December 3rd, 2014 §
 I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week.
I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week.
The first thing I want to comment on is the death of my dear friend Ann Gregory. She died the day before Thanksgiving. Her obituary appears here. Some of you came to know Ann through Twitter or through my stories about her in person or through her comments here on the blog. If you did get to know her and chat with her on Twitter over the past few years, you were lucky.
Ann was the strongest person I know and had numerous diagnoses of cancer throughout her life including leukemia and squamous cell carcinoma. She was quite stoic and, like me, was always okay as long as there was a plan for what to do. We spent hours texting each other (often those hours could be in a single day, depending on which one of us was sick or well that day or what phase of treatment we were in), always supported each other, and she was always a valuable source of information for me. I have missed her so much in the week since she has died. We did not want to leave each other. Four days before she died she texted me to say her goodbye. I will never delete those text messages and I am so sad that I have to do all that I have to do without her. My heartfelt condolences go out to all of her family, especially her husband, Chris, and her legions of friends. Her blog appears here. I just can’t do her life and personality justice here right now, but there is a gaping hole in my life now, and Ann is the precise shape of that hole.
…………………………………………………..
 Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.
Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.
Even though the fitting and simulation take a while, each radiation session itself is quite short. After confirming the patient’s identity with name, birthdate, and a photo, you lay down on the table, they hand you a foam ring to hold on to across your chest so your arms are relaxed and easy to keep still, and a foam wedge is placed under your knees. Then the aforementioned mask is placed on and with some tugging and effort, attached firmly to the table you’re on. The photo gives an idea of what it’s like.
The technicians leave the room and the linear accelerator moves into place. The beam goes on and I can see even through my eyelids a very bright light with a bluish cast. It is only on for less than a minute and then it moves and does the same thing to the other side of my head. They say there is no smell to radiation but I always smell something. I have read that others do, too. I can’t describe exactly what the smell is. I’m working on figuring it out. I’m usually focusing on relaxing and not getting claustrophobic so I haven’t solved the mystery yet. It doesn’t quite smell like burning hair but maybe that is part of it. After the actual beams are done then the techs scurry back in right away and release the mask from its mooring. That’s it.
As I said in my last post, side effects don’t usually start for brain radiation until closer to the end of the 10 session series. So, next week I will see more of the fatigue and the start of hair loss. Memory loss takes a bit longer to occur. There are many things that might happen including headaches and nausea and confusion and blurry vision but those are not as common. I did not have any neurological symptoms before starting radiation so that is a good thing. I have some nausea and loss of appetite but that is primarily due to the liver situation. An inflamed liver causes pain, nausea, and so on.
I did my liver simulation for radiation yesterday. This is actually more complicated for the radiation oncologist to map out than the brain because part of my liver already received radiation when I had the radiation to my spine in January. For this reason, she needs to make sure it doesn’t get any additional radiation this time. None of the 13 or so tattoos (permanent ink dots placed by a needle under the skin to mark where the alignment should be for the laser beams for radiation) that I had from the spine and pelvic radiation in January were in the correct spots for the liver so I got about 6 more of those. The radiation oncologist will focus on the right lobe of the liver, but even that is tricky with the kidney and bowel in range.
They will work to map it this week and I will start liver radiation next Monday. That means this week (12/1-5) will be brain only, then one week (12/8-12) of both brain and liver, then one week (12/15-19) of liver only. Then I will wait a few days and begin chemotherapy again. These are hard days ahead. Side effects will be kicking in right as I go back to chemo. Christmas week will be the peak for all of this to hit the fan.
I’m continuing to get IV fluids 2-3 times a week and am also getting magnesium infusions because the most recent chemo continues to cause my magnesium level to stay far too low. Even though I am not getting chemo right now (in this case, chemo and radiation can’t be given together even though with some cancers they are) I am still having lingering effects from the last round of Cisplatin. The magnesium infusions add about 8 hours a week to time I need to be at MSK (Memorial Sloan-Kettering).
There really isn’t time to do anything else besides be there and rest at home. I’ll be there every weekday for the next few weeks. I’m managing okay and know it’s going to get far worse before it (hopefully) gets better.
I think this should give everyone a pretty good timeline of what I’ll be doing in the next few weeks so that if I can’t update much, you’ll still know. I know people have questions and I will do my best to answer them, it might just take me longer than usual.
Thanks for all of the support, as always.
November 5th, 2014 §
 A quick update.
A quick update.
I received my fourth round of Navelbine yesterday and I’m feeling incredibly rotten today. We’ve now confirmed that this drug is not working (at least as a single agent), so I probably will not have to put up with it much longer.
Yesterday I learned my liver tumors are too big to do the ablation procedure we had hoped (please see update on 11/7 for some corrections to this paragraph). Instead, later today I will be evaluated for a more complicated procedure called Yttrium 90 radioembolization. I will learn more about it today but the general idea is that a catheter is snaked up through the groin to one of the two blood supplies to the liver. While the liver usually gets 75% of its blood from the portal vein, when there are tumors present they often get almost all of their blood from the hepatic artery. The interventional radiologists insert radioactive beads of glass or plastic into that artery so when the tumor gets its blood supply, that supply is radiated and hopefully shrinks the tumor locally, without disruption of healthy cells in the rest of the body. Only one tumor can be treated at a time. It is not a cure, it is just palliative for these metastatic tumors to try to stabilize them or reduce them. I will also need to be off chemo for a week on either side of the procedure.
I also need to be seen tomorrow by the cardiology team at Sloan-Kettering for another opinion on my pericardial fluid situation now that I am having some symptoms and have had more imaging done. They will decide if we need surgical procedure to drain the fluid and biopsy it. It is probably malignant but we can’t be sure. If they don’t feel we need to do any intervention right now, we will watch and wait.
So, we have some big decisions to make including what chemo to go to next. I won’t go into those options here now. First I need to deal with these more pressing issues of the liver and the heart. I had hoped to be able to rest and get through these difficult post-chemo days at home but the appointments mean pushing myself beyond what I really think I’m able to do sometimes. But I have to get answers and be able to get scheduled for what I need when I am hopefully feeling a bit better next week.
Once we have some decisions made about it all I will report back. Things just don’t seem to go the easy or simple route and I’m getting used to that. For now I am going to try to conserve energy and stay pretty quiet. Thanks to you all for your continued support.
November 2nd, 2014 §
 Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Monday I saw my cardiologist to try to get some information about some symptoms I’d been having. My echo (and later in the week, the CT scan) showed there is some excess fluid around my heart. For now it is not causing any effect on heart function but we can’t rule out that it is a problem. I’ll have to repeat tests in a few weeks to try to see if it grows in volume (this would indicate a more sinister issue, and we would need to rule out a malignancy). For now, though, that goes on the back burner.
Tuesday I had bloodwork and IV fluids. The bloodwork is still a bit unclear about if the current chemo (Navelbine) is working. The rise in tumor markers is slowing but we need some definitive results this week, I think, to feel confident in interpreting them. The bloodwork also revealed I was anemic again, so on Thursday I went to New York City and got a transfusion of two units of blood.
On Friday I had a CT scan to compare to my last scan and help us make decisions about treatment. The CT showed both some good news and some concerns. While the lymph nodes and malignant tissue in my chest have resolved (chemotherapy in the last six months has worked and reduced those areas), my liver unfortunately shows two tumors.
The best thing at this time would be to biopsy portions of them (to gather tissue for future testing; my cancer has rarely been in areas that we can actually get samples, so this presents a rare chance to grab some) and also do ablation on them. Ablation is a localized procedure that when successful, destroys tumors of a particular size with very few side effects.
So, a lot is up in the air at the moment.
Because it is only Monday morning I don’t know what this week will bring in regards to chemo. We also don’t yet know if the interventional radiologists will decide that I am a good candidate for the ablation. For now, I wait.
Palbociclib, a drug I received through the expanded access (formerly “compassionate use”) program from Pfizer should arrive this week. That process took approximately 9 weeks and usually takes longer than that. I am fortunate my oncologist kept the process moving in such a timely manner (all applications and documents for such use must be done by the physician, not the patient).
I’m not feeling that well and have been primarily staying home for the last month. Now that I think about it, though, I’ve been basically staying home for the last ten months. Many days my half hour in the morning driving the older two kids to school is my only outing of the day. But I am patient.
At this point the options are still very reasonable and typical for this stage of the disease. I’m waiting for the next treatment proposal and then onward we go.
September 26th, 2014 §
 I have become an expert in uncertainty.
I have become an expert in uncertainty.
I don’t know how I will feel from one day to the next. I don’t know if the chemotherapy that worked a few weeks ago will still work today. I don’t know how my body will tolerate what I’m doing. I don’t know how long this all will last.
I was supposed to get chemo a few days ago (Tuesday) as usual. However, when I arrived and had my bloodwork done I found out that the higher dose of Carboplatin the week before had really continued to hit my body hard. My platelets were too low to safely receive chemo. This means I had very little clotting ability. The Gemzar I was due to get that day hits platelets hard so it presented an even more dangerous situation. My hemoglobin was on its way down, too. I was told I couldn’t get chemo as planned.
Instead, during what turned out to be a 13 hour medical day, I received two bags of platelets by transfusion and one unit of packed red cells. I had never received platelets before. I had no idea what they looked like… they look like pale orange juice (shown at left).

This is a great opportunity to share a link to Sloan-Kettering’s online information about blood and platelet donation and eligibility criteria. I do not need designated donations at this time but I do rely on donor blood and platelets so if you are eligible please donate when you can! It’s a great way to help those with cancer for free.
Today (Friday) I was finally able to get chemo. We will see how I tolerate this dose but the plan now is that rather than receiving my next Carbo/Gem in 14 days, I will get it in 11 days to get back on schedule. This means I will have to do a few daily Neupogen shots next week to boost my white count.
There will be another book auction this year with proceeds going to my fund for metastatic breast cancer research. Authors you know and will recognize are donating signed copies in many genres. I will be sharing links here and on my blog Facebook page if you want to window shop or place a bid. That will be in October. Thanks to Erika Robuck again for arranging this; I know it’s a lot of work.
Wishing you all a good weekend, we expect a last burst of summer here in Connecticut.
September 8th, 2014 §
 I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
First let me report the good things. I have had some great days after my transfusion last week for severe anemia (expected often now after this much chemo).
On Friday night I drove Colin in heavy traffic to his first travel baseball game (took two hours). Then I sat watching warmup and the game which was another 3.5 hours. Then an hour home. I am detailing that time to brag. Look what I did with my son.
It wasn’t physically easy for me. But it was joyous. We got so punchy in the traffic jam that we were waving our hands in the air “seat dancing” to the music. We nicknamed a car “Duck Dynasty” that was broken down by the side of the road and then got lost at the venue and ended up 4-wheeling over gravel hills. We had a blast. Here is my precious middle child when we arrived at the field. The team won which was exciting. It was his first game on a full-sized field and also under the lights. I also got to take him  to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
The medical update since the last post is that in short, there isn’t a good clinical trial that I qualify for/am willing to enroll in right now. The chemo regimen that I am on makes me ineligible for some because it affects my blood counts so severely each time now (quite a catch-22, I would need to go off chemo to even have a chance at being considered). One trial I can’t be considered for because there isn’t enough tissue left from a previous biopsy to use it for required testing. Because my cancer is primarily in bones or other places inaccessible by surgery, this is not an easy problem to fix.
Now I’m going to get a bit technical. I’m hoping to explain a bit about how the different clinical trial types work since many people don’t know these distinctions. Consider this your breast cancer education for the week! Yeah, you know I’m not a doctor so I’m explaining this to the best of my ability. Ask a doctor for more info, especially one who works in clinical trials to be sure the trials you or a loved one might be considering work the same way.
Here we go:
One type of Phase I clinical trial (which I would qualify for) is risky enough that this option isn’t reasonable to me right now. Let me clearly state that they may become very reasonable options at some point soon and I totally understand why other people choose to do them! These particular phase 1 trials I’m opting out of for the time being are the kind that are testing safety of a medication previously untested in humans. That is, they don’t yet even have a dose that they know is safe. They are called “dose escalation Phase I trials” which means they start with a low dose they think is safe and gradually increase the dose until the side effects become too bad and the test subjects can’t continue and they stop participating. They do these on a small number of people.
This process establishes the maximum tolerable dose and the company hopes to then proceed to a Phase II trial. That Phase II trial tests if that established maximum tolerable dose even does anything measurable (Phase II trials test for efficacy: is this drug keeping the cancer stable or even causing it to shrink?).
To complete the clinical trial trio, a Phase III trial tests the “current standard of care” plus the trial drug against the current standard of care alone. That is, does adding this drug to a treatment that is a normal one for this cancer improve outcomes above and beyond just giving the treatment the patient would normally get (are results better? The same? Worse?). For ethical reasons there are no placebos used alone instead of treatment in Phase III trials in metastatic breast cancer. They would be used only to combine with the standard of care treatment. No patient goes untreated. All get the usual treatment as the guarantee.
This process means that during the Phase I dose escalation trial I first mentioned 1) you don’t know if the trial drug is safe, 2) you don’t know if that dose is too low for some or all of that time to even be doing anything, even if it is eventually going to be efficacious, and/or 3) if it even works at any dose (without making things worse). This means continuing with your cancer potentially untreated for months, an often dangerous proposition in metastatic cancer.
I don’t want to go into more details of those trials but I do think it’s important for me to continue to explain the way that some clinical trials work with metastatic breast cancer.
As I think I mentioned in my last post, the likely immediate plan was to increase the dose of one or both of my current chemo drugs. Because I opted not to pursue enrolling in a clinical trial I will remain on IV chemo. If I had chosen the trial I would need an additional two weeks without any chemotherapy to complete the mandatory washout period where I do not use any medications to treat the cancer because their presence in my body could affect the trial drug results or side effects.
I am going in for an increased dose of Carboplatin and steady dose of Gemzar on Tuesday. I did have one increase already in the Spring on my Gemzar dose. We will see what kind of response we can get from this Carboplatin increase, if any. It will hopefully buy us some time until some other trials open up and/or we can consider if we can do a biopsy once we see a current CT scan.
A few readers were concerned that I was relying too heavily on tumor markers in my decision-making. In short, I’m not. I am well aware (as I’ve said in almost every post except last time) that markers, particularly CA 15-3, are not reliable for many people. This is why this test is not used as a screening test for people to find out if they have breast cancer. If it were valid they would use it instead of or in conjunction with routine mammograms.
I know many doctors don’t use blood tests for markers at all and for some types of breast cancer they are totally worthless. Trust me, oncologists at Sloan-Kettering are well aware of all of this information as am I. The most important piece of information is a history of them in me and how they correlate with scans and my disease progression. I am one of the people for whom they are tightly and reliably correlated with my disease. We have had seven years of studying them in my particular case and two years with close monitoring during metastatic disease. So while I definitely appreciate the concern, you can rest assured that we make decisions with all of this in mind. It was my error in not putting that usual caveat in that last post.
So… for now the plan is: higher dose of one of two chemo agents on Tuesday. Test markers to see what they’ve done in last few weeks.
In case you are curious, going for chemo doesn’t just mean getting two drugs. The infusions I will get on Tuesday are numerous. I will get the following 8 infusions in this order: Decadron (helps with nausea and mainly to help prevent an anaphylactic reaction to Carboplatin because I’ve had more than 6 infusions), Pepcid (helps with anaphylaxis prevention and also bonus heartburn help), Benadryl (helps prevent anaphylaxis), Carboplatin (chemo agent #1), 1 liter fluids (helps prevent dehydration and bonus helps to keep kidneys functioning well to avoid high creatinine levels that can be dangerous), Aloxi (anti-nausea, blocks signals from stomach), Gemcitabine (chemo agent #2), Emend (blocks nausea and vomiting signals from the brain).
Away I go… thanks for the support. These days of uncertainty are difficult for me. I like a plan.We have a short term one and I am, as always, moving forward. As I wrote in a prior post and re-read tonight:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
February 23rd, 2014 §
 Sunday morning.
Sunday morning.
A different kind of strength: shave the few soft but strong hairs that are finally ready.
Now gone to the floor.
No tears.
Necessity.
……….
You’ll be seeing more posts here in the near future about some of my feelings over the last two months. I’m starting to feel more like myself. The vertigo is lessening with the decrease I’ve been able to make in the pain medication, as we’d hoped. I’ve reduced the pain meds by 20% and the hope is that as the radiation effects start to kick in I will be able to decrease more. It’s been five weeks now since I finished radiation. I needed these Fentanyl patches desperately while the tumors were out of control. I could not have done it any other way. But certainly we all want me only using the amount I need to control my current level of pain.
I will be going back to meet again with my palliative care doctors this week to reassess my pain meds and talk about the plan for the next few weeks. I was thrilled to see that my last post about the importance of early palliative care and its definition (not end-of-life pain management… but instead total patient care pain management) was so well-received by patients and doctors alike. I encourage both sides to really form a team and focus on all side effects that patients are having with all kinds of treatment.
Patients function better not only emotionally but also physically in that they will heal better if their bodies are not weakened by pain. It takes trial and error to find the right drugs and the right amounts. It takes patience. Most palliative care doctors are experts in patience, I have fortunately found. I know that is not always the case and I always receive emails and comments from people who have had distressing experiences with their care. I am so sorry for that. I am hoping by relaying my own experiences, readers who have not yet found help with pain will have strength to ask again or pursue help if they’ve been unable to.
I’ve started my second month of chemotherapy (Taxol). I do three weekly treatments in a row and then have one week off each month. I had my first infusion of my second month on Thursday. I haven’t had any additional reactions to the chemo so I’ve been able to have the sessions done rather quickly (30 minutes for the 3 pre-medications and then 60 minutes for the actual Taxol). Sometimes I go alone and sometimes I have a friend join me. I am developing a routine and it has worked well so far.
 We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
For today I’m sporting a head scarf and getting used to seeing a new reflection looking back at me in the mirror.
………
Make the most of this day. Whatever that means to you, whatever you can do. No matter how small it seems to you. Don’t waste it.
January 10th, 2014 §
 The car has always been a place of refuge for me.
The car has always been a place of refuge for me.
The shower, too.
Water to rejuvenate
Clearing away the old,
Ready for a new day ahead.
The moment of awakening is significant.
I have learned quickly what the next few hours will be.
I try to give a nurse a complete report but I encounter one problem immediately.
I really cannot type accurately.
My body shakes, my hips cry out in bony futile gasps. I gather up my pump cords, release myself from the wall’s grip.
I walk, counter-clockwise around the nurse’s station with a vengeance, trying to push the pain and discomfort away.
……………………………………..
I am Angry at this morning and that which has me here.
The tears arrive.
The radiation pain seems to be on the way in.
How long with it last? Does that mean it’s working? I and everyone else ask.
“I don’t know” is the way to do it. I say it aloud to the dark, embarrassed after the first word that I realize I am alone in the room.
I hear my voice, speaking to someone not present.
I can’t help but cry as I push the pole.
The movement makes it better. It reminds me of being carefree on a summer day, wind in my hair from the sunroof, feeling the sun on my face.
I think of my friends readying their homes for the day before work and school.
I can feel the radiation, where it burns, or at least the spots where tumors are trying to escape their home,
where they try to find new lands to conquer in a cat and mouse inside my body.
It doesn’t matter what stinking metaphor you use for it; in this case, all roads lead to Hell.
I contemplate eyeliner while the nurse stands, patiently waiting to see how I’ve done overnight.
…. But there is no one there.
I focus very hard on the tasks at hand: morning medicine most especially.
I start to tell my nurse that I weighed myself already today. Or yesterday. Or two days ago. But I can’t remember now. And so I remain mum.
In each moment my mind leaves. I don’t know where it goes. But in those gaps which feel like seconds, minutes have gone by.
The tea is divine, hot silky relief from the cold my body cannot push out.
I realize whatever it is I thought I could accomplish at the keyboard won’t happen once again.
I can’t concentrate. I find gibberish on the page. It takes hours to do a few moment’s work.
Extra time lost.
Time lost.
My precious time.
I stay committed to sitting up, bedside, fighting the urge to recline.
I listen to music trying to keep myself alert.
I think about my children, wondering what each is doing…
I realize today I am too foggy from medication.
I won’t be able to do much for a while. I am too busy talking to people that are not there.
I will rest, let the pain calm, let my head settle.
December 18th, 2013 §
 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
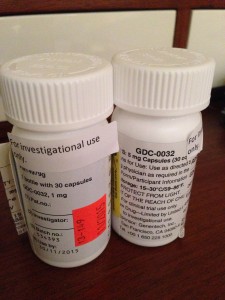
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.
October 18th, 2013 §
 I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I had CT scans of my chest, abdomen, and pelvis. I also had a bone scan of my body. I had bloodwork and an EKG and a urine test. These are all tests that need to be done before I can start the clinical trial and will be used as my baselines. Monitoring will happen at frequent points throughout my treatment. Bone scans and CT scans will be done every 8 weeks for the first 6 months and every 3 months thereafter for as long as I am on the protocol. I’ll write more about the trial and the drugs (fulvestrant and GDC-0032) when I get underway on the 28th. I had a lot of trouble with with the blood portion as I only have my right hand and forearm for blood. It took six needles in that area (which included two blown veins) to get all of the radioactive tracers in and blood out. I will be discussing the option of putting in a port at my next appointment.
So the short story is that results were not as I’d have hoped. I wanted it to be clear that the cancer was still confined to my bones and lymph nodes, even if it were in more bony locations. This, however, is not what it seems to be.
First I need to explain about the tests. I’m going to briefly try to explain why it’s a bit of apples and oranges to compare my test from August with my tests last week and why all of it is a bit jumbled. In August I had a PET scan. In oversimplified terms this test picks up on high activity metabolic areas. So, cancerous tumors (and also some false positive areas on occasion) “light up” because they have a high number of rapidly dividing cells. It measures activity. CT tests, on the other hand, are static. They are like x-rays. They just take a picture without regard to whether the nodule/lump/tumor etc. is malignant. It shows there is something there but can’t necessarily tell you what it is in terms of metastatic breast cancer. CTs are very precise visually. PETs are not necessarily so. CTs in my case can’t tell us for sure if a spot is malignant.
I now have a small spot showing up on my liver that wasn’t visible on the PET in August. So is it a new metastasis? Or is it a benign spot that just didn’t show up on the PET because it’s not cancer? Who knows. We will have to wait and see if it changes when we do the next scans 8 weeks after the trial start (10 weeks from now). There are also nodules in my lungs and pleura. These are potentially (likely) malignant but the ones in my lungs have not changed size in 8 weeks.
I think that’s as much detail as I need to go into. The worst spots in my bones are my T12 vertebrae and my first rib/clavicle area. There are many spots but those are the ones that cause the most pain.
Unfortunately and most significantly at the moment, the scans also showed that the small pleural effusion (fluid in the lining around the lungs) has grown.
So we have many question marks with a few new areas of concern. For now we watch and wait. The pleural effusion will need to be drained if it grows or continues to cause breathing problems. For now any physical exertion gives me trouble. I need rest throughout the day but am trying to conserve energy for activities with the kids.
None of this news changes anything about my planned start of the clinical trial. Whatever these spots are and wherever the metastases are, the drugs I will start in ten days have the best chance to keep the spots stable and eventually perhaps shrink them. Reports from the phase 1 trial participants showed that often there was a stability period of about 8 weeks before some achieved some tumor shrinkage. I have ten more days to go chemo-free before I begin. I am counting the days. That start day is the most important day I have. A few of us in the trial are starting on that day so hopefully I will get to meet some of the other participants. There are 60 nationally in this phase 2 trial, approximately ten people will be at my location. There is relief in knowing there is no placebo in this trial. I may not respond but it won’t be because I received a placebo.
I wish I had better news about the scans but I also am resigned. This is what this disease does. I must do the best I can given my daily symptoms. There are questions marks and only time will give us answers. I try to have as much normalcy as I can, which often just feels like sleepwalking through the days and a bit of play-acting. But it’s important.
I keep coming back to a few lines I wrote recently:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
I can’t do anything more to change what’s happening inside. I have a plan and I just need the days to go by to get started. My quality of life is suffering at the moment but I hope that this will change. It is a rollercoaster, one I have been strapped inside unwillingly. Some days are good, some days are not. These happen to be some of the icky ones, but as always, I press onward.
Every morning I say to myself:
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be tough to do. Persevere.
September 30th, 2013 §
 Here we are again. A crossroads.
Here we are again. A crossroads.
The third of many we will have.
I’ll give a bit of a recap. I know it gets quite technical but documenting the details is important for those who also have metastatic breast cancer.
It’s almost one year to the day that I was diagnosed with metastatic breast cancer in my bones and lymph nodes. I started on the cytotoxic daily drug Xeloda first (in addition to monthly infusions of Zometa) which gave me six months of success, shrinking the amount of cancer evident on PET scans.
In April 2013 when my tumor markers started rising I started on the hormonal combo of Aromasin and Afinitor (and also switched from Zometa to Xgeva because of difficult side effects I was having). I started on a 5 mg/day dose of Afinitor with a 25 mg dose of the Aromasin. I gradually increased the Afinitor dose to 7.5 mg/day, and then when my markers began to rise again a few weeks ago, I started on 10 mg a day.
It has now been five months on this combo (in all of its different dose strengths) and my markers are rising. This chemo is no longer working. So, it’s time to decide what to do next.
Regular readers will know that this is typical of metastatic breast cancer: some therapies may not work at all while some will work for a while. Ultimately, though, the cancer becomes resistant to each of these treatments and will progress. Sometimes you get a great response and can reduce the amount of cancer that is present. Oftentimes you settle for the success of “stability” where the cancer isn’t reduced, but it also isn’t growing. It’s often referred to as hanging out with “Stable Mable.” This is still a good response in most people’s books.
Especially when your cancer is still confined to your bones and lymph nodes, stability has the added feature of being life-saving: as long as the cancer is in those places it cannot kill you. Only once it metastasizes to organs can breast cancer kill.
So… now it’s time to decide what to try next (this part gets technical). Right now it’s looking like I’m headed to a clinical trial of a drug that has shown promise in breaking the resistance of hormone sensitive breast cancers especially in people like me whose cancer displays a Pi3k mutation (40% of people with ER+ breast cancer have one of these mutations). This experimental drug would be in combination with a drug commonly used for my kind of cancer (Faslodex). I’ve enrolled with the clinical trial team. This is a Phase II trial so I would be guaranteed to get the experimental drug.
What does this mean? In simple English, it means I’m trying a new drug that’s designed to break the resistance of this particular kind of cancer to treatment. It seems to be especially effective for those with the type of cancer mutation that I have (Pi3k-alpha). If this drug makes the cancer susceptible to therapy, then the other drug I’m taking can do its work. This class of drugs is at the forefront of where cancer research trials are right now.
I’ve been pre-screeened and have a few more hurdles to clear: scans, bloodwork, and a three week “washout” period where I must be chemo-free to allow any residual effects of my current treatment to clear. Am I nervous about a period with no safety net? Yes, a bit. But I also am curious how my body will react to having current chemo clear my system. I’ve had a lot of trouble with things like high blood pressure, high cholesterol, rapid heart rate, shortness of breath, and headaches in the past few months. I’m interested to see how many of these will improve.
The new drugs will have their own series of side effects, some of them might be similar and a few may be different and more serious. So this three week period sits okay with me because if my current treatment isn’t doing anything anymore, it’s of no use anyway.
There will be so much to share about being involved in a clinical trial. And I will share that with you, should I make it through the final screening process. I am learning so much as I go and I think there is a real chance here to inform others about the experience. Trials are as varied as can be. Each has criteria that must be met. Sometimes you end up on the good side of these and sometimes you don’t.
My oncologist looked at a host of trials before we chose this one. I was ineligible for many of them because of the drugs I have already tried, my particular features of my cancer, what cities the trials were offered in, when they were enrolling patients, etc. Some were not attractive to me because of the phase of trial that it was (I’ll explain in a separate post the differences between Phase 1, 2 and 3 trials). I am glad to be in a trial where a drug has already passed initial safety standards and will also be given to every patient in the group (there are no placebos in this phase of trial).
It’s important to note that a clinical trial should not necessarily be viewed as a “Hail Mary” meaning it’s the last remaining hope. In reality, my sense is that this is very rarely the case, at least with Phase 2 or 3 trials. They can only establish true efficacy in people who are still at certain phases of the disease process and haven’t had too many chemotherapy agents already.
To me the key was to find a trial that had a good scientific basis for success, was currently enrolling patients and was within commuting distance. In addition, I think it’s best if the standard of care drug is one you would already be considering using at this point in your treatment. There is a database at www.clinicaltrials.gov where you can search for trials.
I have reserved my spot in this trial. If I meet the testing criteria I will be one of 60 patients nationwide on this particular protocol, about 10 at my particular location. I view it as an opportunity. It is well-suited for my cancer at this time in treatment. It’s using the newest thinking in targeted therapy based on genomic analysis.
It’s scary, yes. But if it doesn’t work I still have standby treatments to go to (and other trials by that time that I hopefully would be eligible for). I know there is no cure. But maybe this one will give me a chunk of time.
I won’t go into details here but I know people will ask what’s involved. The treatments will be injections (Faslodex is two big intramuscular injections in the butt every month after doses every 2 weeks the first month) combined with daily oral capsule (the experimental drug). I will also continue to get an Xgeva injection in the arm each month. There will be a strict schedule of fasting bloodwork in NYC every two weeks and scans every 8 weeks to monitor the cancer’s growth. I’ll have to keep a medication diary. I’ll let you know how everything else works once I am underway. It’s a lot of work, especially in the first two months including all of the meetings and tests just to get started.
There are so many questions I know people will have. If you post your questions in the comments I will do my best to answer them in future posts if I can. You may post them anonymously if you like. For now I’m not going to state the name of the drug (actually just a string of letters and numbers) until I’m actually enrolled.
It was quite devastating to get the news that the current chemo isn’t working anymore. It always feels like the rug being pulled out from under me. I always cry. I always feel like I’m falling.
But plans are my safety net. Options are my lifejackets.
I leap from treatment to treatment on my tippy toes, knowing if I place too much weight I will sink.
This is the dance I do now. Forever.
September 13th, 2013 §
 It’s always right when they pull the bar down over my head and jam it into my lap on the rollercoaster that I silently start screaming, “Wait! I changed my mind! Let me off!”
It’s always right when they pull the bar down over my head and jam it into my lap on the rollercoaster that I silently start screaming, “Wait! I changed my mind! Let me off!”
By then, however, it’s too late.
With a jerk the car moves forward, its underbelly grabbing the hooks to lift it skyward.
By the time we are moving, climbing, the car is making a clicking sound and I am sure this was a mistake. I wedge my knees against the back of the seat in front of me to minimize my movement.
I steel myself, knowing the drop will come whether I like it or not.
And then there is that moment, that nauseating violent moment before the floating…
For a brief portion of a second I’m airborne, held in by that suffocating bar. Down we go and I slam back into the seat. I tell myself it will be over soon. I just need to ride it out. It will end.
These days I’m on a roller coaster ride that doesn’t end — well, not anywhere good, anyway.
When we last met here for an update, I said the increased dose of chemo had shown a response. That response is proving to be short-lived. Yesterday my tumor markers were up again, back in the range where we need to discuss changing chemo again. It’s been about four and a half months on this chemo combination of Aromasin and Afinitor (I continue with monthly Xgeva injections).
This is the cycle of metastatic breast cancer: chemos inevitably fail. The cancer becomes resistant, mutates, signals a new pathway to drive its survival. We have no way to know how long each will last. When you read studies and “success” is deemed an extra two months of progression-free survival you know you’re dealing with heavy realities.
The immediate plan is to increase the Afinitor one more time, to the maximum. I’m told no one tolerates this dose regimen for long because of the side effects. But I’m almost at that dose now anyway, so let’s give that a go. Even if I can get a response for one month, that will allow me time to figure out what will come next. The two options are to continue with a targeted, anti-hormonal therapy of some kind or begin IV chemo after having a port put in. There are pros and cons to each, I won’t go into them here. Once I’ve made a choice I’ll fully explain it, of course.
And so, for now, I increase the dose. I wait. I retest again one week from now, and two. By then we’ll have a plan, and likely be moving on. Another tally mark of treatments tried to buy me time.
It’s too soon:
I fear the safety bar is not locked.
I fear that each time I reach the top of the hill again I’ll be ejected from the ride, skyward, only to plummet to the ground.
……….
Two housekeeping notes:
1. If you only want to read updates on my chemo status and current health, I make it easy for you by titling these posts “Update” + the date as the title.
2. I’m pleased to report that this website is now optimized for mobile device reading. If you read the posts on your smartphone or tablet you will note that you no longer have to scroll left and right to read; the posts are nicely contained in columns. There is a menu at the top to navigate the site and a clean layout. To comment on posts on your device, look at the end of each post for the “replies” link to click. This should make it easier for those of you on the go to leave a comment.
August 29th, 2013 §
 Remember me pretty,
Remember me pretty,
Remember me whole.
Remember me the way I am today
While friends still honestly say, “You’d never know.”
Let me tell you:
It’s not what it looks like,
It’s not what it seems.
Those times are long over,
Now I am on my own.
The beggars have all ridden.
My wishes: horses gone.
I float above it all,
Watching as I do.
Surrounded by people,
Feeling so alone.
Head down,
At the stoplight tears come,
A young man pulls up next to me
Glances once… twice…
With an engine rev, he’s gone.
I hide it pretty well, you see.
They say, “You look so good,”
“You are so strong,”
But in the space that’s in between
I fall apart
I kick and scream
I claw and grab on for dear life.
Because really,
Truly,
What is happening here:
Choice is gone,
Chance is Queen,
Luck will run right out.
Everyone placed their bets?
Let’s see how far we can go.
August 24th, 2013 §
I had my PET scan on Thursday morning and received the results yesterday. I suppose the best way to simply summarize it is that it’s a mixed bag.
There is mild progression from my scan in April. This means there are more sites of cancer in my bones that are large enough to be detected on these scans (“hot spots”). One hip, one side of my pelvis, one thigh, more tissue and some nodes in my upper chest are all newly affected. Many ribs and one vertebrae continue to be pretty plagued as well but were already lighting up on previous scans.
That said, it is good news that the metastases are still confined to my bones and nodes (honestly, I can’t believe the things I call “good news” these days!). There is no evidence on the scan that it has spread yet to my liver or lungs.
So the scan is overall worse than April but still better than October in that the spots are in the marrow and not eroding bone itself (the fracture I had in my collarbone has healed and the cancer diminished there). This is good and also has the benefit of keeping me mostly pain-free. My chemo causes muscle inflammation which hurts but it’s surely preferable to bone pain. Most other side effects have been the same as before.
So here is where it gets tricky. And if you haven’t figured it out by now, this whole business is quite complicated and full of guesswork. My tumor markers had been rising and it looked like we would need to move to a different chemo. At that point (about a month ago), we decided to increase my chemo dose and see if we could get a response. After two weeks my markers dropped. That was right before the scan.
So, one takeaway is that we are learning that my bloodwork is quite accurately reflecting the cancer’s response to chemo. This is not the case for everyone.
So the million dollar question is: is the scan reflecting the peak progression this time and now that I am on a higher dose of chemo if I continue to have lower markers will we see the scan reflect this in another few months? That is, is the scan showing the worst it got and now with the recent increase in chemo it is actually on a downward trend? That’s the hope: continue to see response. Only time will tell where on that dynamic process this static measure is.
This information puts me in limbo yet again. But that’s really what this world of metastatic breast cancer is. And you know, I would rather have limbo than definite bad news (again, I chuckle at the straws I grasp at here…).
I won’t go into details because this post is growing long, but I did meet this week to discuss possibly enrolling in a clinical trial at Sloan Kettering. This would be a phase 1 trial and would be a strict chemo protocol. I will do a separate post about trials in the future because I think there is a lot to learn about them and also a lot of misinformation about their use with this disease. Bottom line on this particular trial: it wasn’t one I would definitely jump to enroll in. Some additional time to explore it and other options some more would be nice. So “limboland” helps with that, too.
For the next few days (and likely the next few weeks) I will continue taking the higher dose of chemo daily, monitoring the bloodwork every two weeks. I’m having shortness of breath for the first time this week and that is quite unpleasant. It is a side effect of the chemo.
The results are not what I hoped for. But onward I go.
I deal with what is, I adjust to new information as quickly as I can and forge ahead into the unknown.
I thank you for your care and concern this week. As always, it takes some time for me to gather, interpret, and process the information before coherently getting it out to you all.
August 20th, 2013 §
This is the last week of summer before school begins.
 This summer was a big one for us. Youngest Tristan went off to sleepaway camp for one week and loved it so much that in the end, he stayed for a month. Paige and Colin returned to camp as seasoned veterans and had a wonderful time in their home away from home. All learned new skills and made new friends. Paige and Colin’s constant banter of camp stories at the dinner table are now supplemented by Tristan’s own stories.
This summer was a big one for us. Youngest Tristan went off to sleepaway camp for one week and loved it so much that in the end, he stayed for a month. Paige and Colin returned to camp as seasoned veterans and had a wonderful time in their home away from home. All learned new skills and made new friends. Paige and Colin’s constant banter of camp stories at the dinner table are now supplemented by Tristan’s own stories.
I’m so pleased they could be in a place where they could just be kids, not worried about me, free to be carefree and happy. It is my gift to let them go, to not keep them here for my own needs. While I want to spend as much time with them as I can, I know that this is what they all needed to do this year.
 I sit back and smile now, loving that they all have a common reference point of their weeks at camp. Despite the eight year age gap they all find laughs and joy in their summer adventures. They look older to me, of course. And while others are sad about the passage of time and their children growing older and being independent, I say again that I cheer it.
I sit back and smile now, loving that they all have a common reference point of their weeks at camp. Despite the eight year age gap they all find laughs and joy in their summer adventures. They look older to me, of course. And while others are sad about the passage of time and their children growing older and being independent, I say again that I cheer it.
You see, my job now is to prepare them for life without me. My goal is to show them how to accept the help of others but not be reliant on it. I choose to show them every day that there is determination and nobility in facing what life throws you. You may not be able to change the final outcome, but you can change what you do to be ready for it. The strongest way of teaching this right now is by living my life deliberately, making choices and showing them the best I can be. This doesn’t mean denial. Nor does it mean I don’t lose my temper or raise my voice or fall apart sometimes. To be emotionally numb or invariable in my response to what is happening is not healthy. I try to show them that expressing what they feel is a better option. Emotions of anger and sadness and grief and fear are fine to have. It’s beneficial to talk about them, but dwelling on them won’t make things better. Acknowledging their reality, their truth, their basis is what’s needed.
As I always say when I get bad medical test results: a short pity party is good. Then you have to pick yourself up and move on.
 It has been almost eleven months since my diagnosis of stage IV breast cancer, and there isn’t a day that goes by that is free from concern. I notice myself being more and more affected by the daily chemotherapy, feeling more fragile, more vulnerable. I have already had one bad respiratory illness this summer, and I worry about the school year and all of the potential colds and infections that will be transmitted. I don’t want to think about the ways cancer affects my daily life, but I must. The decisions I make about activities, treatments, and chemo all directly affect my life… both in length and quality.
It has been almost eleven months since my diagnosis of stage IV breast cancer, and there isn’t a day that goes by that is free from concern. I notice myself being more and more affected by the daily chemotherapy, feeling more fragile, more vulnerable. I have already had one bad respiratory illness this summer, and I worry about the school year and all of the potential colds and infections that will be transmitted. I don’t want to think about the ways cancer affects my daily life, but I must. The decisions I make about activities, treatments, and chemo all directly affect my life… both in length and quality.
I push myself to do the most I can. I try to do all of the little things that add up to a full day: school supply shopping, back to school haircuts, camp laundry, new shoes, sports registrations, and walking the dog. I also request meetings with school administrators, coaches, and anyone new in my children’s lives for this fall that need to know how my kids’ home life differs from the one they had a year ago.
I’m a planner. I take comfort in routine, the familiar, the predictable. Unfortunately, those are now removed from my life forever. Yes, I know life always tosses everyone curveballs. That’s what life is. But I experience it in a whole new way. I have no way of saying life will ever return to “normal” or even a “new normal.” There will not be a “better”… I am not “sick” in that I cannot recover.
I still feel the drive to help, to counsel, to educate. But am finding it more difficult. I hate saying no but know I will need to start saying this more. In-person interaction is very difficult for me. While no one would know it to look at me, social interaction is extremely draining these days. I try to minimize contact knowing that when I am in public I am under scrutiny. People want to know how I am. They want to be reassured. They look at me for clues as to how things are. There is no reassurance I can offer. This is a disease of progression to the end, a story that will not have a happy ending.
I want the story that I am living to be a good one, to the highest degree it can be. I want the story for my family and friends to be one full of love, memories, and devotion. These people are the center of my world.
I want the story to be different from what it has been, different from what it will be.
As a writer I am used to editing. Revising. Changing what I don’t like.
But I can’t edit this story.
I can’t start it all again.
And so I write through it.
The only way out is through.
But this one… well, this one is quite simply going to have a sad ending, as many stories do.
August 6th, 2013 §
 Hi all,
Hi all,
I may not be posting much this month. Now that all three of our children are home from camp the house is busy and we are readying for school. Public school here starts the last week of August so we have less than three weeks remaining of lazy summer days. I will make sure to post anything important news-wise.
My tumor markers have not climbed any higher in the last two weeks though they still remain slightly elevated from levels a few months ago. Both of my oncologists feel my current chemo regimen of Aromasin + Afinitor is still working. Nonetheless, we would like to see if we can drive the number down further and erase that gain. We are still getting a sense of how much variation is normal with this imprecise test.
Side effects on this Aromasin/Afinitor combo are cumulative in severity, so the longer I am on it, the worse they will become. Currently my major issues are fatigue, immunosuppression (making travel and being in public places risky), mouth and tongue sores, joint pain, muscle aches, skin breakdown, itchy scalp, sun sensitivity, high cholesterol, high triglycerides, increased blood pressure and rapid heart rate. Loss of appetite and associated weight loss are also factors. Yes, I know: to look at me you’d never know all of these plague me. I try not to talk about them too much but they are there.
Because I know many readers will be interested in potential remedies for some of these problems, I should say that I do have all of the treatments I need to deal with these side effects. Some of them are just the way it is, and you have to just adjust if possible. Others like mouth sores and skin/scalp issues can be very successfully treated with topical steroid ointments and liquids (some believe coating the Afinitor pills with food prevents mouth sores but this is actually just a coincidence. It’s not the contact with the mouth that causes the sores, it’s the mechanism of action that does. Blocking the mTOR pathway causes oral mucositis and stomatitis. Starting initially on a smaller dose and working up to the final one does seem to help with the initial outbreak of sores though). Walking helps both the joint pain (despite initial pain) and fatigue, while occasional Ativan helps the blood pressure, heart rate, loss of appetite, and some muscle issues. These are some of a few of the things that my oncologists and I have found to help.
One of my oncologists told me I was “at the precipice” with my side effects; my body could not tolerate a higher dose (currently I take 25 mg of Aromasin and I alternate 5 and 10 mg doses of Afinitor to average 7.5 mg/day). A meeting with my other oncologist today yielded a decision between that I would increase my chemo dose ever-so-slightly to see if I can tolerate it while hopefully get a response.
This type of situation is where the art of oncology comes in. I give a liberal interpretation to the term “art.” I think it’s educated guesswork, creative thinking. The science is the foundation but the application and choices are sometimes educated guesses.
We don’t know if a small increase will affect the tumor markers. It might. It might not. Can my body handle more? That’s an unknown too.
I think of it like the old fashioned scale in the doctor’s office– the one with the weighted bars that you slide left and right until they balance. The nurse gets close to the target, then nudges the bar bit by tiny bit until just the right balance is achieved. This is what we are trying to do: balance quality of life (side effects) with maximum efficacy. Where that line is, we do not know. It varies for each person.
We’ll test again in another week (two weeks since my last one), but it’s unlikely we would see any result that quickly. At least we will see if the markers are continuing to hold steady.
As far as this website, I have many ideas brewing for blogposts soon. Readers have also contributed some great ideas and asked questions that I will do my best to answer.
As always, thank you for the continued support.
May 24th, 2013 §
 It’s Friday! I want to put a post up today because I know it’s been a while and people worry when I am not making posts. All is fine, it’s been a very busy week with a lot of routine medical appointments. Side effects from the new chemo are starting in and phrases like “mouth sores”, “high cholesterol,” and “follicular head pustules” make me certain that the person who called it “crazy, sexy cancer” was delusional about what cancer really is. There’s a lot that’s crazy but I don’t personally find a lot of sexy in it.
It’s Friday! I want to put a post up today because I know it’s been a while and people worry when I am not making posts. All is fine, it’s been a very busy week with a lot of routine medical appointments. Side effects from the new chemo are starting in and phrases like “mouth sores”, “high cholesterol,” and “follicular head pustules” make me certain that the person who called it “crazy, sexy cancer” was delusional about what cancer really is. There’s a lot that’s crazy but I don’t personally find a lot of sexy in it.
I’m getting help from my team in dealing with all of the side effects and have more appointments with more specialists in the next few weeks. For now things are stable and the next two weeks will proceed as planned. I’m still on Aromasin (25 mg/day) and Afinitor (7.5 mg/day). It’s the Afinitor that’s kicking in with my various problems. My tumor markers have shown a response to this combo over the last 6 weeks so we continue with it for now. I also received my monthly injection of Xgeva to strengthen my bones.
I wish you all a good Memorial Day weekend, especially our military personnel and their families.
The photo above is from 2002 by the way… where have eleven years gone?
I also want to mention that my last post, “There’s No Room for That in This (Six Minutes)” is the foundation for what is now a song titled “Six Minutes.” Over the past few weeks musician Doug Allen and I have been working hard on it and we’re almost done. I wrote the lyrics and he found the perfect music to bring those words to life. We are both so proud of the song and will be sharing in the future. His latest CD is available now and I just love it; it has two songs that have been on movie soundtracks… who knows where “Six Minutes” might land! More to come on this project.
………………………………
I get a lot of emails and comments with questions about cancer and how to help those who have it. Let me say clearly that I never think I speak for everyone with cancer. I do believe that asking questions is good, and even if you don’t think my answer is right for you, at least you might look at the issue a different way and clarify your own thoughts.
If people like this format I may continue to post letters/responses more often. I have often thought we need a grief/loss/illness etiquette column and I’ll gladly do my best to help.
This week I received the following excellent question.
……………………………..
Hello…
I’m a 31 yr old only child whose mother was just diagnosed with squamous cell carcinoma a week ago.
I’m going home for the first time (parents in WI, I’m in IL) since the diagnosis and after reading this blog, I’m not sure what I should say to her. She is a pessimist by nature and already saying she would refuse chemo (the details of her condition and treatment plan are still in the works) so my dad and I need to figure out a way to keep her positive so she can indeed have the support she needs to fight it. I bought some colored paper and was going to list “reasons why you are a fighter” as well as post some motivational sayings/quotes on their bathroom mirrors, but the ones that came to mind now seem like the ones you SHOULDN’T say “you can do this,”,”stay strong,”
Do you have any suggestions on what I could write? Please keep us in your prayers, I am obviously terrified of the road to come.
—– J
……………………………..
My response:
A few quick thoughts for you, J. I am so sorry about your mom’s diagnosis.
My first thought is that you all need time to adjust to the news. The way you react initially is not always the way you feel once you get your feet back under you. She needs a bit of time to not only adjust to the news but also to make this treatment plan. She doesn’t even know yet what she will be potentially recommended for treatment and yet you are expressing desires to coach her on how to feel.
Being supportive does not necessarily mean keeping her spirits “up.” Maybe what she needs right now is support for how she actually feels, not pressure to be acting a certain way. The best way to support her is to listen to her, and not try to tell her how she should feel. Let her adjust. And most importantly, respect whatever she chooses.
We love our families more than anything, but it’s her choice to make how she wants to live her life and how she wants to treat her cancer. It’s enough to deal with these diagnoses without feeling you are carrying the emotional burden of your loved ones on your back too. It will mean that she will know everyone rises and falls on her actions. That’s a huge weight above and beyond the physical and emotional toll she will be going through.
One of the most important things to do is to ask her how she thinks you could help her the most. I have a feeling putting up signs is not it, especially if you say she is a pessimist by nature. Signs around the house won’t change her attitude if a lifetime of experiences haven’t. Loving her, spending time with her, helping her with things that she might have trouble doing… those might be better. The key is to ask, really listen, and then respect what she says. Her needs might change (doesn’t want or need help now but needs it in the future) so you have to ask again during treatment.
If she decides to refuse chemo it will be tough, but it’s her choice. Chemo is very hard and is a quality of life issue too. Depending on what they are recommending and what the ultimate details of prognosis are, it’s important to respect what she opts to do while still encouraging her to see the benefits (as described by her doctor).
Those of us with cancer know everyone wants us to be “strong” and “positive” but it’s what we need to hear the least. It’s not like we haven’t thought of that already; it often just makes us feel like people are telling us how we should act because it makes it better for them if we act that way.
Negative emotions are normal with cancer, especially only one week after diagnosis… how could they not be? Not feeling free to express them may just be one more way she feels burdened by this disease right now.
Clearly you love her and want to help. The fact you are concerned with the best way to support her shows wonderful affection. The best way to do that right now, so soon after diagnosis, is to ask, and then respect what she says… That’s my best advice right now.
She will need time, but ultimately I think that she will be grateful for being allowed to express her emotions both negative and positive. I wish you all the best. Please keep us posted.
April 12th, 2013 §
I want to just send out a quick clarification about my chemo because I can tell from messages I’m getting that I didn’t explain well what has happened with my discontinuation of Xeloda. This particular chemo is now failing, yes. But that doesn’t mean it didn’t work. This is part of this disease of metastatic breast cancer. In some cases the treatment option never works; that is, your cancer doesn’t respond at all. You get no benefit from day one. You abandon it quickly.
Mine, however, falls into the other camp: it did work for a period of time. It did what it was supposed to, just for not as long as we’d hoped. That is, it did reduce the amount of cancer in my body for a while, it did hold progression at bay.
It’s no longer doing that, my counts are very slowly rising, but that doesn’t mean it “didn’t work.” It just means it didn’t work for as long as I would have liked.
Most people with advanced disease will be leapfrogging around all sorts of agents (chemo, anti-hormonals, etc.) to try to see what works. The cancer mutates and becomes resistant to most treatments that will get used. That’s when it’s time to move on to a different one. I know people that have been on at least ten different agents. That leapfrogging is just the nature of the path many others and I are on. A small percentage find one that works and it continues to work for a long, long time. Research is needed to find out why these particular cancers are more easily tamed. We do not know now why that is the case but researchers are learning more and more about the subtypes.
So while the stability was not as long as we’d liked, in this particular case it doesn’t mean it didn’t work. It did. For six months. But now we’re moving on.
In my case, because my cancer is estrogen-receptor positive, we’re trying anti-hormonal agents. Although I don’t have ovaries to produce estrogen, the fat cells and adrenal glands in my body still produce estrogen. I will be taking two drugs every day now, Aromasin and Afinitor. The plan is in place and I’m already starting taking them, slowly on the Afinitor because it has a side effect of bad mouth sores if started at a full dose. I won’t go into other side effects here because I don’t know yet what my particular response will be.
Thanks for all of the notes of support and concern over the last 48 hours during the PET scan and this new adjustment. As always, I can’t respond to every message but I do appreciate them all.
April 9th, 2013 §
 In the still of the evening I hear the frogs waking up to Spring.
In the still of the evening I hear the frogs waking up to Spring.
I hear the creak of the floor as my daughter walks around her room,
Sets things just so,
Murmurs to our dog.
In the still of the evening I hear a car,
A train,
A neighbor calling his own dog home for the night.
In the still of the evening my mind wanders again.
Back.
Always back.
I finished my 13th round of chemo 48 hours ago.
I wonder what is going on inside my body.
I wish I could see.
I wish I knew.
Is it working?
Is this round the one that will show evidence of chemo failure?
Will I move on to a new treatment?
One step closer to the end?
Every time I bang against something,
Every time I feel a twinge,
Every time that fractured bone aches,
I pause.
The pauses add up to moments.
The moments add up to minutes.
I reel them back in like fishing line, I show them who’s boss.
Just listen, I say.
Listen to the frogs. The creaks. The murmuring. The train.
Just listen.
Just hear the quiet,
Hear the house going to sleep for the night.
Feel the love.
Be grateful you can.
March 28th, 2013 §
 Limboland is part of stage 4 cancer. On a daily basis I don’t know what’s happening inside my body. I often think about the cancer cells and wonder what they’re doing. Are they dying? Multiplying? It would be so nice to have a reliable blood test to easily and accurately measure how many of them there are at any given time. But these tests do not yet exist for us.
Limboland is part of stage 4 cancer. On a daily basis I don’t know what’s happening inside my body. I often think about the cancer cells and wonder what they’re doing. Are they dying? Multiplying? It would be so nice to have a reliable blood test to easily and accurately measure how many of them there are at any given time. But these tests do not yet exist for us.
My CA 15-3 test again showed a slight elevation from two weeks ago. The numbers have been bouncing around over the last few months (expected) with a slight upward trend (undesirable). It’s hard to know what this means. A few points here and there are not cause for alarm. This volatibility is inherent in this test (which is why some oncologists don’t do this test at all, and why it can’t be used as a screening device. Also, in some people the test doesn’t reflect changes in the amount of cancer present at all). So… it’s a bit to me like trying to juggle Jello.
Of course I want to walk in and have my number be lower than the previous time. But that’s not always possible. With the exception of my hands I’ve felt good for the last two weeks. I’ve been in a frenzy of activity this week with Tristan’s 7th birthday this weekend (more about that in the next few days) and lots of activities with the kids. How I feel is important; while blood tests can show how my counts are, lack of pain in new areas is good too. I received my monthly injection of Xgeva today as well.
I’m back at Sloan Kettering next week and Dr. Dang and I will huddle and strategize. Today my local oncologist and I talked about some ideas about how to treat this test result and what it potentially really means. Right now it seems we are in watchful waiting (not that there is anything new about that). As of today no repeat PET scan is scheduled. We will see if that decision changes next week. My prediction is we wait two more weeks to see where the levels are then and re-evaluate at that time.
Chemo starts this Sunday. I’ve been doing the maximum recommended dose for 5 days, and a slight decreased dose for 2 days. I think this time I’ll be pushing to the maximum dose for all 7 days. It’s hard to know what price I’ll pay for doing so, especially during a very busy week next week (Sloan appointment and then another gig on the Doctor Radio Oncology Show on Wednesday at 1 PM which I hope to attend in person). My hands are my biggest issue, this is just what happens with Hand/Foot Syndrome. I continue to treat my hands with all sorts of products and care, but the truth of the matter is that this is what Xeloda does when it is taken and leaches out of the capillaries. The only true remedy is a decreased dose or discontinuing it altogether. That’s not in the cards right now (thankfully).
It is always hard to hear news that’s not what you want. I’m sure some people would be filled with anxiety and upset after this type of news. I like to give myself a ten minute pity party and then get on with life. If I give myself up to worry and dread for the next two weeks, what have I accomplished besides ruining two precious weeks of my life? Instead I went to the grocery store and stocked my house with food for the long weekend. I came home and played with my new dog (sweet Lucy is especially lovable in times like this).
I am a role model: my children are watching how I handle all of this. Raising polite and kind children is not enough. My children’s mastery of resilience is as important as any other life skill I can teach them. If I become debilitated by anxiety, don’t pick myself up and press forward, I am teaching them a lesson they do not need.
It’s okay to be emotional or upset at bad news. Complete denial serves no one. Acknowledging emotions of anger, sadness and fear but still displaying strength, stamina and persistence is what I try to do.
I hate the turn my life has taken. I hate that this is what is happening to my family and to me. For now, though, I continue to focus on all of the things I can do, and am doing. I pour my heart out on this screen. Some people think I must be depressed all of the time if I have these dark emotions evident in my posts. I can assure you that this is not what I am like all the time. Those feelings exist, and are important. I wouldn’t be human if I didn’t have them. It’s important to get them out not only for my own well-being but also because I know many readers with cancer tell me I’m speaking for them.
So, it’s not what I wanted, but I’m not sounding the alarms. We watch, we wait, we treat. I consciously do the best I can every day. Some days I do better than others. Some days I have a short temper and take my anger at cancer out on my husband or my kids. I’m not perfect. I apologize to them. I tell them I’m trying my best but sometimes it just breaks through. They see that I am human too. I make mistakes.
I draw strength from you all every day. Thank you for your support.
March 18th, 2013 §
Metastatic cancer is an introduction to topsy-turvy world.
Things I once counted down to now I must cheer.
The first time I was diagnosed with breast cancer (stage 2, in December of 2006), I counted my chemo treatments down. “Only 2 more adriamycin/cytoxans to go,” I might say, or “Only 4 Taxols left.”
Now I’m forced to be glad for the chemo rounds.
I started my 12th round of chemo yesterday, on Sunday the 17th. After being sick with a bad cold and stomach virus this week I’m feeling not-quite-ready to start again. I haven’t had enough time to rebound and my side effects are not as reduced as they traditionally have been. My feet and especially my hands are not in great shape and I’m limited as to things I can do. For a few days I had trouble walking. Some days I can’t hold a coffee mug. Most days buttoning and unbuttoning are a lengthy challenge. Typing is sometimes painful as well.
Whereas before I could look forward to the time when chemo would be over, now I must be happy for each round. I must realize that it means another week alive, another week the drugs are working.
Another week to be a wife, mother, friend, daughter.
Another week to write, another week to love.
Another week to hope there is a new treatment brewing.
My milestones used to be measured in how much time I had invested to get through to the other side: putting cancer in the back seat. The goal was successfully completing surgeries and chemo so cancer would be more like background noise rather than an attention-greedy headliner in the spotlight.
But now all of that is backwards. I don’t count down until my treatments are over because they are going to be here for the rest of my life. That’s a hard one to accept some days. There is no “when I’m done with treatment.” Not taking chemo would mean I’ve run out of options or the treatment is worse than the disease. There is no after. There is no “looking forward to being done.” Being done now only means death to me.
This is the way it is.
Everything is upside down.
And that’s how life has felt every day since I was diagnosed with Stage 4 breast cancer.
February 4th, 2013 §
I awaken to the sound of the snowplow scraping,
Metal on asphalt, grotesque.
I didn’t move last night.
Soft bedding, peaceful house, drained body.
I lay in bed not wanting to start the day.
Friends will gather,
We will share and learn and grow.
But before we do,
when we eat,
I know I must dive headlong into the abyss.
My breakfast will come with a side dish of chemo,
A higher dose than last time.
It’s time to begin again.
Back to reality some will say when we part.
I never left it behind.
January 19th, 2013 §
I wrote this back in 2010. Just like in this week’s “I think so too” I decided to think about the history of an object.
………………………………..
I took my friend Brenda out to lunch for her birthday today. While we were sharing an appetizer, a group of four people entered the restaurant: three men dressed in business attire accompanied a woman with a knit cap on. I realized in an instant she was bald underneath that covering and postulated that the hat would not be coming off.
They took off their coats and sat down at the table. I watched them for a while, from a distance, across the restaurant. Indeed, the hat did not come off. She was bald, most certainly, and likely undergoing chemotherapy. My mind started to wander, and I started to wonder. Was she at a business lunch and able to keep working during this crisis? Was she done with treatment and waiting for her hair to grow back in or was she on an “off week” of chemo when food might be somewhat appealing?
I kept looking at her hat. It was freezing cold out today, so it wasn’t particularly out of place. But I kept staring at it. It looked handknit. Had someone she knew made it for her? Had she gotten it from the basket at the cancer center where people knit and donate hats for patients?
I wonder what she’ll do with the hat when her hair grows back in: will she throw it away? Burn it? Give it to someone else who needs it? After wearing those head coverings day after day, you don’t want to lay eyes on them again. After my hair grew back, I saved my scarves for a friend’s sister who was set to start chemo shortly after I finished. I recently saw pictures of her wearing them. It’s odd to see them, associated with so many memories for me, on her head too. Now I have the scarves back, and some have already been lent to another member of the club.
My wig, worn twice, is packed away in the basement. I will soon donate it to a charity that provides wigs to women who can’t afford them. I hate that wig. I hate what it looks like. I hate how it feels. I hate how I looked in it. Twice I wore it, and I had to keep from tearing it off every second it was on my head. It wasn’t me; I felt like someone else in it. But I just can’t get rid of it yet. It’s like a trophy for walking through the fire.
I wonder if that woman I saw at lunch today feels like that. She and her group finished their meals and left before I did. I was really sorry I didn’t get to tell her that her hat looked great on her.
December 12th, 2012 §
Tuesday’s visit with my oncologist at Sloan Kettering was informative, as always. However, the big question can’t be answered: what is the trajectory of my stage IV cancer?
There will be no answer to that for now.
We start with a chemo. We see (through bloodwork and PET scans) how the cancer responds. If it responds, I stay the course until the treatment stops working or the side effects become untenable or dangerous. There is no way to know how long that will be. Any particular chemo could be ineffective from the get-go. It could fail after months. It could fail after years. Then you go to the list of options and decide on a next chemo regimen. This decision is not always easy; you can’t know which one will be best for you. It is often educated guesswork at best. There can be many chemotherapy options and in the end, I will probably try many/all as each one eventually fails. I’ve talked to women who have gone through more than eight different chemos in the treatment of their metastases. One thing I know is that chemotherapy in one form or another will be a part of my life for the rest of my life.
There is also no way to know if you will tolerate a chemo regimen well. Side effects can be dangerous and variable. Sometimes side effects are serious enough that you must discontinue using a particular drug even if it’s effective in reducing the cancer. As you can imagine, this can be a heartbreaking proposition: find something that works but you are unable to take.
As you know from my last post I have been struggling with HFS (Hand/Foot Syndrome) from the current chemo, Xeloda. I had done some research and found some studies indicating that the selective COX-2 inhibitor and anti-inflammatory drug Celebrex has been used with some success in helping reduce the severity of HFS in patients taking Xeloda (and a few other specific chemos). I had reduced my daily dose of chemo from 4000 mg to 3500 mg for this 5th round (7 days on, 7 days off) to see if the HFS improved with a slightly lower dose. Of course it’s scary to reduce the dose of your chemo but I’ve tolerated the maximum dose for a good number of rounds. It’s normal to need to reduce the dose as time goes on.
My oncologist agreed that the Celebrex was a good thought and definitely might help the HFS. There are risk factors associated with the use of the drug but we both agree that it’s worth the small risk. So I am starting with 200 mg once a day to see how I tolerate the Celebrex and if a low dose helps I will stay with that. If needed, it can be increased to 200 mg twice a day. My hope is that the Celebrex helps the HFS and allows me to go back to the higher 4000 mg (8 pills) a day chemo dosing for the next round.
In the meantime I continue with frequent moisturizing of my hands and feet (at least 10 times a day) with a variety of lotions including shea butter, Eucerin, Aquaphor, and more. I stay away from water, do not apply heat on hands/feet, wear socks and soft shoes/slippers, and wear gloves as much as possible. My feet have been doing very well, my hands holding steady and actually do seem improved today. Here’s hoping!
I know this was a technical discussion today but I want to share it for other people in treatment who might be able to ask their doctors about Celebrex if they suffer from HFS with Xeloda. I also hope that the explanation of chemo and prognosis will be informative.
I continue to do as much as I can everyday and when people see me and say, “You’d never know what you’re going through right now,” I take it as a compliment. I was busy today with routine dentist and endocrinology appointments… you can’t ignore the rest of your body when you are treating cancer. Many other body systems will be affected by the cancer and chemo. My thyroid has been holding steady but shows signs of needing another medication adjustment. Bone treatments like the Zometa infusion I take can cause problems with jaw bones. It’s important to keep a watchful eye on your whole body and not use cancer as an excuse for ignoring routine checkups. That’s my loving nag for the day… stay vigilant with your healthcare appointments and thanks for all of your support.
January 12th, 2011 §
That chair you’re sitting in?
I’ve sat in it too:
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too:
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too:
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too:
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too:
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too:
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too:
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too:
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
No more cancer.
Don’t you think that would be amazing?
I think so too.
January 10, 2010
December 17th, 2010 §
originally published September 12, 2009
My friend Andrea found out she needs to have chemo. I cried a lot the day I found that out. Last night she emailed me that she was thinking about the whole “losing her hair” thing. She has gorgeous hair. Thick. Straight. Reddish-brown, in the sun I’d say it has a honey shine in it. She usually wears it back in a ponytail, as she says, “taking it for granted.”
I started writing her back to tell her that focusing on her hair wasn’t silly. There are many things about cancer that are real worries. One of them is going bald. Especially for a woman. And as I typed to her I realized the words were flowing fast and furious.
I realized all the things people had said to me when I was worried about losing my hair and all of the things people had said to me after it eventually happened.
Everyone wants to reassure you that it isn’t as bad as you think it is.
Some days you convince yourself it isn’t that bad.
Some days you are sure they are all lying to you.
Either way, you get through the days.
The day you take that hat or wig or scarf off and wear your newly-grown stubble or “mouse fur” out in public is a great day (My first hair was so fine and soft and thin that it didn’t resemble hair at all… I called it mouse fur because while it blissfully covered my head and was dark, it couldn’t be cut or styled).
So, for my friend, and for other women who are getting ready to start chemo (and those who bravely walk through the world every day without hair because of alopecia and other conditions), no matter what, it matters.
No matter what anyone says…
all the things they will say:
It’s only hair.
It’ll grow back.
You’ll look so pretty anyway.
With a face like yours it won’t matter.
We’ll get you a cute wig.
We’ll get great scarves.
It’ll grow back in no time.
Maybe it’ll be better after it grows in.
It might be curly.
It might be straight.
I know someone whose hair came in gray.
I know someone whose hair came in red.
I know someone whose hair came in black.
I know someone whose hair came in white.
Hers came in curly.
Hers came in straight.
Did you see hers?
It looks great.
Did you see hers?
It looks awful.
I like her better with short hair.
I liked her better with long hair.
You’re gonna look great.
I don’t know what I’d do.
I don’t know how you do it.
I don’t know how you’re gonna do it.
You are so brave.
You are so strong.
You can do it.
You can beat this.
No matter what anyone says–
It is just going to suck.
Bigtime.
You may shed many tears over this one.
It may be harder than you thought.
I’ve heard brave women say it was harder than the actual chemo.
Reports show women actually turn down the chemotherapy they need because they don’t want to go bald.
It’s real.
It’s hard.
If it weren’t,
Women wouldn’t cover their heads.
They would just walk around bald.
They wouldn’t care.
But hair matters.
To us,
To our kids,
To our husbands,
To our friends.
My hair has never been the same since chemo.
I’m not alone in that.
In fact,
My hair now grows “the other way”…
My part is on the opposite side of my head than it used to be.
I think that’s kind of neat.
There’s the way my hair was B.C. (before cancer)
And the way it is now.
It is a big deal.
Don’t let anyone minimize it.
If they do, make them go shave their heads.
Not just clipper cut.
Straight razor shave it until there’s nothing left.
Then the eyebrows.
Then the eyelashes.
And then the stuff they might not think about.
Every piece of body hair.
Of course there are jokes.
And giggles.
The Brazilian wax done for you.
It’s funny.
But not so funny.
Then when your nose hairs fall out you suddenly realize how
Much you needed them.
Your nose runs constantly.
And it’s embarrassing.
Mine dripped clear liquid constantly.
I was so embarrassed.
No one had told me about that part.
I had a tissue stuffed in every pocket.
Because there were no hairs to stop the drip.
Chemo drip.
You try to imagine what it will be like.
You try to picture what you will look like bald.
You pull your hair back,
Slick it back,
Try a wig on to see what it might look like.
But nothing can prepare you.
For that crappy day,
Two weeks in.
When you scratch an itch
Or touch your head
And take away a handful of hair
Or find it on your pillow.
And the sight of it is so sad,
But so disgusting
So repulsive,
That you need it gone.
And then if you need me
You will call me.
And I will come.
And I will cut it.
Or maybe I will just come and cry with you.
And remember what it felt like.
No matter what anyone says,
It isn’t nothing.
It is something.
And even in the scheme of all of the things to be afraid of with cancer,
How you feel about losing your hair is real.
It matters.
And I remember.
February 19th, 2010 §
I took my friend Brenda out to lunch for her birthday today. While we were sharing an appetizer, a group of four people entered the restaurant: three men dressed in business attire accompanied a woman with a knit cap on. I realized in an instant she was bald underneath that covering and postulated that the hat would not be coming off.
They took off their coats and sat down at the table. I watched them for a while, from a distance, across the restaurant. The hat did not come off. She was bald, most certainly, and likely undergoing chemotherapy. My mind started to wander, and I started to wonder. Was she at a business lunch and able to keep working during this crisis? Was she done with treatment and waiting for her hair to grow back in or was she on an “off week” of chemo when food might be somewhat appealing?
I kept looking at her hat. It was freezing cold out today, so it wasn’t particularly out of place. But I kept staring at it. It looked handknit. Had someone she knew made it for her? Had she gotten it from the basket at the cancer center where people knit and donate hats for cancer patients?
I wonder what she’ll do with the hat when her hair grows back in: will she throw it away? Burn it? Give it to someone else who needs it? After wearing those head coverings day after day, you don’t want to lay eyes on them again. After my hair grew back, I saved my scarves for a friend’s sister who was set to start chemo shortly after I finished. I recently saw pictures of her wearing them. It’s odd to see them, associated with so many memories for me, on her head too. Now I have the scarves back, and some have already been lent to another member of the club.
My wig, worn twice, is packed away in the basement. I will soon donate it to a charity that provides wigs to women who can’t afford them. I hate that wig. I hate what it looks like. I hate how it feels. I hate how I looked in it. Twice I wore it, and I had to keep from tearing it off every second it was on my head. It wasn’t me; I felt like someone else in it. But I just can’t get rid of it yet. It’s like a trophy for walking through the fire.
I wonder if that woman I saw at lunch today feels like that. She and her group finished their meals and left before I did. I was really sorry I didn’t get to tell her that her hat looked great on her.
April 27th, 2009 §
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
A cure.
Don’t you think that would be amazing?
I think so too.
 I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week.
I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week. Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.
Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.









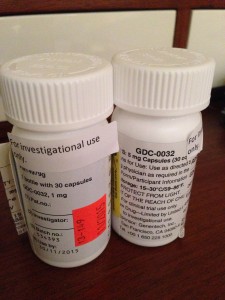











 Link to Twitter
Link to Twitter