Today my son Colin turns 11. All of the usual things go along with that: cupcakes, presents, hugs, reminiscing. As I looked back at the pictures of me, pregnant with him, I just can’t believe how the time has gone. Clichés are clichés because they’re true: the years go by faster and faster.
Christmas of 2001 was spent in New York City awaiting Colin’s imminent arrival. I was so huge and uncomfortable that I couldn’t get around too well. I was sure that baby’s head which felt like it was between my knees was going to emerge any second. Christmas came and went. As New Year’s approached I begged my obstetrician to induce me. Colin wasn’t due until January 10th but it was clear he was “fully cooked.” And big.
I called my parents and told them to come to the city. I just knew I wasn’t going to go much longer, and wanted backup so we could go straight to the hospital without worrying about Paige, then 3.
The morning of the 3rd of January Clarke was getting ready for work, staying home slightly later than usual after the holiday. I awakened feeling a bit off. I told him so. He lingered more, wondering if this would be the day. Shortly after 9 a.m. I said the contractions were starting. Only a few minutes apart. We called the garage for our car, but within 20 minutes the contractions were fast and furious. Out the door we went, got a cab, and started the 20 blocks to the hospital. By the time we got there I was in agony. Already a few centimeters dilated for the last 2 weeks, I knew there wouldn’t be much time.
After some (only funny now that it’s over) problems with an IV, a new nurse, and a whole lot of painful yelling on my part, I finally got into a delivery room. The nurses sent Clarke out as they prepped me for the epidural (with all of my yelling, they probably wanted to give me general anesthesia to shut me up… I was not doing well with the contractions). As I bent over for the anesthesiologist to get the epidural in my back, I could feel it… this kid was on his way out, nothing I could do about it. I sat up, yelled, “He’s coming!” as they sort of shook their heads, thinking they had time.
A nurse saw Colin clearly on his way into the world, and ran down the hall for Clarke, who had gone to the pay phone to check voice mail (pre-cell phone days). They both came running in, just as Colin came out. Literally 10 more seconds and Clarke would have missed the birth of his son. I would have loved that epidural.
He takes the cake for my most dramatic birth of the three children. At least after him, they agreed to induce my third, knowing I’d never make it the fifteen miles to the hospital here in Connecticut.
With the fullest head of black hair and 8 pounds, 13 ounces of bulk, Colin looked huge. And old. And that never changed. He was 20 pounds by four months. And always tall.
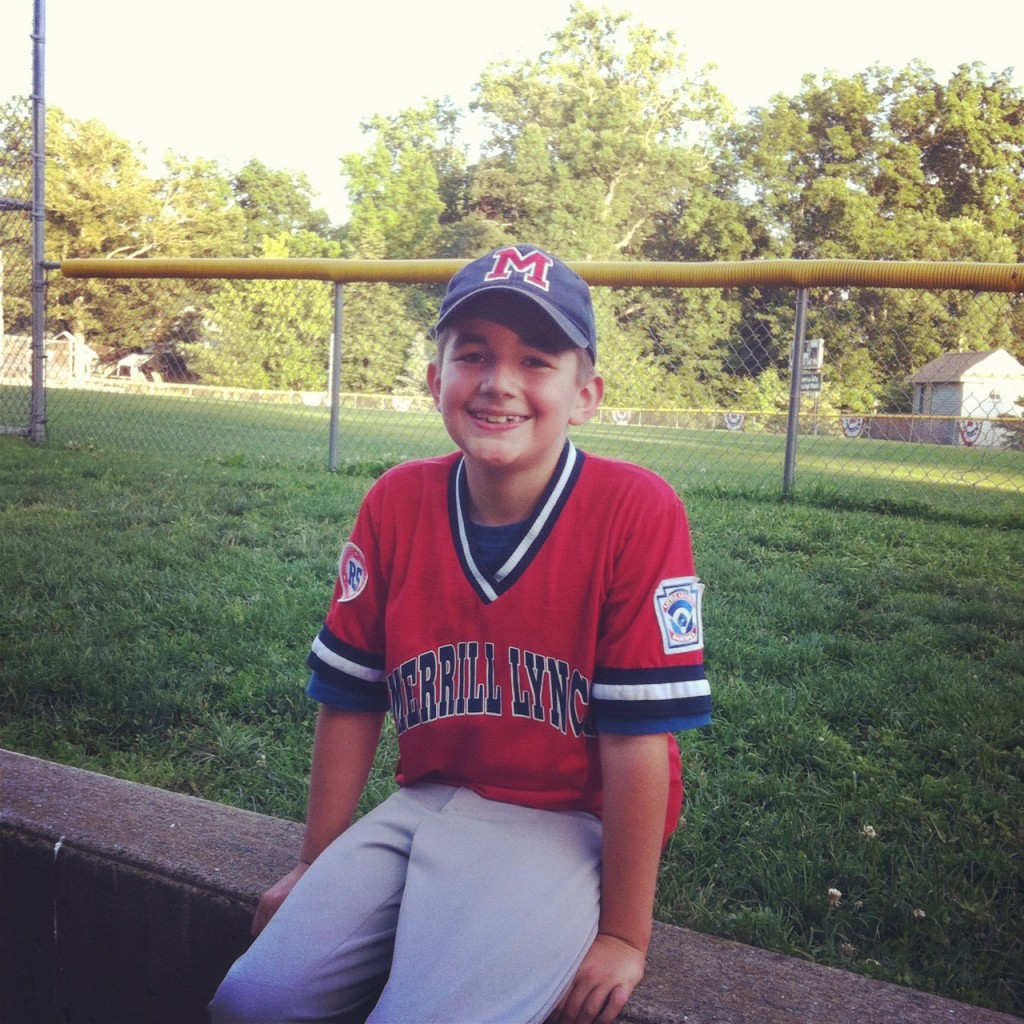
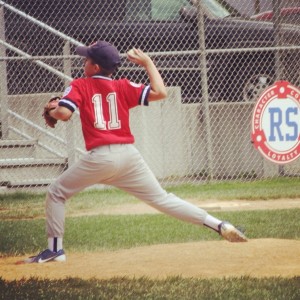
He was a challenging toddler (that’s code for “pain in the neck”) but grew into a lovely boy. He still is. He’s an athlete and quick learner with zeal for trivia and memorizing facts. He’s a caring and protective big brother and a loving football and ESPN-watching companion for his father.
I never thought I could have a son. I thought I would only do well raising girls. When Colin was born I knew we’d have to figure it out together. I can throw a football with some semblance of a spiral. I am getting used to a child who wants to wear sweatpants most days. Who forgets to lift the toilet seat sometimes. Who takes off dirty clothes and drops them on the floor.
But that boy of mine lights up my heart. His smile is spectacular. His giggle is infectious. He recently decided to grow his hair from the crewcut he’s had since he was a toddler. He’s a big kid, dwarfing most in his grade. His heart and his mind are just as large. I hope he knows just how much we love him, and how proud we are of him. Someday he’ll read this and hear it again. The words I say to him often will be here for him to read whenever he wants.
Happy 11th birthday, Colin. I love you and am so proud of who you are. You are smart and funny and caring and loving. You are a fabulous big brother to Tristan, an adoring younger brother to Paige, and an integral part of this family. Your “sidling” hugs make me laugh every time. You cheer me with your guitar-playing and I love to watch you play tennis. Math is your favorite subject and you have your father’s easygoing disposition. I just adore you. I can’t wait to see what you are going to do with your charming self when you grow up. You make my heart soar.
You made quite an entrance into this world. I hope you similarly make the world take notice as you grow.






























 Link to Twitter
Link to Twitter