February 12th, 2015 §
 Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.
Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.
Most of the last three weeks since I last wrote have been dealing still with swelling and blood count issues from radiation and from the extensive disease in my liver that we are working on with the radiation and with chemo. I’ve needed numerous transfusions of red cells for anemia and quite a few for platelets which have really come under attack. We have been taking a break from the Epirubicin and I got a dose of Faslodex (I had it last year as well in a clinical trial with a trial drug, this month I am using it with a daily pill, Letrozole). Rather than being cytotoxic chemos (traditional “cell-killers”) these are anti hormonal agents. We are just trying to let my body recover now for a few weeks.
Last week my abdomen grew and grew with fluid from the liver and overall inflammation. By the end of the week I had an abdomen the size I was when I was ready to give birth. The skin was painfully stretched. We needed to intervene. I went to urgent care for evaluation for a paracentesis (draining/”tap” of fluid). My platelets were too low. They transfused and I just made the cutoff. The process is pretty simple: visualize if the pocket of fluid is drainable (tiny pockets would not be) via ultrasound.
Three needles of increasing gauge are inserted to numb through to the pocket. A catheter is inserted and attached to a drainage bottle that has a bit of vacuum to draw out the fluid. Two and one half liters later we were done. It is a huge amount to see. I did have soreness at the site and discomfort from such a lot of fluid removal after. But this is a very common procedure with metastases to the liver (please, please remember: breast cancer that metastasizes to the liver is not liver cancer. Mets to the brain are not brain cancer. They are breast cancer cells that have moved in the body. There can be/are big differences in terms of prognosis, treatment, chemotherapy agents, etc).
Some patients only need a few of these abdominal taps. Some need them every few weeks depending on how chemo, etc. are working. Sometimes a drain is actually placed to allow a constant ability to remove fluid.
If you were following me last year you know I had a drain placed in my lung while in the hospital that accomplished something similar. I was fortunate to only need that one for a few weeks (I had already had a one-time tap on my left lung called a thoracentesis). For now there are no plans for a drain or other more serious interventions in my abdomen. Now that my potassium levels are holding steady we are using diuretics to manage the issue.
We are working on the plan for next week, it is likely that I will be going back to a chemotherapy called Xeloda (these are pills taken daily) for a bit because it is gentler on blood counts. I’ll update when we have a decision on that.
I’m weak, still unable to drive, or do much more than walk than to the bathroom or a car that is picking me up. I’ve had to adjust some things at home including bathroom rails and so on. Safety is most important and especially with very low platelets falls and any bleeding or injury risk is a serious concern.
I’m sure I’ve forgotten something (or things) but I do want to get this out today. I see snow out the window but I’m still focused on Spring. These hydrangeas in my room this week reminded me March is not far off.
Thank you to those near and far for all different kinds of support given this month with an extra shout-out to my wonderful team at Sloan-Kettering. If any of my doctors, nurses, or support staff there are reading this: you help make these tough days better. I value your care always.
January 17th, 2015 §
 Hi everyone… finally an update. I know I have been quiet. As you probably assumed, it has been a very difficult month. I finished whole brain radiation (and I needed to add the C2 vertebrae) and liver radiation a month ago. The brain and liver were two week regimens each but the start times were staggered so it took three weeks to complete. I was having trouble with my magnesium and potassium levels and those needed to be addressed. As a result I needed to be at Sloan-Kettering every weekday for more than 30 straight days between radiation and the aftermath. It was quite a schedule.
Hi everyone… finally an update. I know I have been quiet. As you probably assumed, it has been a very difficult month. I finished whole brain radiation (and I needed to add the C2 vertebrae) and liver radiation a month ago. The brain and liver were two week regimens each but the start times were staggered so it took three weeks to complete. I was having trouble with my magnesium and potassium levels and those needed to be addressed. As a result I needed to be at Sloan-Kettering every weekday for more than 30 straight days between radiation and the aftermath. It was quite a schedule.
In the last few weeks my problem became swelling (edema) from inflammation from the liver radiation. My abdomen was shockingly distended and that was causing me trouble with discomfort and moving around.
I have had fatigue but it hasn’t been the sleeping-all-day form that I was warned might happen with the brain radiation. Fatigue encompasses more than just “tiredness.” For me the fatigue has been more weighted on weakness. I have had a lot of trouble walking and doing steps. I’ve needed to use a wheelchair at SK for a few weeks now. That shouldn’t last much longer as I get stronger to walk distances again. But on the bad days I couldn’t get more than down to the car for my ride.
I started Epirubicin for my chemotherapy a few days after radiation finished in December. It is dosed based on liver function so the dose has been adjusted each week as we see how my liver is doing post-radiation. I was able to get three straight weekly doses. This current week has been my “off” week; my blood counts are low from three straight weeks of chemo (to be expected in anyone getting it) so a week off is always given for the body to hopefully make enough the replenishment cells of different types.
The magnesium and potassium as of this week are finally holding with home management and no IV supplementation. A helpful tip: the low sodium form of V8 has huge quantities of potassium. Most people think of OJ or a banana to supplement. Only 8 oz of it contain 900 mg of potassium. I drink a few a day, just make sure it is the low sodium version though.
I’ve now tapered totally off the very low steroid dose I had been on for months. Steroids can make your legs very weak if you take them for an extended period of time so it is good to be able to remove them from the equation.
I only needed to go to SK for one trip this week. Diuretics have helped with the edema, each day I see and adjust the dose. I do not have pain beyond what is caused by the fluid around the liver. I do not take any pain pills and haven’t needed them during radiation. I have not had any headaches or neurological issues yet from the brain radiation which is probably due to the fact that my lesions were so small and the low dose of steroids. I am still winning a bunch of my Words with Friends games too! The last time I was able to leave the house to go somewhere except to go to Sloan-Kettering was Thanksgiving. That boggles my mind.
I think this week has been a turning point. I am hopeful the major acute radiation effects are waning. No clue what lies ahead with the delayed ones but I don’t focus on that. For now I will be working on strength (after being basically bedridden for a month) and trying to get more function back. It is a process.
If all goes well I will start a new chemo cycle next week. Radiation effectiveness can’t be assessed immediately so we will do preliminary scans in a few weeks. (I finished on 12/19). Each day is different and I can’t predict how I will feel. But that seems to be the way life will be for me now. I long ago adjusted to that.
I am grateful for all of the support and concern shown over the last month from you, I understandably wasn’t able to return many messages. This past month was really about just getting through. The energy I did have was spent making sure the kids were able to maintain their usual schedules and we made it. Friends who have helped with rides and meals: thank you.
The poppy photo above is from my garden a few years ago… I’m already anxious for Spring to get here. xo
December 27th, 2014 §
 Hi all, a short update.
Hi all, a short update.
I’ve finished two weeks of whole brain radiation (those two weeks had simultaneous radiation to my C2 vertebrae), and two weeks of liver radiation (one overlapping with brain, so all of this was 3 weeks of treatment). I have been overwhelmingly plagued with intense fatigue and other side effects (fatigue is the worst thing at the moment though).
I need to use a wheelchair when I go to Sloan-Kettering now. I’ve needed platelets and red cells once each in the last few weeks and have needed to be at Sloan for one half-day every weekday for the last month or so because my magnesium (despite daily infusions) remains critically low, which is a dangerous situation. My potassium has similarly started to be an issue as well. I get magnesium and potassium in addition to 1.5 to 2 liters of fluids as well each day because I have been having trouble staying hydrated with the radiation effects. Not enough energy here to go into why the magnesium is still an issue now.
Four days ago on Tuesday the 23rd, I began chemotherapy (4 days after finishing all of my radiation). We are starting a new drug called epirubicin which is an anthracycline just like the well-known adriamycin (it is also red like adriamycin).
So basically I’m spending a half day at MSK every weekday and resting (I’m basically bedridden right now) at home the rest of the time. I don’t leave the house except to go to MSK. I expect at least a few more weeks of this.
I’m thrilled that my family has gone away on vacation starting today and they will have a week to ski and be with cousins and grandparents and get a fun break while I recover here. I insisted that they go; it is so important for me to know that our kids and my husband can have some vacation time and get a break. It is not easy to be a family member/caretaker under these conditions so it gives me a lot of joy that they can have a change of scenery. I have a family member staying with me since I can’t be alone and so that will work out just fine in terms of appointments and help with my needs.
I get foggy quickly so I hope this post made sense!
Many thanks as always to those who support me daily with tweets, emails, rides to appointments, donations to my research fund, meals, etc. And to any MSKCC staff who are reading this: you know how much I adore you.
I am grateful that you all continue to join me here. Wishing you a happy and healthy new year if possible and we’ll keep on going into 2015 the best we can…
xo,
Lisa
November 19th, 2014 §
 Nothing poetic here today. Just a report.
Nothing poetic here today. Just a report.
The past week was already one of the most challenging I’ve had this year: my first infusion last week of a triple dose of Cisplatin had me down for the count while I was also digesting the news of the growing liver metastases and what needs to be done to try to reduce those. This week I had a PET scan and CT angiogram of the liver scheduled to assist in my pre-surgical requirements for the Y90 Yttrium radioembolization I talked about in my latest update (the Y90 process is also called SIRT: selective internal radiation therapy).
As a result of the PET scan we got some additional information and what we got was not good. Obviously that isn’t a surprise given that my bloodwork had already told us the prior chemos had stopped working and the cancer has been progressing. The PET confirmed that my liver is an area of increasing trouble with tumors multiplying and growing in size. Not surprising. Also as we suspected, the fluid around my heart appears to be malignant. Then there were surprises: apparently at least one malignant lesion in my brain and new cancerous areas throughout my skull and jaw.
The PET is not a good way to identify exact size and precise location of specific tumors, however. Therefore, on Friday I will need a brain MRI to get good imaging and see exactly what is going on. Then we will see what needs attention, what is watch and wait. Not all brain lesions should be radiated with gamma knife surgery immediately; it is a risk/benefit assessment when you’re shooting radiation into the brain. Obviously, though, gamma knife surgery is a treatment that will be considered once we have details on what we are looking at.
Skull metastases, despite sounding scary, are just bony mets. This is what systemic chemotherapies (treatments that are given orally or through IV that work throughout the whole body) are designed to work on. Brain lesions often need different therapy because many/most drugs do not cross the blood/brain barrier (or do so in an indirect or imperfect way) and so are not effective in counteracting metastases to the brain. Metastases to the brain often require a change in therapy to address this issue.
For now we proceed with the liver plan because that is a local therapy designed to work on just that issue. It needs attention now and isn’t changed (yet) by this new information. As for the rest, I will just have to see what the brain scan shows and go from there. It will be a long week of tests and waiting. Sometimes I wonder how I walk around knowing what is in me and what it is doing to me and still manage to get through the day. I have seen the roller coaster of what this disease does. Some things that sound terrifying end up being able to be managed.
We will be scheduling chemo intermixed with my liver procedures (day before, or maybe a few days after), adjusting the chemo doses to lower ones so that there is time for my blood counts to rise in the time needed. It will be an art and science to balance. By then we will know if the Cisplatin is working. I can only hope that it is and that it will. We have a few choices lined up for if it isn’t.
While all of this goes on I still search for that laugh, I still appreciate the small things.
Most people know my “bit of beauty” tweet by now (“Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.”). Judy Clement Wall has made this into notecards and a print and is donating all funds from sales through 2014 to my research fund at Sloan-Kettering. If interested, go here to her Etsy shop. I know that this is the quote many people will remember me for most. But I have another tweet I like to send out. Some days this one just feels right. It is:
Make the most of this day. Whatever that means to you, whatever you can do, no matter how small it seems.
For now, and again, I say: Onward.
(A housekeeping note: for anyone who has signed up to receive these posts by email but sees that posts aren’t arriving: you must confirm your subscription by clicking the verification option in the first email you will receive. If you have been wondering why you aren’t getting the emails, please re-sign up from the home page at www.lisabadams.com, upper right corner, and make sure to verify. There are loads of unverified requests and only you can do this part!)
November 7th, 2014 §
 This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
Unfortunately, what I learned while reviewing the scan with him is that I don’t just have two tumors in the liver. Instead there are actually many tumors in my liver, with those two being the largest. The fact there are so many tumors is why I am not a candidate for external beam radiation or other non-invasive treatment.
So far I am still a candidate for the Yttrium 90 radioembolyzation procedure where radioactive beads are inserted via a catheter snaked up through the groin into the hepatic artery and subsequently “feed” the tumors radioactive material as the beads work their way into the liver.
It will take three separate procedures spaced about two weeks apart to get this done. I will start the first week of December and finish in January. The first procedure involves mapping things out (in essence, a “dry run” where mock beads are inserted) and the next two are actual placement procedures. This is all a joint approach between interventional radiology and nuclear medicine. Before I start I will need a CT angiogram of the liver and a PET scan. After treatment I will have to monitor progress with PET scans every three months.
In the meantime we need to start on a new IV chemotherapy right away to try to see if we can find a chemo that will work on the liver tumors. We have no way of knowing if we will find one or what it will be. Right now my oncologist is eyeing Cisplatin, a platinum-based chemo like the Carboplatin I was on this summer. We will make the decision by next week and begin then.
The liver situation is serious. The cancer is growing rapidly there and we need to get it under control. Results of using Yttrium 90 for breast mets is pretty good, definitely good enough to proceed with it. To be honest, it is not a choice about whether to do it (I’m not at a point where I would consider doing nothing and stopping treatment, I realize that proceeding with any type of treatment is a choice in and of itself). There aren’t other options to treat these in a “batch” way.
So, there is a lot of adjustment right now. I feel sadness, disappointment, and anger that chemo has worked so well in some areas but the liver has been resistant. Things change so fast with this disease. One day things are relatively stable and within weeks they can be spiraling out of control.
As always, I will continue to educate and do what I can to show what my life with metastatic breast cancer is, what life with the disease can be.
For now, I will begin a new chemo and proceed with plans and pre-surgical testing for December. I’ve appreciated the emails and comments so much and I thank you all for your concern and wishes. I am sorry that I can’t respond to them all individually.
November 2nd, 2014 §
 Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Monday I saw my cardiologist to try to get some information about some symptoms I’d been having. My echo (and later in the week, the CT scan) showed there is some excess fluid around my heart. For now it is not causing any effect on heart function but we can’t rule out that it is a problem. I’ll have to repeat tests in a few weeks to try to see if it grows in volume (this would indicate a more sinister issue, and we would need to rule out a malignancy). For now, though, that goes on the back burner.
Tuesday I had bloodwork and IV fluids. The bloodwork is still a bit unclear about if the current chemo (Navelbine) is working. The rise in tumor markers is slowing but we need some definitive results this week, I think, to feel confident in interpreting them. The bloodwork also revealed I was anemic again, so on Thursday I went to New York City and got a transfusion of two units of blood.
On Friday I had a CT scan to compare to my last scan and help us make decisions about treatment. The CT showed both some good news and some concerns. While the lymph nodes and malignant tissue in my chest have resolved (chemotherapy in the last six months has worked and reduced those areas), my liver unfortunately shows two tumors.
The best thing at this time would be to biopsy portions of them (to gather tissue for future testing; my cancer has rarely been in areas that we can actually get samples, so this presents a rare chance to grab some) and also do ablation on them. Ablation is a localized procedure that when successful, destroys tumors of a particular size with very few side effects.
So, a lot is up in the air at the moment.
Because it is only Monday morning I don’t know what this week will bring in regards to chemo. We also don’t yet know if the interventional radiologists will decide that I am a good candidate for the ablation. For now, I wait.
Palbociclib, a drug I received through the expanded access (formerly “compassionate use”) program from Pfizer should arrive this week. That process took approximately 9 weeks and usually takes longer than that. I am fortunate my oncologist kept the process moving in such a timely manner (all applications and documents for such use must be done by the physician, not the patient).
I’m not feeling that well and have been primarily staying home for the last month. Now that I think about it, though, I’ve been basically staying home for the last ten months. Many days my half hour in the morning driving the older two kids to school is my only outing of the day. But I am patient.
At this point the options are still very reasonable and typical for this stage of the disease. I’m waiting for the next treatment proposal and then onward we go.
December 29th, 2013 §
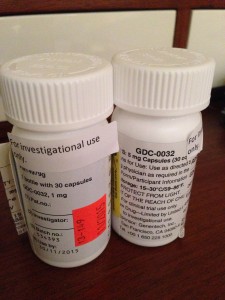
 No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
Everyone kept telling me how great I would feel after the thoracentesis. I did feel like I was breathing easier, but I didn’t feel great. In fact, I had quite a bit of pain. They checked for an air leak by x-ray as they always do after this procedure. There were no visible complications. But there was still tremendous pain starting that day and increasing into the next. It was more than the pain from the reinflation of a lung that had been compressed by half its size. But exactly what it was we weren’t sure.
By Thursday when I had to go back to Sloan-Kettering for my PET scan, echocardiogram, and EKG I was in agony. One of the doctors I met with could see how much pain I was in and prescribed some narcotics. I can’t take anti-inflammatories because I am having a liver biopsy next week and they put patients at risk for bleeding. I am so grateful a doctor seeing me about paperwork reached out to offer assistance and relief.
My father met me in the city. After I completed the required tests he drove me home. I can’t think of anyone better qualified to keep an eye on me than a retired cardiothoracic surgeon. Unfortunately, the pain continued. In all likelihood it is a combination of the cancer causing inflammation in the pleura and some nerve inflammation now that some of that fluid is gone and the lung is reinflated. It’s really all conjecture. We will see if the scans and tests reveal any additional information.
Oxycodone couldn’t keep the pain under control so yesterday I had to combine it with a Fentanyl patch. This duo is definitely helping me more; I’m still in pain but it’s more manageable today (Sunday). Each of these patches lasts for 72 hours and will deliver a constant stream of medication to me. I am pretty much bedridden.
It’s looking like Tuesday (New Year’s Eve) will unfortunately be a tough day. I was already scheduled to have a liver biopsy (This is not to check for malignancies; we already know there are metastases here. This procedure will be for repeated genomic sequencing analysis and other testing to make the best choices about chemotherapy and future clinical trials). Now, given all of the events this week, the team has decided that I need to have a PleurX catheter put in. This is a drainage system that will allow me to remove excess pleural fluid at home rather than having to have it tapped with a needle each time it builds up. The catheter will stay in place only as long as I need it, which will be as soon as treatment starts working and the fluid stops being produced in such copious amounts. I assume this will be at least a few weeks.
Having these two procedures and pain control issues means I will need to stay overnight in the hospital for observation. It’s amazing the lengths some people will go to to be in NYC for New Year’s Eve fireworks, isn’t it? Maybe Anderson Cooper will swing by while I’m recovering.
Once we see the results of all of the tests I’ve had and have these two procedures behind me, we will re-assess the plan to start the second clinical trial on Thursday. The most important immediate tasks at this point are to treat the two symptoms and get my breathing and pain under control. Immediately after that we go to work on the metastases to stop the problems at their source.
Thank you for all of the support I’ve had over the last few days including local friends who have been so kind and some friends who came from quite a distance to keep me company this weekend. I’m just putting one foot in front of the other and doing everything I can to gather all of the information I need to make a decision about what the best next step is.
Of course, as much as I can, I’ll keep you posted. Twitter is always the best way to keep up to date on daily happenings. It’s a lot easier for me to get quick bursts of info out in that medium. So many have asked: I have all of the help that I need and respectfully ask for no visitors or gifts during this time.
I would like to wish you all a happy and healthy 2014 if I don’t post again here before we all ring it in.
December 18th, 2013 §
 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
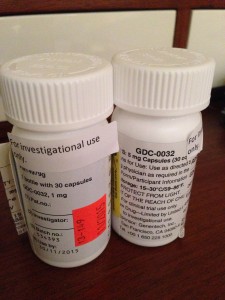
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.
October 18th, 2013 §
 I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I confess I have putting off writing this post. After getting results of my scans I needed a few days to just sit with the information. I have also been dealing with some physical issues during my washout period (an interval where you must be chemo-free) before my clinical trial starts on October 28th.
I had CT scans of my chest, abdomen, and pelvis. I also had a bone scan of my body. I had bloodwork and an EKG and a urine test. These are all tests that need to be done before I can start the clinical trial and will be used as my baselines. Monitoring will happen at frequent points throughout my treatment. Bone scans and CT scans will be done every 8 weeks for the first 6 months and every 3 months thereafter for as long as I am on the protocol. I’ll write more about the trial and the drugs (fulvestrant and GDC-0032) when I get underway on the 28th. I had a lot of trouble with with the blood portion as I only have my right hand and forearm for blood. It took six needles in that area (which included two blown veins) to get all of the radioactive tracers in and blood out. I will be discussing the option of putting in a port at my next appointment.
So the short story is that results were not as I’d have hoped. I wanted it to be clear that the cancer was still confined to my bones and lymph nodes, even if it were in more bony locations. This, however, is not what it seems to be.
First I need to explain about the tests. I’m going to briefly try to explain why it’s a bit of apples and oranges to compare my test from August with my tests last week and why all of it is a bit jumbled. In August I had a PET scan. In oversimplified terms this test picks up on high activity metabolic areas. So, cancerous tumors (and also some false positive areas on occasion) “light up” because they have a high number of rapidly dividing cells. It measures activity. CT tests, on the other hand, are static. They are like x-rays. They just take a picture without regard to whether the nodule/lump/tumor etc. is malignant. It shows there is something there but can’t necessarily tell you what it is in terms of metastatic breast cancer. CTs are very precise visually. PETs are not necessarily so. CTs in my case can’t tell us for sure if a spot is malignant.
I now have a small spot showing up on my liver that wasn’t visible on the PET in August. So is it a new metastasis? Or is it a benign spot that just didn’t show up on the PET because it’s not cancer? Who knows. We will have to wait and see if it changes when we do the next scans 8 weeks after the trial start (10 weeks from now). There are also nodules in my lungs and pleura. These are potentially (likely) malignant but the ones in my lungs have not changed size in 8 weeks.
I think that’s as much detail as I need to go into. The worst spots in my bones are my T12 vertebrae and my first rib/clavicle area. There are many spots but those are the ones that cause the most pain.
Unfortunately and most significantly at the moment, the scans also showed that the small pleural effusion (fluid in the lining around the lungs) has grown.
So we have many question marks with a few new areas of concern. For now we watch and wait. The pleural effusion will need to be drained if it grows or continues to cause breathing problems. For now any physical exertion gives me trouble. I need rest throughout the day but am trying to conserve energy for activities with the kids.
None of this news changes anything about my planned start of the clinical trial. Whatever these spots are and wherever the metastases are, the drugs I will start in ten days have the best chance to keep the spots stable and eventually perhaps shrink them. Reports from the phase 1 trial participants showed that often there was a stability period of about 8 weeks before some achieved some tumor shrinkage. I have ten more days to go chemo-free before I begin. I am counting the days. That start day is the most important day I have. A few of us in the trial are starting on that day so hopefully I will get to meet some of the other participants. There are 60 nationally in this phase 2 trial, approximately ten people will be at my location. There is relief in knowing there is no placebo in this trial. I may not respond but it won’t be because I received a placebo.
I wish I had better news about the scans but I also am resigned. This is what this disease does. I must do the best I can given my daily symptoms. There are questions marks and only time will give us answers. I try to have as much normalcy as I can, which often just feels like sleepwalking through the days and a bit of play-acting. But it’s important.
I keep coming back to a few lines I wrote recently:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
I can’t do anything more to change what’s happening inside. I have a plan and I just need the days to go by to get started. My quality of life is suffering at the moment but I hope that this will change. It is a rollercoaster, one I have been strapped inside unwillingly. Some days are good, some days are not. These happen to be some of the icky ones, but as always, I press onward.
Every morning I say to myself:
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be tough to do. Persevere.
 Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.
Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.







 Link to Twitter
Link to Twitter