 For those who wanted to hear my interview on Doctor Radio and weren’t able to listen on Wednesday, here is a link to a downloadable audio file of the one hour show. Thanks to my brother, Mark, for doing this. That show leads directly into today’s discussion.
For those who wanted to hear my interview on Doctor Radio and weren’t able to listen on Wednesday, here is a link to a downloadable audio file of the one hour show. Thanks to my brother, Mark, for doing this. That show leads directly into today’s discussion.
……………………………..
I always get some heat about posting essays about the stupid things people say to those with cancer.
I know people come here expecting to learn. That’s what I’m trying to do: educate. People inevitably vary in their responses to what people say. After all, responses to books, movies, and comedians are all over the place.
Occasionally people will get defensive and say, “Well, I have said one of those ‘stupid’ things and I meant well.” I am going to take an unpopular stance and say that meaning well isn’t always enough.
Maybe the listener is scared. Maybe they’ve had cancer or a family member with it. Maybe they are just uncomfortable talking about illness and death. It’s important to remember: it’s not about you. It’s about the person with the illness. If you are a friend you will need to get over your discomfort or get out of the way. What you don’t want is for the ill person to have to be consoling the listener or trying to minimize the seriousness of what they’re feeling.
Do not turn it back on you, or when you had cancer, or when your child or mother or 2nd grade teacher did. It’s not necessarily the same. Types of cancer are not the same. Even subtypes of cancer are not the same. Now, I’m not saying you should always avoid interjecting something to let the other person know that you’ve had experience with cancer. But the first thing out of your mouth shouldn’t be to connect it to someone else and what their outcome was, good or bad.
Different diseases cannot be compared. Different cases of the same disease cannot necessarily be compared, either. Chiming in with, “Oh, my second cousin’s boyfriend’s dog walker had breast cancer” doesn’t help a person, especially if it’s followed by “She suffered in pain for a long time and died” (yes, this gets said more often than you can imagine). The other end of the spectrum is, “Oh I know someone who had that. They’re fine now.” (Okay, but some people are not fine… should they be jealous? Feel inadequate?) Someone told me in response to learning I had metastatic breast cancer that his wife “had a bit of that last year.”
If you had a coworker who worked the entire time she had treatment, that’s great. We are happy for her, truly. But that bears no relation to how someone else can handle their surgeries, treatments, and side effects. So while you might think it’s supportive (in your mind you’re saying, “See, I’m being supportive and reassuring her that it might not be as bad as she thinks”) what that person may reasonably hear is, “Wow, if you have to take time off work you are weak, or at least not as strong as my coworker was.”
What would be something better to say to a coworker? How about “Please tell me how I can help you during this time. Is there something at work I can do to make it easier for you? I hope you know I would like to help if I can. If you can’t think of anything now, that’s okay. Just let me know if/when you do. I’ll ask again to make sure you’re getting the help you might need.”
Asking “Has this been a good week or bad week for you?” seems like a good bet to ask someone you might not be best friends with. It shows concern and they can be as detailed as they want in their response.
…………………………..
A few weeks ago someone tweeted to me, “As a cancer survivor myself, I know that half the battle is the mindset. Be determined to defeat cancer and you will!” Then followed that one up with “I meant that if we believe we can win against it, we will.”
Comments about someone’s attitude are definite don’ts. Does that mean those who die every day are responsible for their deaths because they are weak-minded? If it were as easy to defeat cancer as mindset, people would not die of it by the thousands every day.
Similarly, comments about appearance while rampant, can strike the wrong chord. I can’t tell you how many times people find out about my stage 4 diagnosis and say, “But you LOOK just fine!” The two are not always correlated, most especially at the time of diagnosis. This is why many people don’t know they have cancer and are completely taken by surprise. When people tell me “You look great!” I know they mean something nice by it. But the rest of that comment, the dark underbelly, is “You don’t look like you’re dying” or in some ways more insidious, “If you look that good you can’t possibly be that sick/it can’t be that serious.”
Don’t say you know exactly how someone feels if you don’t have evidence to back that up. Being a compassionate person and caring friend does not require personal experience that is identical to what the person is going through. Let me say that again, a different way: in my opinion you don’t need to have had cancer to be a caring friend. It might help you to be a good friend if you have had cancer, but it’s no guarantee. People “do” cancer differently. While the experience might have similarities, it doesn’t mean we will necessarily agree on how to deal with it. Part of what I try to do here is level the playing field. I try to bring you information and advice you can use so that you will know more about helping than you did before.
Don’t tell them that their science-based treatments are bunk and what they really need to be doing is just changing their diet, breathing pure oxygen, or relieving their constipation to be cured of cancer. Do not tell someone who is in the middle of treatment that chemotherapy is a waste of time. You may think your suggestions of supplements/vitamins/tea are harmless, however, there are serious interactions that can dull the effectiveness of chemotherapy and other treatments. Not all lotions are good to use during radiation treatment. Not all vitamins are good additions.
………………………….
I like what @travisbhartwell tweeted to me: “Mindset changes the days you have, not the number of days you have.”
The worst thing that can happen is that friends disappear. This is happening to me in spades. It may be that they are afraid they’ll say the “wrong” thing and end up being written about. But I think it also has to do with the fact that death and illness make people uncomfortable. I represent their fears. People who should be in touch with me at least every week or two (because that is how often we saw each other before) have just dropped away.
That said, there are so many people in my life who are so wonderful. Who offer to help, who make it easy to accept it. Who send notes or emails of support months after the initial shock. Who keep asking what they can do. Who pointedly give ways they can help and ask if I could use it.
………………………………..
One thing I think is very important is to always say to someone who is ill or has experienced a death in the family: do not write me a thank you note for this. Do not feel the need to answer this email. Do not feel the need to call me back.
If you live near the person ask them, “Would it be helpful if I texted you before I run errands so that I can pick something up for you?” Texting and email help because talking on the phone is almost always too much of an ordeal and/or inconvenient. I have friends who email me at the beginning of the week to say, “I’ll be at the grocery store, the drugstore, and the post office this week. Can I do anything there for you?” Some will text on the spur of the moment, “Running to Costco. Need anything?” These are invaluable offers.
If you have no knowledge of what information you are being told, admit it. People with serious illnesses do not expect you to know everything about their new diagnosis. They are probably learning a lot of information in a short period of time and may not even know the details of their diagnosis and treatment. They don’t expect you to have the knowledge but you need a way to connect. I recommend when someone tells you about a diagnosis you don’t know much/anything about you say, “I don’t know anything about what that diagnosis means. Would you mind telling me about it, and what it means for you?”
How is it affecting your day-to-day life and what part of that can I help you with?
I’m so sorry to hear that.
What is the worst part of this for you and how can I help make that a bit easier for you?
If your friend is dying or has a relative who is, and they refer to the death or how difficult treatment/daily life is, don’t brush it off, dismiss it, or say, “Oh, you’re not going to die. You’ll be fine. It will all be okay. Things will work out.” Saying this to someone with stage 4 cancer comes across as dismissive of the seriousness of their diagnosis.
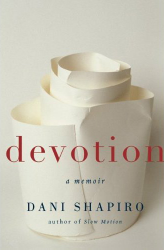
If the listener says, “Oh, that’s depressing, let’s not talk about dying,” it can isolate the person who is ill, making them feel they should not be thinking about what is a very real concern or outcome. As Julie Klam points out in her book Friendkeeping, acknowledging someone’s wishes should be paramount. She tells the story of her mother and her mother’s friend Patty who was dying of cancer. Patty wanted to give Julie’s mom a pendant. Rather than gratefully accepting it, Julie’s mom insisted Patty would wear it again, that she would get better. Instead, she died a few days later. Years later when recounting the story with regret, Julie’s mom said, “She knew she was dying. It probably would’ve been comforting to her for me to acknowledge that… I was just afraid that she had some small glimmer of hope. I just didn’t know.” I would bet that if that same scenario happened again, Julie’s mom would act differently.
Later in the chapter Julie recounts being a friend to someone who had to terminate a pregnancy. She asks Julie a question that continues to haunt me: “Will anything ever be good again?” It echoes in my mind now: Will anything ever be good again? Will anything ever be good again?
The truth of the matter is that for some it will. For some people, it won’t.
Check in with your friend intermittently. Give her reminders that she is not forgotten even if she is not out in public. I love getting cards or texts or emails that tell me what my friends are up to. As I write this my friend Kathleen texted me to say she was eating at one of our favorite places. “I miss your company” she said. How can you not love that?
I love written notes. I save my favorites. When I’m having a bad day there is something about pulling out a card, seeing handwriting, reading a message. It’s just more personal than seeing it on a screen. Of course texts and emails are great for frequent check-ins, but for a special message? Real paper can’t be beat.
Other winners to me are notes that remind me of a funny experience a friend and I had, a favorite memory. Many people know I love my garden and flowers. They will send me a pretty card and tell me what they saw at the farmer’s market or in their own garden or what they’re looking forward to about Spring. Sometimes they will tell me about being on vacation and how they thought of me when they saw the water or the tropical plants and they remembered a trip I’d blogged about.
Some send a favorite poem or story or memory. I like those. I don’t like religious quotations or cards that focus on people praying for me or hoping for a miracle. That assumes I am a religious person (I am not and I don’t believe in miracles). I think cards should focus on the person— the connection to that person, your friendship, not what types of religious comfort or explanation the writer endorses.
One Twitter friend, Neil Shurley, wrote me a song titled “We Love You, Lisa,” and then made a video with people holding up signs that say those same words. I still watch it. I always cry. It’s one of my favorite things anyone has ever done for me. This, from what most people would term a stranger. Another friend, Nichole, took photographs that people sent her, combined them with poems and sayings and turned them into a photo book for me. When I’m down it’s another thing I reach for to feel support.
Does the person who is ill have children? If so, you can do what one room mom did for me this year: For school events Lizzie always asked if I felt well enough to join on any party or field trip. She offered rides to school performances. When I could not attend, she (and other moms) took photos and videos and sent them to me… without being asked. My friend Zerlina put together a playdate calendar and a dozen moms signed up in rotation to have Tristan over three times a week for playdates for the past six months. This was especially helpful. Sometimes I’ve been well enough to say we would host the playdate here. But knowing there was fun built in with his friends was a relief to me.
Finally, I always love my mother’s suggestion for one of the best questions you can ask in any situation whether it be posed to a friend, a spouse, a child, a coworker. When someone comes to you with a complaint, a problem, or a rant asking the simple question, “Do you just want me to listen or do you want my advice?” is a wonderful way to be supportive. Sometimes a friend just needs to cry and vent, no advice wanted. By asking you will show sensitivity to the distinction. This is what I mean by not needing to have had the same experience to be a good friend. Listening matters. It’s free, and all you have to do is offer (and follow through).
And if you have a serious illness how do you respond when someone asks you how you are? If you don’t want to answer in detail, one suggestion is to say, “There are good days and bad days. Today is a … day.” This response is also a good one after the death of a loved one. If you are having a good day it allows you to acknowledge they’re not all like that. If you’re having a bad day it expresses that you know they won’t all be like that, either.
……………………………….
I think we all like to hear that we matter, that we make a difference, that we are loved. In the end, you can never go wrong by telling (or writing) someone what they mean to you, what you like about them, and what you enjoy most about being with them. This is the essence of friendship to me. Some days you need a serious chat. Some days you need a friend to be silly with. Some days you need a friend to go shopping and have a gossip session with and try to put cancer in the back seat for a few hours. There are many ways to be supportive.
My dear friend Cathy texts me every morning to wish me a good day and asks, “How can I help you today?” I most certainly don’t expect that every friend should do this. But boy, it means a lot that she does. I rarely need something these days. But I will someday. And when I do, I know she’ll be there for me.
I have so many people in my world who care. I know how fortunate I am. I hope that some of these suggestions will be helpful and I am sure you will find others as readers comment on the post. You don’t need to have many things to say… a few good options will do.
…………………………………….
I hope you all have a good weekend, we are starting to feel Spring here and boy, does it feel good!






















 Link to Twitter
Link to Twitter