became a sieve. Surgical menopause without the option of hormone replacement seven years ago started the process. But mental anguish and immediate, lifelong chemotherapy been major contributors to my Swiss cheese mind.
Something happened to my brain when I heard the words “Your breast cancer has metastasized.” Suddenly, irreparably, it became a sieve. Surgical menopause without the option of hormone replacement seven years ago started the process. But mental anguish and immediate, lifelong chemotherapy been major contributors to my Swiss cheese mind.
I used to read a lot. People think of me as a reader. I am sorry to say I’ve become a fraud.
I love to support authors and their books. That has not changed. It never will.
But when it comes to what I’m actually reading (and finishing)… well, I have a confession to make: it’s not much in the past nine months.
My mind jumps all over the place. It simultaneously wants quiet but is restless. It craves nothingness and distraction. It is hard for me to sustain long conversations; I find them exhausting now. This is one reason Twitter has remained such a wonderful social medium for me; it is defined by short chats that can be stopped and started at will.
When it comes to reading, however, I am having trouble. I hope this ability will return. I spend my focused time writing when I can. Even then, as readers here know, I almost always write brief pieces, expressing thoughts in as few words as possible.
When I was first diagnosed with breast cancer and underwent chemo in 2007 I didn’t read either. I hear from so many people that this is how they felt, too. Those who are newly-diagnosed think they will spend their time catching up on books they want to read during chemotherapy or after surgery. It just rarely happens: either your brain is in a fog or you feel rotten. When you feel good, you want to get out and do things with your family and/or friends.
My current stack of “am reading” and “to be read” is shown in the photo above: books by Dani Shapiro (am reading), Kate Atkinson, Rosie Schaap, and Meg Wolitzer (to be read). I’ve cleared out shelves and shelves of books that I know I won’t get to and given these treasures away. It really made me sad to see so many books there, mocking my isolation: tangible reminders of things I will leave undone. And yet, I saved a bookcase or two of books I still want to read. I won’t give up hope completely.
So now I turn it to you, readers: Do you go through phases of reading? What have you noticed about your reading habits when you had bad news? Health issues? Medical treatment of some kind?
On the flip side, what happened to your reading habits after happy events? I didn’t read after the birth of each of my children: middle of the night feedings were accompanied by nodding off, not turning pages of a book. I’m not an audio book person, I should specify. I know how wonderful this format can be, it just doesn’t work for me. I either fall asleep (chemo fatigue and the sound of someone reading to me… isn’t that how we prime our children for bedtime, after all?) or my mind does its trademark wandering and I have to keep rewinding the story.
The beautiful thing about a book is that it endures. It will wait for you. Like a good friend, when you are finally ready, it will share itself with you.
June 26th, 2013 §
 I’ve again invited my mother, Dr. Rita Bonchek, to write a piece for the blog. Her previous posts on the difference between guilt and regret, grieving the death of a parent, what it’s like to read my blogposts about cancer, and how to help children understand death have been well-received. As a psychologist specializing in grief and loss I think her perspective and ability to share insights are welcome additions to the posts I make. I know that she gains comfort from talking with other parents who have children with cancer and sharing their feelings about the way that cancer has affected their roles as parents (and often as grandparents). Her post appears below.
I’ve again invited my mother, Dr. Rita Bonchek, to write a piece for the blog. Her previous posts on the difference between guilt and regret, grieving the death of a parent, what it’s like to read my blogposts about cancer, and how to help children understand death have been well-received. As a psychologist specializing in grief and loss I think her perspective and ability to share insights are welcome additions to the posts I make. I know that she gains comfort from talking with other parents who have children with cancer and sharing their feelings about the way that cancer has affected their roles as parents (and often as grandparents). Her post appears below.
I think the only thing I would say that I might disagree with here is that I don’t think it has to always be a one way street. Mom refers to a time when I was helping her with problems she had in her own life. Yes, perhaps it’s important to be aware of when you are asking your child for help or advice. However, if this is the way your relationship is (ours is, for example), then I believe that maintaining some of this dynamic adds to the sense of “normalcy” that may be elusive but also can be comforting to both parties. That is, if I am not in an immediate medical crisis, helping my mother with a problem she is having feels good to me, rewarding, reminiscent of the way things were before. If the street is always one way, that adds to the feelings of separateness between us, a strong reminder that everything is different.
A suggestion we both have is to focus more on parents taking care of themselves, finding ways to cope in a way that is right for them. Certainly parents and children do not always have the same strategies to deal with medical crises. The parent also may need support to deal with his/her grief during this fragile time. Individuals may find help in talking to a therapist or other supportive figure or attending a support group for parents.
There are constant ebbs and flows in the parent/child relationship based on how treatments are going, anxiety about upcoming tests or bloodwork, and the side effects of treatments. It may not always be clear how much the parent needs to be parent at any given time. Open communication is so important. One of the hardest conversations my mother and I had recently was one in which I openly laid out some ways in which she could be more helpful to me now. That conversation led to a wonderful new phase of support. She feels good that she knows better what I need, how to be helpful to me and to my family. I cannot expect her to be a mind-reader, and the ways that I need support change with how my treatments are going. I will be undergoing treatment for the rest of my life, so it’s important that we are as honest and supportive of each other as possible. I know that she has her own challenges in dealing with my diagnosis. She feels good now knowing some of the things she can do that are most helpful. I truly believe that is what makes a parent feel good is to know they are a help, rather than an additional source of stress for their child during this difficult time.
My mother and I both hope that this piece will be an introduction to this topic. There is so much to say about changing relationships during medical crises. Perhaps today’s post will allow you to raise some of these topics with a family member.
……………………………………
Dr. Rita Bonchek writes:
Throughout this blogpost, I repeatedly refer to children. Even though adult in years, they are our children. When they are diagnosed with cancer, the relationship between parent and child will, by necessity, change. I would like to suggest how parents can strengthen the relationship and cope more effectively at this time.
When Lisa completed cancer treatment after her initial diagnosis (double mastectomy and chemotherapy in 2007, oophorectomy in 2008), everyone, including her doctors, believed that there was an infinitesimal chance that the cancer would return: that period of time was in the past and life would move forward. When the cancer returned in the form of an incurable metastasis in 2012, we were all devastated.
Families have one type of relationship when all of its members are healthy and a different type when one member is ill. But cancer isn’t necessarily just being ill for a period of time, recovering and continuing on with life. Cancer can be a life and death everyday concern. So, what happens? The conversations change because references to cancer are screened , levity is uncomfortable because how can one laugh about trivial jokes when something so serious is occurring and discussions that involve long-range planning are avoided since how long will long-range be.
Who we were as parent and child before the diagnosis of cancer is not who we are and become after the devastating news. The prior carefree mutual relationship now shifts from both of the parties interacting and sharing problems and concerns to only focusing all attention and sensitivity towards the child. There is now a one-way street. How could this not be? When one asks the question “Whose needs are being met?” it must only be the one who lives with the cancer. The goal is, as much as possible, to reduce stress and tension between mother and child but, most importantly, within the child.
There are some tensions that occur when a parent offers to help a child with household chores, fixing meals, carrying packages, etc. A child’s snappish response of “I can do it myself” may indicate that to accept the offer is to admit a weakened condition. Or, any offer to help may cause reminders that at some time sooner or later that help will be needed. It may be better just to do the chore without asking as in folding laundry, unloading the dishwasher, making a meal that could be frozen if the gesture is not accepted. It is MOST important that we do not take personally such behaviors as negativity or curtness. There can be mis-directed anger at a parent instead of directed, expressed anger at the overwhelming madness-sadness of the cancer diagnosis.
It can be helpful to establish ground rules. The parent can ask “What CAN I do for you that would be helpful?” “What should I NOT do that might be upsetting to you?” Those of you who read this blog-post will surely have suggestions that all of us, who are trying to function each day as best as possible for ourselves and for our children, can benefit from reading.
From the day of the diagnosis, our worlds have changed irrevocably for the worse and we must adjust. I may sound as if I knew exactly what to do and employed suggestions proffered. Not so. Just ask Lisa. I let her down. I had personal problems during the time after her diagnosis of metastatic breast cancer and I vented and asked for her advice as she was trying so hard to just get by.
I felt only Lisa knew the participants well enough to understand my dilemmas and to help me. Time after time, I apologized, I vowed that I would not involve her again and she forgave me. But once was not enough, even twice was not enough, for me to learn my lesson and to seek help elsewhere. If I had remembered to ask myself “Whose needs were being met?,” I hope I wouldn’t have placed Lisa in that position. Our children may no longer be as available to support us.
When I was in practice as a psychologist who specialized in grief and loss counseling, I tried to help my patients to understand, process and deal with major losses. I often explained to them that denial was an effective coping mechanism if it allowed them to absorb the overwhelming loss little by little, bit by bit. But denial cannot be total and the reality of the situation must at some time be acknowledged. So, although I do recognize the possibilities of breakthroughs in medical science, I do not believe in nor count on miracles.
I will let my thoughts go a certain distance into the future when I must, but I function day by day as a way of living . I choose not to focus on what may occur in the future because it may not occur. What a waste of time and energy that would be. I cannot focus on the possible downturns during the treatment, on any pain or suffering Lisa could be experiencing but is not telling me about.
The reality is that though I can support and comfort her, there is nothing I can do to make her physical and emotional suffering go away. If I indulged in this negativity and worry about Lisa in my everyday life, I would have no life. I try to remember- not always successfully- that worrying benefits no one. If my worrying could provide even a tiny extension of Lisa’s life, I would worry myself sick.
A line in Joyce’s “ Ulysses” states this emphasis on the present: “Hold to the now, the here, through which all future plunges to the past.”
To derive satisfaction from life, Lisa and I agreed that auditing classes at Franklin & Marshall College would distract me with an activity that would challenge me and bring me satisfaction. And so it has. The last thing we want our children to do is to worry about us. Whatever we do for ourselves, we do for them. Find some interest or activity that gets you through each day.
Lisa and I have quite different personalities and behaviors. As her readers know, she is very open in describing her thoughts and feelings. In contrast, I was a very private person. When Lisa first started writing, I was uncomfortable seeing private information about our family being disclosed publicly and shared with people I did and did not know. But, very soon, I began to appreciate the role that Lisa’s writing played and continues to play in her life and the lives of her readers. And so I changed and re-evaluated my stance on privacy. In answer to the question “whose needs were being met?” I substituted my privacy desire for Lisa’s openness. I stand with Lisa to help cancer patients and their loved ones live with cancer and not die from cancer.
Our daughter, Lisa, is an incredible daughter, wife, mother and friend. I cannot and will not imagine living my life without her.
June 10th, 2013 §
 I have my list of things I worry about.
I have my list of things I worry about.
First on my mind in the morning,
Last in my head at night.
And if I pop awake In the middle of the night?
Yes, the list is there too.
Across the aisle from me on the train to New York City last time sat a woman.
At one point on the journey she flipped huge black bug-eye sunglasses from the top of her head down over her eyes, her look now an insect dressed in designer clothes.
She reached in her purse,
grabbed a strand of worry beads and started kneading them.
With a rapid-fire reflexiveness she started moving one bead at a time .
Each only moved about half an inch down the string.
From the worry side to the safe side.
I could hear the rhythmic mantra of the beads again and again and again,
Quieter but still audible over the clickity clack pattern of the train itself.
I wondered what her worries were.
I wondered if she would add mine to hers.
Or trade with me, even.
Sometimes we need to do something with that energy.
For her it was tiny movements, thumb and forefinger
Pinching and sliding ivory beads on a round string.
We have our rituals when things get bleak. Some pray.
I do not.
There is a coping that comes with grief, a way to release the tension that grips us when things are bad.
Some days it does feel like it eats from the inside out.
When you must come to terms with what you fear
and what you dread
and all you want to do is lay down on the floor like a petulant two year old
and kick and scream about the unfairness of it all…
As if the universe gives a damn that life hasn’t been fair to you.
Clearly it doesn’t.
So I do not appeal to the universe to change what is.
I turn to my balms. I turn to research.
I turn to science.
I turn to determination and hope which are the last things I can cling to,
fingertip by fingertip,
like the cat on that iconic poster that says “Hang on, baby.”
Inner strength is sheer will.
My claws are firmly entrenched.
There is no other way to be.
There is no justice.
It’s up to me to come to terms with the weighted side.
That is where I live right now.
And so every day, when I wake up in the pre-dawn hours and contemplate my worry list and
come to terms with the day that is about to dawn,
I gather strength,
summoning it from its slumber.
“Here we go,” I say.
“Let’s do this.”
Another day is here.
I will see another.
Hang on, baby.
June 8th, 2013 §
 Two weeks ago we had a family photo session with my friend Julia Arstorp. Julia has taken numerous series of photos of us through the years and I really wanted to have updated photos of all of us. The children have changed so much in the past two years! I will share some of them throughout the next few months. I have updated my Welcome page of the blog with a few of them too. I know some of you only read these posts by email so you can always take a peek at the home page to see what’s new.
Two weeks ago we had a family photo session with my friend Julia Arstorp. Julia has taken numerous series of photos of us through the years and I really wanted to have updated photos of all of us. The children have changed so much in the past two years! I will share some of them throughout the next few months. I have updated my Welcome page of the blog with a few of them too. I know some of you only read these posts by email so you can always take a peek at the home page to see what’s new.
One of the photos I love most is this black and white one with our new dog Lucy, a Pembroke Welsh Corgi that we got in January. If you follow me on Twitter you know how much I love her. She is my first dog ever… the kids always wanted a dog but I wasn’t sure about the commitment. Clarke had a great Corgi named Pearl when we met so I knew the breed and loved their personalities. Lucy is two now and she has brought such joy to our lives.
 Most people who know me are shocked I not only let Lucy on the bed and throughout the house. My attitude is she is a part of our family so she gets to share. She’s not a big snuggler (prefers to lay next to you or under the bed) but we have had some great naps together over the past few months. She is great at fetch which is a lot of fun to watch as her little legs run so fast and her big ears get pinned back to her head as she scurries… she is fast on those little legs!
Most people who know me are shocked I not only let Lucy on the bed and throughout the house. My attitude is she is a part of our family so she gets to share. She’s not a big snuggler (prefers to lay next to you or under the bed) but we have had some great naps together over the past few months. She is great at fetch which is a lot of fun to watch as her little legs run so fast and her big ears get pinned back to her head as she scurries… she is fast on those little legs!
The end of the year is very busy now with school ending for all of the kids. Colin will graduate from elementary school and start at the middle school in 6th grade in the fall. Tristan will be going into second grade and Paige will be a high school sophomore (eek!). Right now we have baseball playoffs, karate belt testing, and some upcoming visits from family.
I’ve been managing the side effects from the new Aromasin/Afinitor regimen pretty well. Right now I’m still on 7.5 mg of Afinitor a day, my biggest problems from the drug combo are severe muscle and joint pain, thyroiditis (I also have Hashimoto’s Disease), loss of appetite with weight loss, and migraines. The mouth sores and head irritation have improved.
Bloodwork yesterday showed a drop in my tumor markers, an indication that it is still working now after about 2 months. This gives me a two week reprieve in worry. I really do live in two week increments right now. I’ve been able to do all of the things I need to do and most of the things I want to do. I am learning more and more the difference between these two things.
 I’ve attended every single one of Colin’s baseball games. I got all three of them to the dentist for checkups and their regular doctors’ appointments. I keep a regular schedule right now but try to rest more on weekends when I can. I am glad for the normalcy that my days mean to them and to me. We all know it’s not truly normal, of course, but the comfort of routine is real, especially to them. I find it hard to believe the last 8 months have been since my diagnosis of metastatic breast cancer.
I’ve attended every single one of Colin’s baseball games. I got all three of them to the dentist for checkups and their regular doctors’ appointments. I keep a regular schedule right now but try to rest more on weekends when I can. I am glad for the normalcy that my days mean to them and to me. We all know it’s not truly normal, of course, but the comfort of routine is real, especially to them. I find it hard to believe the last 8 months have been since my diagnosis of metastatic breast cancer.
I gave an interview to the Daily Beast this week about Komen’s cancellation of many of their walks this year because of drops in funding despite Nancy Brinker giving herself a pay raise to $685,000 a year. I wish the piece had gone into more depth about the lack of funding for metastatic research, but I still think some good points were used from the interview. You can read it here.
If you are looking for a place to donate money for breast cancer research, I do have a donation page at Sloan-Kettering which funnels money to metastatic breast cancer research. You can see the page here. It has raised about $17,000 since last fall.
I hope you all have a good weekend.
Find a bit of joy in the world. Share it. If you can’t find it, create it…
June 4th, 2013 §
 I just want to see my son play baseball,
I just want to see my son play baseball,
Watch him wave at me when he’s on base.
I just want to take my daughter shopping for makeup,
Applying powder to her porcelain skin.
I just want to read with my youngest one,
Snuggled up in bed together turning pages of a book.
I just want to grow old with my husband,
Continue to share our lives as we have for twenty-two years already now.
I just want to sit in the garden when we are old.
I just want to talk about the good old days.
I don’t want to read about mTOR inhibitors or side effects or months of disease-free progression.
I want to read beach fluff and skim through cheesy magazines.
I want to get a pedicure and have a nap in the chair.
I want choosing the color of my nail polish to be the toughest decision I have to make for a day.
I don’t want to read reports from the ASCO conference or tweets about new research findings.
I just want it to go away.
But it can’t.
It won’t.
I will never know another day of my life without metastatic cancer or chemo or treatment or dread.
But I will search for joy.
I will.
I will do what I can every day to find that joy,
And if I can’t find it I will make it.
This is my pledge,
This is my promise.
For them.
Some days it is hard to do.
Some days fear and sadness are too much.
Some days I do not know how I will do this with grace,
But I will try.
I must make the most of this time:
Helping others, educating, writing.
I know no other way to do this.
But it’s the hardest thing to do.
I cry, I give in to the emotions, but only for a few minutes.
No good can come from that.
I gather strength.
I re-commit.
I go on living.
The bad days will come someday.
But that day is not today.
That time is not now.
And so I am a parent, a wife, a friend, a sister, a daughter, a writer, and everything else I have been until now.
That is who I am.
That is who I will continue to be.
For as long as I possibly can.
May 31st, 2013 §
 This afternoon I will attend my youngest child’s Field Day. It will be a steamy 93 degrees here and I will join parents as we stand around and chat while we clap for our children and hug their sweaty bodies and remind them to drink lots of water.
This afternoon I will attend my youngest child’s Field Day. It will be a steamy 93 degrees here and I will join parents as we stand around and chat while we clap for our children and hug their sweaty bodies and remind them to drink lots of water.
It is always in these group events that so many of us feel like outsiders. It is often when surrounded by many people we are most aware of being alone. For me, this has never been more true than during the past 8 months since my diagnosis with stage IV breast cancer.
I return again and again to the desire to escape, the need to flee, the pull toward being somewhere else. The refrain in the new song I am co-writing with Doug Allen is about this need we all have, regardless of the cause, to take moments during the day where we just “check out” for a bit. It says:
I take a trip inside my head,
I don’t know where I go.
Somewhere else,
Anywhere else,
Far from things I know.
There are days when I want to be the ostrich, when I just am so overwhelmed with things that I can’t be on social media, returning emails, or even talking. I just am still. I notice that I rarely read anymore, even television can’t capture my attention. I sit in silence a lot, and when I have the opportunity I write or work on the songs.
I take those trips inside my head.
The pull of educating and informing is too strong to allow me to stay hidden away, though. Social gravity pulls me back. Sharing and documenting fuel me. I take my anger, my sadness, and my grief and I send them out into the world in constructive words and deeds. I can feel powerless and without control in many ways about what is happening to me but I always feel that I can control my reaction to these things. This is my lesson to the people in my life.
There is a scene in the film Children of a Lesser God where William Hurt’s character jumps into a pool to try to experience utter silence the way that his deaf girlfriend does. He wants to know what that feels like. He quickly realizes, however, that this won’t work. He knows when he rises to the surface he will once again hear sound. He can’t live what she lives. He can’t share her loss in that way.
Antoine de Saint-Exupery wrote, “It is such a secret place, the land of tears.” Most mornings I stand in the shower for a while longer than I need to. I listen to the water, I think about the day, I am grateful to have another. I know I will have more days. For those few minutes I take a trip inside my head. I gather my strength, I focus on the work to be done.
I turn off the water, I step out of the enclosure, and I rejoin the world of the living. That’s what I am doing every day: living with metastatic cancer.
May 27th, 2013 §
Today is Memorial Day. Each year my letter to troops stationed overseas is similar. Each year I question whether I should write something new, if it’s “cheating” to say the same thing. In the end I realize that thank you never gets old, it never needs to be re-written. Thank you doesn’t have an expiration date.
This year we went to buy items for the care package drive sponsored by the Darien Little League. Volunteers collect supplies including toiletries, non-perishable food, and games and send them to soldiers far from home.
My letters always have the same theme: bravery– chance or choice? I don’t know if the soldiers find my musing on this distinction weird in a letter, but they must ponder the topic of bravery as often as I do.
………………………………………
May 27, 2013
Dear Servicemen/women,
My family and I are sending you some supplies on this Memorial Day Weekend. We want you to know that we have not forgotten you or the sacrifice you are making every day to be away from your own families and in harm’s way. It’s not much, but perhaps knowing you are in our hearts and minds will help.
Six years ago I was diagnosed with breast cancer. I was in remission for more than five years and now my cancer has metastasized to my bones and lymph nodes. It’s not curable. As I go through treatment, people called me brave. I don’t think I deserve it. “Brave” is not a word you used about someone like me. I have gotten cancer by chance and I am dealing with it, the best I can.
But soldiers? You are brave. You have a choice—you put your lives on the line after making a conscious decision to do so. You know the danger and you do it anyway. To me, that is true bravery, true heroism.
Seeing danger and making the choice to proceed anyway is precisely how I define bravery. We all find ways to deal with the fear of death. We know the uncertainty that lies ahead. We see the bravery in others before we will see it in ourselves.
What underlies bravery: chance or choice? Can both?
Are we just hesitant to see the quality in ourselves? Are we just modest? Do we just act the way we need to, to get the job done?
I think when you choose to throw your hat in the ring, that choice counts for something.
That makes you brave.
That’s what makes soldiers heroes.
Happy Memorial Day to you. And thank you for your continued service to our country.
Lisa Bonchek Adams
May 24th, 2013 §
 It’s Friday! I want to put a post up today because I know it’s been a while and people worry when I am not making posts. All is fine, it’s been a very busy week with a lot of routine medical appointments. Side effects from the new chemo are starting in and phrases like “mouth sores”, “high cholesterol,” and “follicular head pustules” make me certain that the person who called it “crazy, sexy cancer” was delusional about what cancer really is. There’s a lot that’s crazy but I don’t personally find a lot of sexy in it.
It’s Friday! I want to put a post up today because I know it’s been a while and people worry when I am not making posts. All is fine, it’s been a very busy week with a lot of routine medical appointments. Side effects from the new chemo are starting in and phrases like “mouth sores”, “high cholesterol,” and “follicular head pustules” make me certain that the person who called it “crazy, sexy cancer” was delusional about what cancer really is. There’s a lot that’s crazy but I don’t personally find a lot of sexy in it.
I’m getting help from my team in dealing with all of the side effects and have more appointments with more specialists in the next few weeks. For now things are stable and the next two weeks will proceed as planned. I’m still on Aromasin (25 mg/day) and Afinitor (7.5 mg/day). It’s the Afinitor that’s kicking in with my various problems. My tumor markers have shown a response to this combo over the last 6 weeks so we continue with it for now. I also received my monthly injection of Xgeva to strengthen my bones.
I wish you all a good Memorial Day weekend, especially our military personnel and their families.
The photo above is from 2002 by the way… where have eleven years gone?
I also want to mention that my last post, “There’s No Room for That in This (Six Minutes)” is the foundation for what is now a song titled “Six Minutes.” Over the past few weeks musician Doug Allen and I have been working hard on it and we’re almost done. I wrote the lyrics and he found the perfect music to bring those words to life. We are both so proud of the song and will be sharing in the future. His latest CD is available now and I just love it; it has two songs that have been on movie soundtracks… who knows where “Six Minutes” might land! More to come on this project.
………………………………
I get a lot of emails and comments with questions about cancer and how to help those who have it. Let me say clearly that I never think I speak for everyone with cancer. I do believe that asking questions is good, and even if you don’t think my answer is right for you, at least you might look at the issue a different way and clarify your own thoughts.
If people like this format I may continue to post letters/responses more often. I have often thought we need a grief/loss/illness etiquette column and I’ll gladly do my best to help.
This week I received the following excellent question.
……………………………..
Hello…
I’m a 31 yr old only child whose mother was just diagnosed with squamous cell carcinoma a week ago.
I’m going home for the first time (parents in WI, I’m in IL) since the diagnosis and after reading this blog, I’m not sure what I should say to her. She is a pessimist by nature and already saying she would refuse chemo (the details of her condition and treatment plan are still in the works) so my dad and I need to figure out a way to keep her positive so she can indeed have the support she needs to fight it. I bought some colored paper and was going to list “reasons why you are a fighter” as well as post some motivational sayings/quotes on their bathroom mirrors, but the ones that came to mind now seem like the ones you SHOULDN’T say “you can do this,”,”stay strong,”
Do you have any suggestions on what I could write? Please keep us in your prayers, I am obviously terrified of the road to come.
—– J
……………………………..
My response:
A few quick thoughts for you, J. I am so sorry about your mom’s diagnosis.
My first thought is that you all need time to adjust to the news. The way you react initially is not always the way you feel once you get your feet back under you. She needs a bit of time to not only adjust to the news but also to make this treatment plan. She doesn’t even know yet what she will be potentially recommended for treatment and yet you are expressing desires to coach her on how to feel.
Being supportive does not necessarily mean keeping her spirits “up.” Maybe what she needs right now is support for how she actually feels, not pressure to be acting a certain way. The best way to support her is to listen to her, and not try to tell her how she should feel. Let her adjust. And most importantly, respect whatever she chooses.
We love our families more than anything, but it’s her choice to make how she wants to live her life and how she wants to treat her cancer. It’s enough to deal with these diagnoses without feeling you are carrying the emotional burden of your loved ones on your back too. It will mean that she will know everyone rises and falls on her actions. That’s a huge weight above and beyond the physical and emotional toll she will be going through.
One of the most important things to do is to ask her how she thinks you could help her the most. I have a feeling putting up signs is not it, especially if you say she is a pessimist by nature. Signs around the house won’t change her attitude if a lifetime of experiences haven’t. Loving her, spending time with her, helping her with things that she might have trouble doing… those might be better. The key is to ask, really listen, and then respect what she says. Her needs might change (doesn’t want or need help now but needs it in the future) so you have to ask again during treatment.
If she decides to refuse chemo it will be tough, but it’s her choice. Chemo is very hard and is a quality of life issue too. Depending on what they are recommending and what the ultimate details of prognosis are, it’s important to respect what she opts to do while still encouraging her to see the benefits (as described by her doctor).
Those of us with cancer know everyone wants us to be “strong” and “positive” but it’s what we need to hear the least. It’s not like we haven’t thought of that already; it often just makes us feel like people are telling us how we should act because it makes it better for them if we act that way.
Negative emotions are normal with cancer, especially only one week after diagnosis… how could they not be? Not feeling free to express them may just be one more way she feels burdened by this disease right now.
Clearly you love her and want to help. The fact you are concerned with the best way to support her shows wonderful affection. The best way to do that right now, so soon after diagnosis, is to ask, and then respect what she says… That’s my best advice right now.
She will need time, but ultimately I think that she will be grateful for being allowed to express her emotions both negative and positive. I wish you all the best. Please keep us posted.
May 15th, 2013 §
 I find myself in silence a lot,
I find myself in silence a lot,
Tuning out the noise.
No room for anything but thoughts.
I try to forget for a few minutes,
I stare at a spot on the wall.
I lose myself.
No clue how long it has been.
The clock says it’s been six minutes,
I am glad that they’ve gone by.
But then I realize I have wasted them:
Six minutes of my life.
I want them back,
Feel I should use them for something better,
Something constructive.
I am mad at myself:
That was a waste of time.
I want days of suffering to pass,
But I also know that this is the only time I have.
I take a trip inside my head
I don’t know where I go.
Somewhere else,
Anywhere else,
Far away from here.
If you’d let me, I would run away,
I would go find a way
To keep you safe from this,
Safely far from this.
Some days I long to tell you how I truly feel,
But there’s no room for that in this,
No room for that in this.
It is not a choice.
That I know.
And when I finally do go
It won’t be for lack of want, or heart, or strength.
When I die it will be because that is what cancer is,
This is what cancer does.
And when it comes to being fair,
There is no room for that in this,
No room for that in this.
May 10th, 2013 §
 My mother, Dr. Rita Bonchek, is a psychologist who specializes in grief and loss. A career discussing death and dying, however, was insufficient preparation for hearing the words, “Mom, I have metastatic breast cancer.”
My mother, Dr. Rita Bonchek, is a psychologist who specializes in grief and loss. A career discussing death and dying, however, was insufficient preparation for hearing the words, “Mom, I have metastatic breast cancer.”
Mom and I have reacted very differently to the news of my stage IV cancer. I was online within days writing posts about the steps I was taking. I wrote immediately about how to help children in the days following a diagnosis like mine. As my readers know, I’m very open about this part of my life.
My mother, on the other hand, is much more private. She would never write a blog the way I do. She didn’t want to share this news with people; she wasn’t ready to talk about it. I respect her decision but that approach doesn’t work for me. Sometimes our different ways of thinking lead to disagreements. Despite our differences we always support each other.
I thought it might be helpful for readers to hear what she has to say about reading my posts. Some of us with cancer choose to be very public with our daily lives but our parents are often forgotten in the discussion. I think the timing of Mother’s Day weekend is perfect to share this piece. I love you, Mom (photo at left: 1970).
…………………………………….
 I am Lisa’s proud mother and I have followed her blog from its first day. As her mother, I read her blog from a unique point of view, and I want to share my perspective with you.
I am Lisa’s proud mother and I have followed her blog from its first day. As her mother, I read her blog from a unique point of view, and I want to share my perspective with you.
Those of you who are reading this blog follow Lisa and her incredible writing. It is her understanding of human behavior, her expression of feelings of her heart and thoughts of her mind that make so many people want another blog from her as soon as the one being read is finished.
Yet, as the mother of this outstanding-in-all-aspects daughter, my reading of Lisa’s blogposts is complicated because each piece contains an extra layer of heart-wrenching pain for me. Lisa’s blog is a precious sharing of her everyday life, of medical explanation and analysis of each and every test result, of measured consideration of her hopes, fears, etc. Parents rarely get the opportunity to get “up close and personal” to this extent with a child. As Lisa’s mother, knowing her innermost thoughts is a gift and a curse.
If you (or anyone else but Lisa) were writing about a life journey with a cancer diagnosis, I could handle reading about the physical assaults on your body and the emotional assaults on your psyche because I would be more objective and not involved in your everyday life. I could read your blog, feel empathy and sorrow for the diagnosis, but step away from it. However, I am enmeshed in Lisa’s writing.
Lisa’s father stopped having the blogposts sent directly to his e-mail because he was often caught unaware with heavy emotional subject matter arriving at inappropriate times. He now accesses the blogposts only when he feels emotionally prepared for whatever he may find.
While this would also be a very reasonable decision for me to make, I have the ambivalent feelings of wanting to be close and share every moment of what Lisa thinks and feels at that moment versus retreating from the declarations of how her life is now and her fears for the future for her and the family – her family and my family.
Lisa and I share the personality trait of always wanting to know the truth so we are as well prepared for the worst as we can be. Lisa and I promised each other that we would never withhold any information to protect each other. The honesty Lisa promised me is the honesty she has promised to all of you, her readers.
On one level, her blog reveals to me everything I want to know, but on another level what I unconsciously don’t want to know. This emotional see-saw of wanting to read it but not wanting to read it is a decision that I must make each time a new blog-post appears in my inbox.
Why is this “to know or not to know” decision so difficult for me? When I read Lisa’s writings, I imagine the sub-text that she does not reveal: how she is managing to keep her family’s lives as “normal” (whatever that means) as possible.
Lisa is, as most mothers are, the hub of her family’s life. When Lisa writes in a blog-post that she was very tired and rested for hours, I know that her closed bedroom door makes every family member who sees that closed door go into overdrive with founded or unfounded concern and fear.
Lisa and I share the goals to make the most of each day and to cherish and to love one another. These are life affirmations within our control when so much of life is out of our control. Share our goals as you and I, Lisa’s readers, benefit from Lisa’s greatest gift to us: who she is and how she lives her life, in sickness and in health.
May 2nd, 2013 §
I have my father’s walk,
A slow, deliberate, long-gaited stride.
I have my mother’s smile, her voice, compassion.
I can’t yet see myself in my children,
I wonder if it is always that way.
I remember as a teen the day I actually could match my father stride-for-stride,
My smaller feet dwarfed by his size 13 shoes.
I remember thinking I was a grownup then.
I was wrong, of course.
I had no clue what being an adult was.
I learned.
Yes, I did.
I yearn to go back to those days,
Perhaps I was not carefree but I was taken care of.
Knowing my parents were in charge,
I felt safe, protected.
Now I am a parent in charge,
I must be ready.
My children try to match my steps, still unable to.
I yearn for the day they can.
I hope I will be beside them when they are old enough to mirror my stride.
Not just beside them in spirit.
That’s not enough.
I want more.
When they think they are grownups
I want to be there too.
April 28th, 2013 §
 It is easy to be happy when you are healthy.
It is easy to be happy when you are healthy.
It is harder to know that this may not be true much longer.
People love to casually say,
“Enjoy every moment” or
“We all die some day anyway” or
“Life is fleeting.”
I know this already.
And I know it in a different way.
I don’t need to be told to
fight the good fight to beat it
or the key is to just stay strong
or that it’s mind over matter
or that I should pray for a miracle
or that I will be cured.
That’s nonsense.
Scientifically impossible in my case.
And so, when you say,
“No, that can’t be true.
There must be something that will cure you,
If you want it/pray for it/think it will be so,
You can be healed,”
What you do is force me to assert my knowledge,
Insist upon my diagnosis,
Explain the desperate nature of my disease,
Spend my time defending my sentence.
I know it’s what you wish.
I know you insist because you want it to be the case.
I know you’re grasping at straws,
Wanting to reassure yourself that bad things won’t happen to you,
That bad things don’t happen to good people,
That something awful won’t happen to me.
Trust me, I wish for it too.
But these things do happen.
It has happened to me.
The truth is that wishes don’t count for anything when you’re placing them against cell biology.
I know many healthy people who say the passage of time is bittersweet.
It isn’t a competition but I can tell you that this passage of time is different.
If you could feel it for just a moment you would know.
There is a difference between
Distant,
Hypothetical,
Potential,
Maybe…
and reality.
I have learned that being nervous about test results,
Worrying,
Wondering,
are not the same as the reality.
Reality is having your oncologist walk in the room
and when you say to him, “How are you?”
and he says, “Not good,”
you naïvely think it must be a problem with him,
or his family and
instead he ducks his head,
takes a breath,
looks at you, and says,
“Your test results were not good.
Your tumor markers are up.”
He knows I know what this means.
He waits for a moment and says,
“I think you have a metastasis.”
A few minutes later he says,
“You need to go get a chest x-ray right now.
Go across the street,
I will come over to the hospital and look at it immediately.
Wait for me there.
Then you need to schedule a PET scan as soon as possible.
Have you had any other unusual pain?
A cough perhaps?”
The room spins, the world stops.
My life didn’t end in that moment, but life as I knew it ended for sure.
No turning back.
Reeling, processing, shock.
All you can do is let your jaw drop,
the tears fall,
your body shake,
crumple.
Slowly,
deliberately,
as I looked at him
in a way that I never had in the six years he had been my doctor,
the only words that came to my lips in response
were to repeat over
and
over
and
over
and
over
again:
“Fuck. Fuck. Fuck. Fuck.”
Because that’s the only word that could capture how angry
and scared
and angry
and surprised
and angry
and shocked
and angry
I was.
I never have liked the term “to expire” rather than “to die.”
I started thinking about these words though.
We all have an expiration date.
I’ve never thought of it like that before.
We all have one.
It is as if I’ve grabbed a carton of milk without looking.
I took the one in front I guess,
The one with the rapidly approaching date they put conveniently at the shelf’s edge for people to grab when they’re not paying attention.
Except I did pay attention.
I did.
I was always paying attention.
No one was more vigilant than I.
I want to put this carton back,
I want to say it’s not mine.
I want to scream it.
This must be for someone else.
The date is too soon but I can’t trade it in for a new one.
No givebacks.
The problem is
I don’t know exactly what the date says.
April 18th, 2013 §

I sit on the beach, feel the sand’s angry texture rub my chemo feet in a way I wish it wouldn’t.
I watch my family in the ocean, turquoise and calm and vast.
My husband flips over, face in the water, takes some strokes out to sea. His movement is graceful, effortless, just as it was the when I met him 22 years ago.
He was a sprinter on the college team then, and while he laughs and says it doesn’t feel effortless anymore, nor perhaps fast, it does not matter. In my mind’s eye he is that young man, swimming fast, joking with his team, coming over to the stands to talk to me while chewing on the strap of his racing goggles. I fall in love with him again every time I see him swim.
My three children float, bobbing in the ocean water.
I can feel the distance between us, it feels like a lifetime.
It is my family in the ocean floating away from me.
I see the quartet, I watch as an outsider.
I do this a lot lately. I watch them from afar and think how it will be without me. A new family unit. Behind the big black sunglasses my tears stream down.
Suddenly Tristan is running from the water to me, across the sand. He stands, dripping, face beaming. “I just wanted to tell you I love you, Mama.” I take his picture. I capture the sweetness. I grab him, hug him, feeling the cold ocean water on him, melding it to my hot skin. I murmur to him what a sweet boy he is, that he must never lose that. I send him back to the ocean, away, so I can cry harder.
By the time they return to shore I’ll have myself composed. But my oldest immediately senses something amiss. She mouths to me, “Are you okay?” And pantomimes tears rolling down her cheeks.
Yes, I nod.
I walk to the water’s edge to prove it.
April 11th, 2013 §
A quick update. I’m sorry to say that my hand-wringing and concern in my last post were met with unfavorable results yesterday. My tumor markers were again slightly higher. In and of itself (an isolated rise) it would be acceptable. But this has been a trend for long enough that it’s evidence my current chemo has failed. Goodbye Xeloda. I’m sorry to see you go. I’d hoped for longer than six months on it for sure.
I’ve got a PET scan early this morning (Thursday). It is being used as much to see how much progression there is as to be used as a baseline before starting the next treatment.
I’m still talking with my oncologists about what the next treatment should be (options include oral anti-hormonals and various IV chemotherapies). Whatever I choose will be ripe with new side effects and demand monitoring. My hands will improve; much as I am happy about that, I am truly sorry to see the Xeloda go. I think you always want to hope that the first thing you throw at this disease will keep you stable for longer than this. But, the Xeloda did good work for six months. But we knew this day would come: on to the next.
I am glad there are still things to try. But of course, for now, I’m sad.
I’m still grieving and angry and all of those emotions. But I’m also learning new skills of compartmentalization and recovery. I move forward, I move on, I live. There is no choice. I change treatments and see what I can get from it. My life has become a puzzle shifting pieces; we move and mix them around until they fit. That fit won’t last, but hopefully it lasts for a while.
Do not be concerned if you don’t see a post for a bit. I’m going into research and decision-making mode. I appreciate all of the support from everyone. I know that if hopes and wishes and hugs could cure my cancer I’d be healthy for sure. I can’t acknowledge all of the messages right now and even the thank you notes for Tristan’s birthday party are sitting half-done. For now this is what I am focusing on and being every bit the mom and wife that I can be at every other moment.
April 9th, 2013 §
 In the still of the evening I hear the frogs waking up to Spring.
In the still of the evening I hear the frogs waking up to Spring.
I hear the creak of the floor as my daughter walks around her room,
Sets things just so,
Murmurs to our dog.
In the still of the evening I hear a car,
A train,
A neighbor calling his own dog home for the night.
In the still of the evening my mind wanders again.
Back.
Always back.
I finished my 13th round of chemo 48 hours ago.
I wonder what is going on inside my body.
I wish I could see.
I wish I knew.
Is it working?
Is this round the one that will show evidence of chemo failure?
Will I move on to a new treatment?
One step closer to the end?
Every time I bang against something,
Every time I feel a twinge,
Every time that fractured bone aches,
I pause.
The pauses add up to moments.
The moments add up to minutes.
I reel them back in like fishing line, I show them who’s boss.
Just listen, I say.
Listen to the frogs. The creaks. The murmuring. The train.
Just listen.
Just hear the quiet,
Hear the house going to sleep for the night.
Feel the love.
Be grateful you can.
April 5th, 2013 §
 For those who wanted to hear my interview on Doctor Radio and weren’t able to listen on Wednesday, here is a link to a downloadable audio file of the one hour show. Thanks to my brother, Mark, for doing this. That show leads directly into today’s discussion.
For those who wanted to hear my interview on Doctor Radio and weren’t able to listen on Wednesday, here is a link to a downloadable audio file of the one hour show. Thanks to my brother, Mark, for doing this. That show leads directly into today’s discussion.
……………………………..
I always get some heat about posting essays about the stupid things people say to those with cancer.
I know people come here expecting to learn. That’s what I’m trying to do: educate. People inevitably vary in their responses to what people say. After all, responses to books, movies, and comedians are all over the place.
Occasionally people will get defensive and say, “Well, I have said one of those ‘stupid’ things and I meant well.” I am going to take an unpopular stance and say that meaning well isn’t always enough.
Maybe the listener is scared. Maybe they’ve had cancer or a family member with it. Maybe they are just uncomfortable talking about illness and death. It’s important to remember: it’s not about you. It’s about the person with the illness. If you are a friend you will need to get over your discomfort or get out of the way. What you don’t want is for the ill person to have to be consoling the listener or trying to minimize the seriousness of what they’re feeling.
Do not turn it back on you, or when you had cancer, or when your child or mother or 2nd grade teacher did. It’s not necessarily the same. Types of cancer are not the same. Even subtypes of cancer are not the same. Now, I’m not saying you should always avoid interjecting something to let the other person know that you’ve had experience with cancer. But the first thing out of your mouth shouldn’t be to connect it to someone else and what their outcome was, good or bad.
Different diseases cannot be compared. Different cases of the same disease cannot necessarily be compared, either. Chiming in with, “Oh, my second cousin’s boyfriend’s dog walker had breast cancer” doesn’t help a person, especially if it’s followed by “She suffered in pain for a long time and died” (yes, this gets said more often than you can imagine). The other end of the spectrum is, “Oh I know someone who had that. They’re fine now.” (Okay, but some people are not fine… should they be jealous? Feel inadequate?) Someone told me in response to learning I had metastatic breast cancer that his wife “had a bit of that last year.”
If you had a coworker who worked the entire time she had treatment, that’s great. We are happy for her, truly. But that bears no relation to how someone else can handle their surgeries, treatments, and side effects. So while you might think it’s supportive (in your mind you’re saying, “See, I’m being supportive and reassuring her that it might not be as bad as she thinks”) what that person may reasonably hear is, “Wow, if you have to take time off work you are weak, or at least not as strong as my coworker was.”
What would be something better to say to a coworker? How about “Please tell me how I can help you during this time. Is there something at work I can do to make it easier for you? I hope you know I would like to help if I can. If you can’t think of anything now, that’s okay. Just let me know if/when you do. I’ll ask again to make sure you’re getting the help you might need.”
Asking “Has this been a good week or bad week for you?” seems like a good bet to ask someone you might not be best friends with. It shows concern and they can be as detailed as they want in their response.
…………………………..
A few weeks ago someone tweeted to me, “As a cancer survivor myself, I know that half the battle is the mindset. Be determined to defeat cancer and you will!” Then followed that one up with “I meant that if we believe we can win against it, we will.”
Comments about someone’s attitude are definite don’ts. Does that mean those who die every day are responsible for their deaths because they are weak-minded? If it were as easy to defeat cancer as mindset, people would not die of it by the thousands every day.
Similarly, comments about appearance while rampant, can strike the wrong chord. I can’t tell you how many times people find out about my stage 4 diagnosis and say, “But you LOOK just fine!” The two are not always correlated, most especially at the time of diagnosis. This is why many people don’t know they have cancer and are completely taken by surprise. When people tell me “You look great!” I know they mean something nice by it. But the rest of that comment, the dark underbelly, is “You don’t look like you’re dying” or in some ways more insidious, “If you look that good you can’t possibly be that sick/it can’t be that serious.”
Don’t say you know exactly how someone feels if you don’t have evidence to back that up. Being a compassionate person and caring friend does not require personal experience that is identical to what the person is going through. Let me say that again, a different way: in my opinion you don’t need to have had cancer to be a caring friend. It might help you to be a good friend if you have had cancer, but it’s no guarantee. People “do” cancer differently. While the experience might have similarities, it doesn’t mean we will necessarily agree on how to deal with it. Part of what I try to do here is level the playing field. I try to bring you information and advice you can use so that you will know more about helping than you did before.
Don’t tell them that their science-based treatments are bunk and what they really need to be doing is just changing their diet, breathing pure oxygen, or relieving their constipation to be cured of cancer. Do not tell someone who is in the middle of treatment that chemotherapy is a waste of time. You may think your suggestions of supplements/vitamins/tea are harmless, however, there are serious interactions that can dull the effectiveness of chemotherapy and other treatments. Not all lotions are good to use during radiation treatment. Not all vitamins are good additions.
………………………….
I like what @travisbhartwell tweeted to me: “Mindset changes the days you have, not the number of days you have.”
The worst thing that can happen is that friends disappear. This is happening to me in spades. It may be that they are afraid they’ll say the “wrong” thing and end up being written about. But I think it also has to do with the fact that death and illness make people uncomfortable. I represent their fears. People who should be in touch with me at least every week or two (because that is how often we saw each other before) have just dropped away.
That said, there are so many people in my life who are so wonderful. Who offer to help, who make it easy to accept it. Who send notes or emails of support months after the initial shock. Who keep asking what they can do. Who pointedly give ways they can help and ask if I could use it.
………………………………..
One thing I think is very important is to always say to someone who is ill or has experienced a death in the family: do not write me a thank you note for this. Do not feel the need to answer this email. Do not feel the need to call me back.
If you live near the person ask them, “Would it be helpful if I texted you before I run errands so that I can pick something up for you?” Texting and email help because talking on the phone is almost always too much of an ordeal and/or inconvenient. I have friends who email me at the beginning of the week to say, “I’ll be at the grocery store, the drugstore, and the post office this week. Can I do anything there for you?” Some will text on the spur of the moment, “Running to Costco. Need anything?” These are invaluable offers.
If you have no knowledge of what information you are being told, admit it. People with serious illnesses do not expect you to know everything about their new diagnosis. They are probably learning a lot of information in a short period of time and may not even know the details of their diagnosis and treatment. They don’t expect you to have the knowledge but you need a way to connect. I recommend when someone tells you about a diagnosis you don’t know much/anything about you say, “I don’t know anything about what that diagnosis means. Would you mind telling me about it, and what it means for you?”
How is it affecting your day-to-day life and what part of that can I help you with?
I’m so sorry to hear that.
What is the worst part of this for you and how can I help make that a bit easier for you?
If your friend is dying or has a relative who is, and they refer to the death or how difficult treatment/daily life is, don’t brush it off, dismiss it, or say, “Oh, you’re not going to die. You’ll be fine. It will all be okay. Things will work out.” Saying this to someone with stage 4 cancer comes across as dismissive of the seriousness of their diagnosis.
If the listener says, “Oh, that’s depressing, let’s not talk about dying,” it can isolate the person who is ill, making them feel they should not be thinking about what is a very real concern or outcome. As Julie Klam points out in her book Friendkeeping, acknowledging someone’s wishes should be paramount. She tells the story of her mother and her mother’s friend Patty who was dying of cancer. Patty wanted to give Julie’s mom a pendant. Rather than gratefully accepting it, Julie’s mom insisted Patty would wear it again, that she would get better. Instead, she died a few days later. Years later when recounting the story with regret, Julie’s mom said, “She knew she was dying. It probably would’ve been comforting to her for me to acknowledge that… I was just afraid that she had some small glimmer of hope. I just didn’t know.” I would bet that if that same scenario happened again, Julie’s mom would act differently.
Later in the chapter Julie recounts being a friend to someone who had to terminate a pregnancy. She asks Julie a question that continues to haunt me: “Will anything ever be good again?” It echoes in my mind now: Will anything ever be good again? Will anything ever be good again?
The truth of the matter is that for some it will. For some people, it won’t.
Check in with your friend intermittently. Give her reminders that she is not forgotten even if she is not out in public. I love getting cards or texts or emails that tell me what my friends are up to. As I write this my friend Kathleen texted me to say she was eating at one of our favorite places. “I miss your company” she said. How can you not love that?
I love written notes. I save my favorites. When I’m having a bad day there is something about pulling out a card, seeing handwriting, reading a message. It’s just more personal than seeing it on a screen. Of course texts and emails are great for frequent check-ins, but for a special message? Real paper can’t be beat.
Other winners to me are notes that remind me of a funny experience a friend and I had, a favorite memory. Many people know I love my garden and flowers. They will send me a pretty card and tell me what they saw at the farmer’s market or in their own garden or what they’re looking forward to about Spring. Sometimes they will tell me about being on vacation and how they thought of me when they saw the water or the tropical plants and they remembered a trip I’d blogged about.
Some send a favorite poem or story or memory. I like those. I don’t like religious quotations or cards that focus on people praying for me or hoping for a miracle. That assumes I am a religious person (I am not and I don’t believe in miracles). I think cards should focus on the person— the connection to that person, your friendship, not what types of religious comfort or explanation the writer endorses.
One Twitter friend, Neil Shurley, wrote me a song titled “We Love You, Lisa,” and then made a video with people holding up signs that say those same words. I still watch it. I always cry. It’s one of my favorite things anyone has ever done for me. This, from what most people would term a stranger. Another friend, Nichole, took photographs that people sent her, combined them with poems and sayings and turned them into a photo book for me. When I’m down it’s another thing I reach for to feel support.
Does the person who is ill have children? If so, you can do what one room mom did for me this year: For school events Lizzie always asked if I felt well enough to join on any party or field trip. She offered rides to school performances. When I could not attend, she (and other moms) took photos and videos and sent them to me… without being asked. My friend Zerlina put together a playdate calendar and a dozen moms signed up in rotation to have Tristan over three times a week for playdates for the past six months. This was especially helpful. Sometimes I’ve been well enough to say we would host the playdate here. But knowing there was fun built in with his friends was a relief to me.
Finally, I always love my mother’s suggestion for one of the best questions you can ask in any situation whether it be posed to a friend, a spouse, a child, a coworker. When someone comes to you with a complaint, a problem, or a rant asking the simple question, “Do you just want me to listen or do you want my advice?” is a wonderful way to be supportive. Sometimes a friend just needs to cry and vent, no advice wanted. By asking you will show sensitivity to the distinction. This is what I mean by not needing to have had the same experience to be a good friend. Listening matters. It’s free, and all you have to do is offer (and follow through).
And if you have a serious illness how do you respond when someone asks you how you are? If you don’t want to answer in detail, one suggestion is to say, “There are good days and bad days. Today is a … day.” This response is also a good one after the death of a loved one. If you are having a good day it allows you to acknowledge they’re not all like that. If you’re having a bad day it expresses that you know they won’t all be like that, either.
……………………………….
I think we all like to hear that we matter, that we make a difference, that we are loved. In the end, you can never go wrong by telling (or writing) someone what they mean to you, what you like about them, and what you enjoy most about being with them. This is the essence of friendship to me. Some days you need a serious chat. Some days you need a friend to be silly with. Some days you need a friend to go shopping and have a gossip session with and try to put cancer in the back seat for a few hours. There are many ways to be supportive.
My dear friend Cathy texts me every morning to wish me a good day and asks, “How can I help you today?” I most certainly don’t expect that every friend should do this. But boy, it means a lot that she does. I rarely need something these days. But I will someday. And when I do, I know she’ll be there for me.
I have so many people in my world who care. I know how fortunate I am. I hope that some of these suggestions will be helpful and I am sure you will find others as readers comment on the post. You don’t need to have many things to say… a few good options will do.
…………………………………….
I hope you all have a good weekend, we are starting to feel Spring here and boy, does it feel good!
 The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
















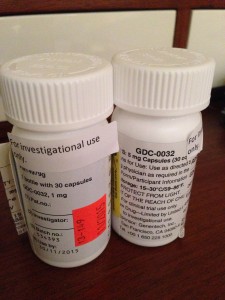



























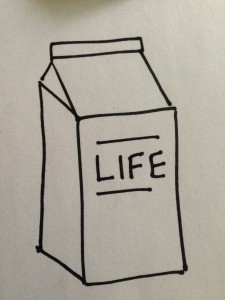



 Link to Twitter
Link to Twitter