March 7th, 2013 §
 Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).
Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).
I have always had two oncologists’ input on my treatment since my original diagnosis of stage II breast cancer in December of 2006. Even through the more than five years of remission, I continued meeting with them about my adjuvant therapy.
Immediately after I was diagnosed in October with stage IV my oncologists began talking about finding a balance between length of life and quality of life. These two aspects of my life would have to be constantly juggled. The art of medicine and its role in treating cancer suddenly has become crystal clear while the science of decision-making often remains blurred.
For many people it is often reassuring to hear there is a plan, a prescribed protocol. There is a type of comfort in being diagnosed with a disease and being told there are defined steps you need to take. With metastatic cancer it’s not crystal clear. Patients must often help decide what is right for them.
I was offered options about which treatment to try first: a traditional chemo or an anti-hormonal combination. One would attack cancer cells, but also attack the healthy cells in my body. The other would aim to “starve” the cancer of some of its fuel (hormones). One important positive feature about my cancer is that there are choices about how to try to keep it in check. This hopefully will equate to having stable disease for a while so I can live longer. Some types of cancer do not respond to certain therapies and therefore there are fewer options in treating them.
When I went to see my medical oncologist at Sloan Kettering, this week she pulled the chair over and sat only inches from me. I was on the exam table, in the modest red and peach Seersucker bathrobe Sloan uses for their exam gowns. We sat and talked about research and trials and side effects and my blog and my family. She gets emotional sometimes when we talk about the current situation. So do I.
Then Dr. Chau Dang said something that I will always remember. She said that many doctors start to distance themselves from their patients as the patients get sicker and closer to death. She said this is their coping mechanism. Of course I couldn’t help but wonder if the same process is what is behind some of my friends disappearing and rarely contacting me anymore. Some physicians, she said, seem to back away, needing emotional distance not to be weakened each and every time a patient dies.
In contrast, my doctor feels this is precisely the time in her relationship with her patients to embrace them, bring them close, provide them care and comfort as much as possible. It’s important to remember, she always says, that this isn’t a case, this is a life. A person with friends and families who love them. Death happens for all of us. It’s her role to do what she can to prolong life, and when that can’t be done anymore, it’s important to still care for the person, not just treat the disease.
The nature of the doctor-patient relationship changes over the course of illness. Perhaps nowhere is that truer than in oncology. I’ve always been a partner in my care, it’s the only way I know how to be. It’s my life, after all, and the decisions we make as a team are ones I do not want to regret because I gave up control or didn’t have adequate information. However, I also accept that treating cancer is not an exact science.
Some patients do not want to have options. They want their physician to pick the course of treatment that seems best matched for the patient and proceed. A patient sometimes doesn’t want choices; he or she wants the doctor to do the sifting and prescribing. This works for many people, and takes the responsibility off the patient. There is mental comfort in that approach, too. I can understand why some people make that choice.
One of the things that is difficult in being a true participant in your own care is that while you get the satisfaction of partial control, you also must accept responsibility if/when things go wrong. This is part of the deal.
Some things just are.
Some things just happen, even when you do all you can.
I have accepted this jagged truth all along.
But I think some people never do.
March 4th, 2013 §
 Once or twice a week I awaken in the middle of the night with a poem in my head. I reach for my phone and I type frantically. I go back in the morning, or after a few days, and read what I’ve written. I know the words are important, streaming from my head like water breaking through a dam. This poem came from one of these middle-of-the-night sessions.
Once or twice a week I awaken in the middle of the night with a poem in my head. I reach for my phone and I type frantically. I go back in the morning, or after a few days, and read what I’ve written. I know the words are important, streaming from my head like water breaking through a dam. This poem came from one of these middle-of-the-night sessions.
If you let me
If you let me
I’ll cry you a river
Scream at the moon
Hold your hand
Kiss your mouth
Feel your heartbeat
Dream of more
Fear the end
Wish it were different
Pound my fists
Swear a blue streak.
If you let me
I’ll give you strength
Find a reason
Deliver some hope
Take a needle
Feel the pain.
If you let me
I’ll be grateful
Feign bravery
Take a stand
Do my best.
In the end
I’ll whimper softly
Try again
Give a last kiss
Take a last breath
Slip away.
February 21st, 2013 §
 “I look so old in that picture.”
“I look so old in that picture.”
I hear this one a lot now that my friends and I are what they term “middle-aged.” They want to see and choose pictures before they get saved or shared; the confidence and carefree attitude in photos from our youth has slipped away.
It’s not just people my age, though. For example, my father in his 70s comments on how old he appears in photos I take, too. With a full head of white-gray hair, he doesn’t look old, I think… but even if he does? What’s wrong with looking his age? With plastic surgery and Hollywood showing altered appearances all the time it’s almost shocking when we see people who haven’t adjusted their appearance. Maggie Smith (most recently of Downton Abbey fame) has a face as wrinkled as a Shar-Pei, and we love her for it.
Aging isn’t easy. There are cruel sides: bodies that hurt, diseases like Alzheimer’s that strike mercilessly, loss of independence and body control. For sure, I don’t mean to imply that getting old is pleasant.
Aging is, however, the price one pays for living.
I look at getting old as a positive now. To age means to be alive. For some of us getting old is now a pipe dream. I will miss an entire generation of my life. That is the truth about my stage IV breast cancer.
I face the reality that I am not middle aged. I am living my own old age now, in my 40s.
February 11th, 2013 §
The finish line is the goal.
Runners strap on shoes, push their bodies, train for months.
Do it well. Do it faster. Faster than the others.
Laps around the track, tires squealing, pit stops along the way.
Checkerboad flags, shake the champagne.
Biking stages, climb the hills, pass the others, wear the gold jersey.
You got there first.
You won.
But I do not want the finish line.
I do not want to get there first.
I am dragging my feet.
Digging in my heels.
Fingertips grasping,
Losing touch,
Don’t make me go.
I’m fighting, crawling, resisting, doing everything I can.
Make the time slow down,
Make the days longer,
Make the end out of my sight.
I don’t want to be the first to the finish line.
I want to be last.
This time, losing would be winning.
January 31st, 2013 §
I always think these updates must be boring to read. I know they’re necessary, and important. I know this is how most of you get the nitty gritty details on my treatment. Somehow, though, I always wonder if they are actually educational or if they are too technical. So, that’s why I try to limit them to about once a week or when there are changes. My goal is to show you how these decisions get made (in my case only). Some cancers have very specific and formulaic treatment schedules. Metastatic disease often does not. It’s unclear which drug(s) will work and for how long. It’s never known how a patient will tolerate the drug initially and cumulatively as time goes on. The patient has a lot of leeway in many of these cases. There is no blueprint. A good team has communication about options and constantly revises their strategy.
I had this week “off” from chemo. The last few days I’ve felt very good. I have been spending lots of time with our new dog, Lucy, who has brought joy into our home in so many ways. We just adore her.
I was at Sloan Kettering last week and today I met with my local oncologist. Fortunately everyone in agreement after a review of all of the options. One of the things that’s always a concern is quality of life. My doctors are very keen on making sure I am comfortable and able to do things I enjoy. The balancing act of aggressive treatment to extend life without sacrificing too much quality of life is an integral part of treating metastatic cancer. There is no cure. But the goal is holding off the inevitable as long as possible.
I’ve had lingering trouble with the monthly IV bone drug Zometa. Some readers suggested I ask about the other available drug Xgeva, a subcutaneous injection also given once a month. They anecdotally reported fewer side effects. Both of my doctors do not believe Xgeva actually is better for my needs cancer-wise than Zometa, but also agree it’s not worse. One option was to try an IV steroid infusion of Decadron immediately prior to the Zometa to see if it helped with side effects. The other option was to try to the Xgeva and see if I had any side effects from that (most people report fewer to no problems with it, though most also do not have problems with Zometa after the first one or two times). I’ve opted to try the Xgeva. I would usually have gotten it today (28 day interval) but I have plans this weekend that are very important to me. I don’t want to risk being ill and having to cancel. It will not be a problem to get the injection on Monday, so I will postpone it for a few days. We’ll see how I tolerate the Xgeva shot and go from there.
My tumor marker number stayed relatively constant after that small increase two weeks ago. This is good, but leaves us in a bit of a quandary. We aren’t yet at the point of doing a repeat PET scan. The rise is not enough to warrant that, though we will do it soon. Neither is the increase enough to assume the chemo has stopped working after initially being responsive. We don’t know, as I said in the last update, if it’s an anomaly or a trend. The only things that can show us are more data points. I happen to like data points. I like seeing what happens every 2 weeks even if it means more of an emotional rollercoaster. We are only 4 months into this and I don’t feel that we have a handle on how I’m responding yet. Only time can shed light on that. I did have a good initial reaction to the drug which was encouraging.
So… since we’ve achieved a good decrease in the last 4 months with the Xeloda but now that is slowing down and I seem to have “bottomed out” on its efficacy, what now? We want to keep everything where it is. If we can get more of a decrease, that’s the best. If not, we need it to hold steady. We all agree it’s time to try again to increase the chemotherapy dose and see if I can both tolerate it and get a stronger marker response. I started at 8 pills a day in the beginning (for about 2 months) and had to decrease about two months ago to 7 pills a day when side effects became intolerable.
It’s time to walk into the fire again. There is no manual for how to do this. We all brainstorm, we talk about what my goals are, we talk about what makes scientific sense. The idea this time is to increase, but not go back to the 8 pills for the whole round. Instead, to try to get more chemo in my system, I will alternate 7 and 8 pills for the week. We’ll see how I do. Debilitating nausea, stomach pain, hand/foot syndrome, and migraines have been my issues with this drug in the last month.
Also, I will change my start day. Thursday night was my usual. Lately, however, I’ve felt rotten on the weekends (both weekends this time around, as effects often last into day 10 or 11 which technically are “off” days for me). I will now start chemo on Saturday night or Sunday morning and see if we can shift my “rotten days” to weekdays instead. I want more quality days with my family on weekends if I can get it.
This is all educated guesswork, a constant dance of drugs and schedules and side effects and efficacy.
There is no manual.
There is no “must.”
There is only me, floating away, trying to grasp the fingertips of treatment and hope.
January 19th, 2013 §
I wrote this back in 2010. Just like in this week’s “I think so too” I decided to think about the history of an object.
………………………………..
I took my friend Brenda out to lunch for her birthday today. While we were sharing an appetizer, a group of four people entered the restaurant: three men dressed in business attire accompanied a woman with a knit cap on. I realized in an instant she was bald underneath that covering and postulated that the hat would not be coming off.
They took off their coats and sat down at the table. I watched them for a while, from a distance, across the restaurant. Indeed, the hat did not come off. She was bald, most certainly, and likely undergoing chemotherapy. My mind started to wander, and I started to wonder. Was she at a business lunch and able to keep working during this crisis? Was she done with treatment and waiting for her hair to grow back in or was she on an “off week” of chemo when food might be somewhat appealing?
I kept looking at her hat. It was freezing cold out today, so it wasn’t particularly out of place. But I kept staring at it. It looked handknit. Had someone she knew made it for her? Had she gotten it from the basket at the cancer center where people knit and donate hats for patients?
I wonder what she’ll do with the hat when her hair grows back in: will she throw it away? Burn it? Give it to someone else who needs it? After wearing those head coverings day after day, you don’t want to lay eyes on them again. After my hair grew back, I saved my scarves for a friend’s sister who was set to start chemo shortly after I finished. I recently saw pictures of her wearing them. It’s odd to see them, associated with so many memories for me, on her head too. Now I have the scarves back, and some have already been lent to another member of the club.
My wig, worn twice, is packed away in the basement. I will soon donate it to a charity that provides wigs to women who can’t afford them. I hate that wig. I hate what it looks like. I hate how it feels. I hate how I looked in it. Twice I wore it, and I had to keep from tearing it off every second it was on my head. It wasn’t me; I felt like someone else in it. But I just can’t get rid of it yet. It’s like a trophy for walking through the fire.
I wonder if that woman I saw at lunch today feels like that. She and her group finished their meals and left before I did. I was really sorry I didn’t get to tell her that her hat looked great on her.
January 17th, 2013 §
** please note I updated this post in October 2013. I added the following information:
Once again Facebook games about breast cancer are making the rounds now that it is October. I posted this last year and got some flack from people who thought anything that “raised awareness” about breast cancer was good and couldn’t understand why I am critical of these messages.
My point is that this isn’t awareness.
There probably isn’t anyone on Facebook who doesn’t know that breast cancer exists. But there certainly is a lot of myth-busting to be done. This is not how to do it. Topics that do need attention include male breast cancer, the underfunding of metastatic research (30% of people with breast cancer will eventually have metastases yet less than 5% of breast cancer funding overall goes to metastatic research), the fact that for many breast cancers 5 years in remission does not mean you’re free from risk of recurrence, not all breast cancer presents with a lump so self exams and/or mammograms may not always find certain types of breast cancer (inflammatory breast cancer)… the list goes on and on.
There’s a lot of work to be done educating. Education is awareness, these Facebook posts are not.
A friend asked me, “What can I do to help? I can’t donate money to your research fund but would like some ideas on things I could do instead.” What a great question. Rather than post these messages on your Facebook page here are a few easy ideas:
1. Make sure you are properly vaccinated from vaccine-preventable illnesses. This includes your family (kids and your parents if applicable), friends, and anyone else you can get involved (nag). Boosters like those for pertussis are very important. Get your annual flu shot. People over the age of 65 and some others at high risk should also talk to doctors about the pneumonia vaccine.
2. If eligible, donate blood and platelets. These products are needed by cancer patients constantly.
3. If eligible, get tested to be a bone marrow donor. Go to BeTheMatch.com to see the requirements. The initial registry just requires a cheek swab. It’s easy as can be.
4. Read blogs/follow tweets by people living with cancer. I think understanding the day to day lives of those of us living with it is a great way to truly become more aware. It’s one of the reasons I spend so much time writing here. I try to bring you the science, the experience, the thoughts of a mother trying to cope with raising a family and managing an terminal diagnosis.
If you want to see the comments on the new post you can go here. The original post appears below:
………………………….
I don’t usually rant, but something has me steaming. Today the following exact message appeared in my Facebook inbox:
So here is the time of year again when we try to raise awareness for breast cancer through a game. It’s very easy and I would like all of you to participate. Two years ago we had to write the color of our underwear on our wall. Men wondered for days at what was going on with random colors on our walls. This year we make references to your love life status. Do not answer to this message just post the corresponding word on your wall AND send this message privately to all the girls in your contact list!!!!!! BLUEBERRY = single; PINEAPPLE = it’s complicated; RASPBERRY = I can’t / don’t want to commit; APPLE= engaged; CHERRY= in a relationship; BANANA=married; AVOCADO= I’m the better half; STRAWBERRY= can’t find Mr. Right; LEMON = want to be single RAISIN = want to get married to my partner. Last time the underwear game was mentioned on tv, let’s see if we get there with this one !!!!!Copy and paste this message into a new one and send to all your girly friends and update your status with your answer. DO NOT RESPOND TO THIS CONVO, just leave and participate.
I’m going to keep my reaction short. I’m hoping writing something down like this will allow people who are as infuriated as I am with these silly requests to have something to react with.
First, I give you permission to ignore this crap. Better yet, write back to the people who have shared it. Let’s do some real awareness here.
The above instructions are not awareness. This is offensive. Breast cancer is not a joke, awareness does not come from sharing the color of your underwear or your marital status (the whole “tee-hee, wink-wink” attitude adds to my disgust). Even if it ended up on TV, that still would not be educating people about breast cancer they didn’t know before. All it does is show the world that lots of people are willing to post silly things as their status updates.
Let’s do a piece of education right here. The status update says “only send this to your girly friends.” Um, hello… men get breast cancer too. Men are also the husbands, fathers, sons, brothers, and some of the friends, coworkers, nurses, and doctors who care for and are left grieving for people (men and women) who die of breast cancer. We should not exclude them from ANY discussion of cancer.
Just because it says it’s about “breast cancer awareness” doesn’t mean you have to agree. Go ahead. Ignore it. Or write back and tell them why you don’t want to be included in these things anymore. Another blogger, Susan Niebur, wrote about her take here. She was an astrophysicist, by the way. She died of metastatic breast cancer.
Anyone who has breast cancer and uses your FB status update as an indicator of whether you support their cause is not very enlightened. When I rank “how to help those of us with cancer,” sharing one of these paragraphs as a status update is the lowest possible method of showing support. There are endless ways to do that. I think it actually is the opposite; sharing these status updates makes people feel they are doing something real for breast cancer causes when they aren’t.
I’ve also had it with the “I’ll bet most of my friends won’t share this post” attempt to guilt me in to sharing something like “share this if you think domestic abuse is awful.” “Share this if you think autistic kids are special.” Well yes, actually, I believe both of those things. And just because I didn’t share them as my status update doesn’t mean I do NOT agree with the statements.
Education underlies awareness. To even call something a “game” and honestly believe it’s doing anything to help any aspect of this disease is delusional.
I also think that those of us who have had breast cancer have an obligation to speak out if we disagree with these posts. People look to us to see how we react. If we not only read these updates but share them, it does constitute endorsement. It says we agree. It says it’s okay to think of breast cancer awareness this way.
I say: count me out of these Facebook games.
I have stage 4 breast cancer and it is no game to me.
January 17th, 2013 §
There is comfort in routine. Some people are superstitious. Sometimes they want the same chemo nurse, the same appointment time, the same chair. “If it’s working don’t mess with it” applies to many things about treating cancer.
I’m always thinking about continuity and the stories that objects tell. I’ve written twice about the tape measure my plastic surgeon used to measure me before surgery. I’ll post those pieces again this month. Whenever I sit in a chair in a doctor’s office I think about all of the people who have sat in it before me.
Each person has a story. So, too, does each chair. Here is one from 2011.
……………………………
Back in 2011 my plastic/reconstructive surgeon asked, “Did you know it’s been four years since your reconstruction surgery?”
Immediately he chuckled, “Of course you know that,” he said, realizing my mental calendar was certainly more precise than his– of course I marked the days off in my head.
Whenever I sit in a waiting room I am instantly transported to that place and time. I sit and watch patients walking in and walking out. I can tell by hearing what the time interval until their next appointment what stage of treatment they are in.
I sit in the chair, the same one I did four years ago.
It’s the same chair, but I am not the same person.
My body is not the same.
There is continuity in that chair.
There is a story it tells me.
I wrote this piece to the next person who sits in that chair.
………………………….
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. PET scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments. Tears. Avoidance.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Asking the grocery line folks to “make the bags light, please.” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
Targeted treatments. Effective treatments.
Ultimately, someday, perhaps: a cure.
Don’t you think that would be amazing?
I think so too.
January 13th, 2013 §
Originally written on January 30, 2009 (the two year anniversary of my surgery).
……………………………..
I had two surgeons that day:
one just wasn’t enough for the job.
The surgical oncologist would take away,
the reconstructive surgeon would begin to put back.
Before I headed off into my slumber,
I stood as one marked me with purple marker.
He drew,
he checked,
he measured.
And then a laugh,
always a laugh to break the tension:
Surgeons must initial the body part to be removed to ensure
they remove the correct one.
But what if you are removing both?
How silly to sign twice,
we agreed.
And yet he did,
initialing my breasts with his unwelcome autograph.
The edges of the yellow fabric measuring tape he used
had purple fingerprints up and down their sides;
use after use had changed their hue.
And now it was my turn to go under the knife –
a few more purple prints on the tape.
I got marked many a time by him that year.
Endless rounds of
purple dots,
dashes,
and lines
punctuating my body
with their strange, secret blueprint
only those wearing blue understood.
We stood in front of mirrors
making decisions in tandem
as to how my body should and would take new shape.
Two years today and counting.
Moving forward.
Sometimes crawling,
sometimes marching,
and sometimes just stopping to rest
and take note of my location.
Numb inside and out,
but determined.
Grateful,
hopeful,
often melancholy.
Here comes another year
to put more distance
between
it and me.
Let’s go.
January 12th, 2013 §
Now that my cancer is stage IV many things that once seemed important are now at the bottom of my list. I distinctly remember during and after my breast reconstruction that I was very obsessed with every tiny detail about my implants. What size should they be? Were they healing well? Were they even? How did they compare to other women’s reconstructed breasts?
I think after I finished chemo I needed something to focus on. It seemed that this was something positive. Something for me. Something that would make me feel better (after all, those tissue expanders before the implants were the pits).
The time between when I was diagnosed and when I had my double mastectomy was about one month. Those were anxiety-filled weeks. Though I consoled myself with the news that my cancer was confined and surgery would most likely be enough to treat it, later I learned after the mastectomies that my cancer was actually stage II.
I look now at this piece I wrote and I can still connect to it. I still remember what it felt like. But now that I’ve got metastatic cancer I don’t give a damn about how my implants look. None of that matters to me. One of my first phone calls after the new stage IV diagnosis was to my plastic surgeon to ask if there was any reason to consider removing them if it would help any of my treatments that are to come (there isn’t).
This piece was written about my first diagnosis and surgery… when it was all very new. It seems so long ago. A lifetime. It’s been six years.
……………………………………
In the weeks before my surgery, I looked at pictures of double mastectomy patients on the Internet. I Googled “bilateral mastectomy images before and after” thinking I was doing research. I thought I was preparing myself for what was coming.
In reality I was trying to scare myself. I wanted to see if I could handle the worst; if I could, I would be ready. My reaction to those images would be my litmus test.
Some of the pictures were horrific. I sat transfixed. I looked. I sobbed. I saw scarred, bizarre, transformed bodies and couldn’t believe that was going to be my body.
Days later, when I met my surgeon for my pre-op appointment for the first time he said, “From now on, don’t look at pictures on the Internet. If you want to see before and after pictures, ask me: look at ones in my office. You can’t look at random pictures and think that’s necessarily what you are going to look like.”
All I could do was duck my head in an admission of guilt. How did he know what I’d done?
I realized how he knew: other women must do this. Other women must have made this mistake.
The aftermath is terrible to me though not in the ways I’d anticipated. I have no sensation in my chest. I never will.
A major erogenous zone has been completely taken away from me. Yes, I have new nipples constructed, but they have no feeling in them; they are completely cosmetic. The entire reconstruction looks great but I can’t feel any of it. It does help me psychologically beyond measure to have had these procedures though.
Here I sit, two gel-filled silicone shells inside my body simulating the biologically feminine body parts I should have. And sometimes that thought is disturbing.
To be clear: I don’t regret having them put in. I’ve never regretted that. It was a decision I made, and made deliberately. I knew that reconstructing my breasts was the right decision for me. I am overwhelmingly happy with the cosmetic appearance and the wonderful job my talented surgeon did. I will always be grateful to him for what he’s done.
I definitely don’t remember what my breasts looked like before. I only remember these.
I once asked my plastic surgeon to see my “before” pictures a year or two after my reconstruction was over. You know what? My “before” breasts didn’t look so great.
In my mind they did though.
In my mind, everything about my life before cancer was better.
But that’s not the truth.
Don’t take that as an endorsement of the “cancer is a gift” nonsense though.
My mind distorts the memory of my body before cancer. Then forgets it.
My mind distorts the memory of my life before cancer. Then forgets it.
With time, I can get used to a new self.
It’s like catching my reflection in the mirror: only lately do I recognize the person staring back at me.
For over a year the new hair threw me. It’s darker than I remember it being before it fell out. It’s shorter than it was before, too.
And the look in my eyes? That’s different also.
I just don’t recognize myself some days.
Sounds like a cliché if you haven’t lived it.
But it’s true.
January 9th, 2013 §
Elizabeth Edwards reached many people because she was in the public eye, but inspirational people also live quiet lives. We can be inspired by Edwards’s grace and courage as she dealt with the challenging parts of her life in the same way we can find inspirational people around us each and every day. These are all people we can connect with and learn from. In doing so, we better ourselves.
When she was diagnosed with metastatic cancer people told me not to worry: it wouldn’t happen to me just because it happened to her. That’s true. It wouldn’t happen just because it happened to her. But it did happen. And now I look back on everything I’ve said for the past 5.5 years and I am glad I expressed those thoughts as they were happening. Because my fear came true.
…………………………………..
(from December 7, 2010).
I didn’t know Elizabeth Edwards. In fact, I wrote a piece critical of her when she initially stood by John after his affair. I was disappointed when she gave an interview on CNN in May of 2009 and spoke only of John’s “imperfection” rather than calling him the cheater he was and kicking him to the curb. I was angry she hadn’t used her interview time to talk about herself, her cancer, her life: the topics I wanted to hear about. I was angry at her for not claiming her remaining years of life as her own.
So why am I sitting with tears in my eyes because she has died?
I cry because it makes me feel vulnerable and scared of what this disease can do to me: what it did to her.
Yes, I know… there are plenty of men and women who get cancer, have treatment, and stay in remission for the rest of their lives. And, in essence, isn’t that what every cancer patient hopes for, as Betty Rollins wrote, “to die of something else”?
I don’t think it makes me pessimistic, depressing, or negative to think that I am vulnerable.
It’s the truth. It’s my truth.
Anyone who hasn’t been to the oncologist with me to see my risk-of-recurrence charts, my mortality charts, my decision-making discussions along the way can’t say to me “Oh, don’t worry, that won’t be you.” No one, including me, knows how it will go.
People tell me: stay strong, just think positive, you can’t generalize from her situation.
I respond: I am strong, I hope for the best. I don’t think positive thinking is going to save me if there are remaining cancer cells still in me.
I hope that people won’t say to someone who has been diagnosed with cancer, “Don’t worry, what happened to Elizabeth Edwards won’t happen to you.” Because while we do everything we can to ensure we die of something else, it just isn’t always the case. In 2006 her oncologist told her that there were many things going on in her life, “but cancer was not one of them.” Things change quickly, cancer can recur when you least expect it.
I have sympathy for her family. I cry for her children. I am saddened about the years she spent with a man who didn’t deserve her. I am angry about the time she wasted on him. I hoped she would be an example of someone who would keep cancer at bay.
I grieve for that hope, now gone.
December 20th, 2012 §
Today marks the six year anniversary of the day I was first told I had breast cancer. When the radiologist told me the news, she also said she didn’t know exactly what it was or how bad it was.
This is why you do not schedule mammograms or biopsies right before a holiday. Especially Christmas. You’ll be going on vacation… and if you aren’t going on vacation, the doctors, nurses, and pathologists will.
I was told on December 20, 2006 that I almost certainly had cancer based on the mammogram and ultrasound images. I’d need a biopsy to confirm it. But they couldn’t do the biopsy until after the new year. It’s hard to hear, “We think you have cancer. Now go on your vacation and when you come back we’ll figure it all out.” Weeks later I was told I had extensive DCIS and would need to have my left breast removed. I opted to have a double mastectomy. A few weeks later a second look at the slides revealed I had some breast cancer in one of the lymph nodes that had been removed (I am now a big advocate for a second opinion on pathology). I was reclassified as having stage II breast cancer. I had chemotherapy; later, a salpingo-oophorectomy.
Almost six years later, I have now found out that I have stage IV (metastatic) breast cancer (details here).
Yesterday I went to an appointment with my local oncologist. I go to see him every two weeks right now to review bloodwork and to discuss dosing for the next round of chemotherapy which starts tonight.
The concept of “good news” has been completely redefined since my new diagnosis. There is no cure, so I can’t hope for that. There is never going to be a day I am not aware of running out of time. Now “good news” gets defined as stable disease. If you’re lucky, and the chemo is working, good news can even mean reduced disease. Now I hope for that.
I look at my oncologist’s face when he walks in the room. I scan it for signs of what kind of news day this will be. The day he told me about my metastasis I read his face. When he walked in that day I asked him how he was and he said, “Not good.” I assumed it was something about him, his family. I immediately starting worrying about the bad news he was going to tell me about someone else. But it was my bad news. It was my nightmare.
I never used the word cured. I never said it. And I don’t like when others do with my kind of cancer. I always prefer the technical terms NED (no evidence of disease) which means it may be there, but we can’t detect it with the tests we have done. I don’t even like the term “cancer-free” for my particular cancer… again, there might be cancer there, but just not enough to be detected or can’t be with the tools used.
Five years had come and came and gone. Even nurses in other specialties would say at my checkups, “Oh! Five years! That means you’re cured!” and when I’d explain to them that it actually didn’t mean that at all with my kind of breast cancer they would look at me quizzically.
“SEE?! I told you!” I want to go back to say to all of them. I was vigilant for a reason. It “shouldn’t” have happened based on the statistics, the predictions. But it did. And now the only life I’ve got is spent dealing with it.
……………..
I watched my oncologist’s face yesterday. We’ve had some bloodwork results in the last two months that have been a good first step but he hasn’t been willing to budge much on declaring that this chemo is working. One or two data points are not enough for either of us to feel confident, actually. But yesterday we got our fifth data point.
I still have metastatic cancer. That isn’t going to change.
But I have some news I can finally share: my bloodwork is showing “indisputably” (in the words of my doctor) that my cancer is shrinking. The chemo is working. The pills I’ve been swallowing, seven or eight a day for seven straight days at a time, in alternate weeks, are doing what we’d hoped. The cancer is still there. But it’s smaller. But it’s responding. It’s been consistently trending down since I started on Xeloda. Now, with more than a few data points, we can finally characterize the effect and I can share it publicly.
……………………….
So what does that mean? I know that’s the question most will ask. It simply means this is the chemo I stay on for now. It means that I just keep doing what I am doing. I’m not “cured” or “feeling better” or “cancer-free.”
It means that modern science and pharmaceuticals are giving me some time. For today, the cancer is responding, shrinking. And in the land of stage IV cancer, that’s unmitigated good news. Make no mistake, it’s no Christmas miracle. It’s not happening for any other reason than the fact that I am aggressively taking as strong a dose of this drug as I can tolerate, and it’s doing its thing.
Six years ago I went on Christmas vacation and feared for my life. I was scared and confused and miserable. Now, six years later I’m in a much worse place vis-a-vis cancer but my mindset is different.
I’m coming to terms with accepting the life I have — the one I thought I’d have is gone. I have created a new one. The best one I can.
For today, I celebrate the good news. I will go to my children’s school holiday parties. I will smile. I will make memories. I will not focus on side effects. I will find beauty in something small.
I will savor the things I can do today.
December 12th, 2012 §
Tuesday’s visit with my oncologist at Sloan Kettering was informative, as always. However, the big question can’t be answered: what is the trajectory of my stage IV cancer?
There will be no answer to that for now.
We start with a chemo. We see (through bloodwork and PET scans) how the cancer responds. If it responds, I stay the course until the treatment stops working or the side effects become untenable or dangerous. There is no way to know how long that will be. Any particular chemo could be ineffective from the get-go. It could fail after months. It could fail after years. Then you go to the list of options and decide on a next chemo regimen. This decision is not always easy; you can’t know which one will be best for you. It is often educated guesswork at best. There can be many chemotherapy options and in the end, I will probably try many/all as each one eventually fails. I’ve talked to women who have gone through more than eight different chemos in the treatment of their metastases. One thing I know is that chemotherapy in one form or another will be a part of my life for the rest of my life.
There is also no way to know if you will tolerate a chemo regimen well. Side effects can be dangerous and variable. Sometimes side effects are serious enough that you must discontinue using a particular drug even if it’s effective in reducing the cancer. As you can imagine, this can be a heartbreaking proposition: find something that works but you are unable to take.
As you know from my last post I have been struggling with HFS (Hand/Foot Syndrome) from the current chemo, Xeloda. I had done some research and found some studies indicating that the selective COX-2 inhibitor and anti-inflammatory drug Celebrex has been used with some success in helping reduce the severity of HFS in patients taking Xeloda (and a few other specific chemos). I had reduced my daily dose of chemo from 4000 mg to 3500 mg for this 5th round (7 days on, 7 days off) to see if the HFS improved with a slightly lower dose. Of course it’s scary to reduce the dose of your chemo but I’ve tolerated the maximum dose for a good number of rounds. It’s normal to need to reduce the dose as time goes on.
My oncologist agreed that the Celebrex was a good thought and definitely might help the HFS. There are risk factors associated with the use of the drug but we both agree that it’s worth the small risk. So I am starting with 200 mg once a day to see how I tolerate the Celebrex and if a low dose helps I will stay with that. If needed, it can be increased to 200 mg twice a day. My hope is that the Celebrex helps the HFS and allows me to go back to the higher 4000 mg (8 pills) a day chemo dosing for the next round.
In the meantime I continue with frequent moisturizing of my hands and feet (at least 10 times a day) with a variety of lotions including shea butter, Eucerin, Aquaphor, and more. I stay away from water, do not apply heat on hands/feet, wear socks and soft shoes/slippers, and wear gloves as much as possible. My feet have been doing very well, my hands holding steady and actually do seem improved today. Here’s hoping!
I know this was a technical discussion today but I want to share it for other people in treatment who might be able to ask their doctors about Celebrex if they suffer from HFS with Xeloda. I also hope that the explanation of chemo and prognosis will be informative.
I continue to do as much as I can everyday and when people see me and say, “You’d never know what you’re going through right now,” I take it as a compliment. I was busy today with routine dentist and endocrinology appointments… you can’t ignore the rest of your body when you are treating cancer. Many other body systems will be affected by the cancer and chemo. My thyroid has been holding steady but shows signs of needing another medication adjustment. Bone treatments like the Zometa infusion I take can cause problems with jaw bones. It’s important to keep a watchful eye on your whole body and not use cancer as an excuse for ignoring routine checkups. That’s my loving nag for the day… stay vigilant with your healthcare appointments and thanks for all of your support.
December 8th, 2012 §
I realized it’s time for an update… but confess I’ve started and stopped this one a few times. Somehow when things are going along somewhat easily it’s easy to do the updates.This is the first one I’ve had to discuss side effects and I hesitated a lot about what to write and whether to post it. I wasn’t sure about talking about these things lest they be seen as complaining. My goal has always been to educate and inform above all.
Friends on Twitter assured me that talking about the daily in and out of chemo treatment for metastatic cancer is important. Not only are they learning what it’s like, but it tells people what I’m dealing with and what activities might be hard for me on a daily basis. One Twitter follower also said that for those who have family members with this disease and might not be forthcoming with detailed information, some of these updates give them an idea of what it might be like for their loved ones. While treatments and surgeries vary so much, I thought this was an excellent point.
I also have decided to post this information because I know other metastatic patients will find it through search engines and maybe it will help them. So… I’ve opted to continue to share these things. It’s the reality of cancer. It’s the reality of MY cancer.
I’m struggling at the moment with Palmar/Plantar Erythrodysesthesia or Hand/Foot Syndrome (HFS). This is a common side effect of Xeloda, the chemo I am currently taking. In short, the capillaries in the hands and feet rupture and the chemotherapy spills into the extremities. Redness, swelling, burning, peeling, tenderness, numbness and tingling can accompany it. While it does not always start right away, once you’ve had a few rounds it’s likely to be a cumulative effect.
After receiving another monthly IV infusion of Zometa to strengthen my bones on Tuesday, I started a new round (#5 for those of you keeping track at home) on Thursday night, and had to decrease my dose slightly to deal with the HFS. Rather than 8 pills a day (4000 mg) I’m on 7 now. The hope is that the HFS will stay at its current level and not progress on this dose. This is what feet start to look like with HFS:

It can get much worse than this with blisters and ulcerations but mine is not at that stage. If it were to reach that point we’d have to stop chemo until it healed and then re-introduce it. Driving was one of the hardest things yesterday, the pressure from the steering wheel (or anything against my hands) was difficult to tolerate. I wear cushiony gloves most of the day now and follow all of the guidelines to keep it at a minimum. My hands are more sore and sensitive than my feet this week but not as red as my feet. Thankfully while I could not hold a pen during most of the day, I could still do some typing. A long-term side effect of this particular drug is the potential to lose your fingerprints. I see an episode of CSI coming on that one! An article about the difficulty traveling with such a condition appears here.
Loss of appetite continues to be an issue but my weight has stabilized after a 20 pound loss in the first 6 weeks. It’s weight I needed to take off anyway, actually. I must eat twice a day when I take chemo and once I start eating I usually do just fine. I do better eating in the evening. My blood counts remained fine even during the weight loss and my instructions have been to “keep doing what I’m doing.” The one thing I can’t do is exercise at the moment. Friction on my feet can exacerbate the HFS so for now it’s not happening. A soon as the rib in my shoulder heals I will be trying to get back to Pilates class.
I’ll be back at Sloan Kettering on Tuesday, 12/11 to meet with my oncologist. We’ll evaluate the HFS by then and talk about ways to help me deal with it and make me more comfortable. We will also then be talking about what dose I will take for my next round and also start talking about when my next PET scan will be.
That’s the update for now, I’m still doing everything I can and am out and about as much as possible. I still bring the kids to the bus in the morning and try to do errands like the grocery shopping as often as I can. I ask for help with things that really are tough on my hands like stuffing the holiday cards or doing laundry or dishes. Even small tasks give me a sense of accomplishment and normalcy so while the weather holds I continue to do them. Once ice and snow set in and my concerns about slips and falls and bone breakage rise I will get help with more of the outdoor things.
I’ll have more pieces coming out on HuffPo shortly; thank you all for the excitement and congratulations about that new venue. My piece about what to do as soon as you are diagnosed, especially in regard to children, will be the next one they post. After that I’m looking at writing on the topics of bravery/inspiration, the situation when people you barely know take your condition as seriously as if they were family members, and the story of how I found out I had metastatic cancer to begin with. If you have any topics you’d like to see a piece about leave a comment or email me via the contact form and I’ll definitely take it into consideration!
Thanks for all of the support this week.
December 2nd, 2012 §
For those who were asleep in the wee hours yesterday morning and have asked, here is a link to the radio interview I did with Robin Kall yesterday on WHJJ. It’s about 15 min long… to listen click here.
If you are in a radio mood, the post containing the link to the HashHags interview I did a few weeks ago is here.
November 30th, 2012 §
Good news first: I’ve been asked to be a blogger for the new Huffington Post section called Generation Why which focuses on young people and cancer. At first I had to look to my left and right and ask, “Me?” because I haven’t really thought of myself as young in a while. But certainly issues facing people like me with cancer can be unique. The necessary pushes and pulls of being social for my children with the always magnetic desire to just be alone will be one theme I will write about for sure. A friend commented that he was “impressed” I was writing for HuffPo… I will have to remind him that Jenny McCarthy does, too, so it might not be as impressive as he thinks!
That said, I’m very pleased to have a wider audience for my writing. I hope the readers and commenters will be as nice as you all have been. The first post should go up this week and I’ve decided to have them use this week’s post “Alone” as my inaugural piece because the response to that one was overwhelming. I might as well start with a bang! I hope that piece will be one that represents my perspective well.
So.. the bad news is not terrible, but here is the latest news. While I started with very good tolerance to the 4th round of chemo, the end of the round ended up bringing hand/foot syndrome (palmar-plantar erythrodysesthesia) from the Xeloda. Hand/foot syndrome is not the same as neuropathy (though it may include some of those symptoms), which many people on chemotherapy experience.
Hand/foot syndrome is associated with a few particular drugs, Xeloda is one. The capillaries in your hands and feet leak and/or rupture, causing the chemo to spill into the extremities. This causes them to be extremely red, swollen, painful, sensitive to touch, cracked, peeling, and potentially ulcerating. Numbness and tingling also accompany the condition.
For the past month I’ve been trying to keep these effects at bay, but eventually the toxicity builds up. Fine motor activities like tying shoes are hard at the moment, anything that touches/puts pressure on hands and feet. Thankfully I have some shoes with furry insides and cushioning. Socks must be worn 24/7 and slippers at all times. Holding the steering wheel is uncomfortable but doable, thankfully. So many people have suggested I should do something relaxing like go for a massage or manicure/pedicure. Unfortunately between the broken ribs and a “no touching” order for hands and feet these things will have to wait!
I had to skip my last dose (there are 14 in each round right now) of chemo yesterday to prevent a flare. The plan will be to reduce the chemo dose to 3 pills in the morning and 4 at night next round to see if that will be enough of a reduction to stop the progression of the syndrome. If it isn’t, we’ll reduce again. The reduction in dosage is not rare. My understanding is that tolerating 4/4 for 7 days on and 7 days off for more than a few months is pretty unheard of.
I’ll have bloodwork on Monday, December 3rd and then meet with my local oncologist on Tuesday the 4th for a strategy meeting and check on the hands and feet. I’ll also receive my monthly IV of Zometa for my bones at that time.
…………………
Tomorrow (Saturday) sometime between 7-8 AM I’ll be on Robin Kall’s radio show which streams at www.920whjj.com. Stay in your PJs and join us! I think it will be after 7:15 sometime as the 2nd segment.
…………………
Thanks for the continued support and I’ll have a more creative post this weekend.
November 24th, 2012 §
I can see how isolating metastatic cancer can be already.
It has become hard for me to be around other people.
I find myself hiding as much as possible.
When I am in the company of others my mind wanders.
I can’t focus. I feel the need to retreat.
For the time being I just can’t relate to others’ lives which only 6 weeks ago were so similar to my own. Now… we are a world apart.
It’s not their fault. It’s just that circumstances make it so that I am selfish. I try to conserve my energy as much as I can.
Already I can see relationships suffering. There is a fine line between giving space and putting distance. Some are already dropping away, and we’ve only just begun. Others have risen to the occasion and helped more than I could have dreamed. Only true friendships are going to make it under these circumstances. Sometimes the isolation comes from being shut out. Sometimes it comes from locking yourself away.
Phone calls go unanswered, emails often do too. Thank you notes don’t always get written, social commitments get canceled or never scheduled in the first place.
I know that people cannot truly understand.
I don’t want a support group right now because metastatic cancer has a wide range of outcomes. I don’t know if I will be in a rapidly progressing group or not. I don’t know whom to look to that is “like me.” There is no way to know which group I will be in, who my peers are.
Right now I am very sensitive to death, to pain, to suffering. It’s very hard for me to see right now. I’m too raw. I just don’t think I’m ready for a group. But I won’t say I never will be. I need to talk to my oncologists about whether they have patients like me.
It’s difficult to listen to people complain about trivial things, normal things, things I was complaining about two months ago.
Now those complaints just annoy me, or make me sad.
I want to scream, “I want your problems!” And I do. I want that life back. I want to turn back the clock. I just don’t want it to be this right now.
One of the things that bothers me the most about this disease is the knowledge that the way I feel right now is the best I will ever feel for the rest of my life. It’s only going to get worse. That thought terrifies me.
When you feel crappy you want the time to go faster. You just want to get through it.
The problem is that what you may not have is time.
It’s a conundrum. You want the time to pass, but this is the only time you have.
I know so many people say, “No one ever knows how much time they have. You have to make the most of every day, of every moment.” I know that’s true. But the knowledge that there is something identifiable in your body that is a threat, is most likely to be that which kills you, bears a different weight. Of course the doctors don’t know exactly how much time it will be. There is no crystal ball.
Everyone tells me the stories of friends and relatives who were told they only had months and years later they are still alive and doing okay. I am told these stories every single day. I get it. I do. And I love them, they give me hope. But often those people’s diagnoses and particulars bear no relation to mine. Additionally, there are also stories of the people in the other group, the ones who thought they had years and didn’t. People probably have the good sense not to tell me those stories. But they are out there. It’s not that I focus on the negative. It’s not that I necessarily think I will be in that group. But anything is possible. On both sides.
The part that scares me: I’m only at the beginning. I hope that I will get stronger, gain acceptance as I get used to this diagnosis. But I’m not sure about that. I truly believe I could handle this better if I didn’t have so much worry about my children and what effect this will have on them. I wish I could protect them, shield them from this agony.
There are good days and bad days. I must do my best. But being the one everyone is watching takes a toll. Everyone will take their cues from me. I will set the stage for how my friends and family will deal with this: how I handle metastatic cancer matters. I am laying groundwork. I must do it right.
Some days that is an overwhelming task.
“Doing it right” doesn’t mean I have to be positive all the time. Doing it right means I have to be honest. It means I get up each day and do the best I can. For myself, for my husband, for my children, for others who may have cancer and those who will get it. It’s okay to be scared, and angry, and sad, and everything else.
It’s all part of this.
And for me, so is sharing.
November 21st, 2012 §
I load the dishwasher, put in a load of laundry and buy Colin a new white dress shirt
Because I can.
I walk the two blocks between the doctor’s office and the drugstore on a crisp autumn day
Because I can.
I give my children an extra hug, just one more kiss, an additional “I love you” before the bus
Because I can.
But still I worry about today, tomorrow, and the next day.
How can I not?
I put makeup on yesterday.
I can tell it puts people at ease.
If I look “healthy” then they can relax.
If I don’t look sick they won’t have to worry how to act or what to say.
They tell me “You’d never know to look at you. You’d never know you have cancer. You’d never know you’re sick.”
Some moments that’s true. Some moments I feel good. Some days, in fact. And I treasure those.
Some days it’s a lie. It’s not how I feel.
I know it’s a compliment. I take it as such.
The phlebotomist asked me at my oncology appointment yesterday if I’m ready for Thanksgiving.
I wasn’t sure whether to cry or laugh.
Ready?
I don’t know.
Giving thanks. That’s a loaded phrase.
I am grateful I have some time. I am thankful for the kindness that gets shown to me every day by my family and friends.
I appreciate every person who tells me they are lifted by my words, learn from them, say they express something they have felt or even just wondered about.
For every email I get of support,
Every offer of help,
Every playdate,
Every Facebook post, photo, comment
I give thanks.
But cancer sucks. This diagnosis is my nightmare.
But I also know that tragedies happen to people every single day. A life can be lost without warning. I have learned of two sudden deaths of friends’ loved ones this week and I see the pain those losses have caused. I learned it for myself when my mother-in-law died. She did not have time to say her goodbyes.
I don’t like that my life revolves around this disease right now. I try to keep my life focused on others as much as I can. I try to check in on friends who have their own troubles. I try to keep up with the kids. I try to be a good wife and keep the house running. I wish I could be a better wife right now. I try to be strong. I try to suffer on my own time. I try at these things but don’t always accomplish them.
It’s an isolating predicament. Few can know the anguish, the daily trials, all of the parts of my life which don’t get shared with anyone. I share some here, of course, and with friends, but much of it is my own. For now, this is how it needs to be while I continue to process and try to make sense of this new chapter.
Thanks to you all.
…………………….
I was honored to be featured in this blogpost from the American Cancer Society titled “Cancer survivors are truly remarkable people” which focused on the post I wrote in the days after my diagnosis giving tips on how to talk to children about stage IV cancer.
……………………..
Many have asked about the fractures on my left side. The one that is painful is the one in a rib up near my collarbone. That will probably take two months to heal. It is a fracture caused by cancer in that bone. The cancer must shrink first. Only then can the bone heal. So it will be a slow process.
I start round 4 of chemo tomorrow, on Thanksgiving night. Same full strength dose because I was able to tolerate the last round again. Same regimen: 7 days on, 7 days off.
October 19th, 2012 §
I’m doing quite well after first week of chemo. Today is my first full day off and I’ll start up again next Thursday night. I only have a few minutes to update you but I know I’ve been so quiet this week and usually that makes people worry!
I want to say that everywhere I’ve gone for medical appointments this week I have doctors telling me stories of patients of theirs who have been living with metastatic breast cancer in their bones for years (and in some cases, “years and years”). Until proven otherwise, that’s the group I’m putting myself in. Anyone who knows me knows I’m the biggest realist (and skeptic) there is. But right now I’m going full steam ahead and trying to recalibrate my life to this new normal. My body will be doing lots of work and I know I won’t be able to do everything I want to. I’m already accepting help so much more than I ever have. For now I am hoping that it helps others to be able to do something practical and useful for me instead of feeling helpless… since I know feeling helpless is a terrible feeling when watching a friend or loved one go through a difficult time.
I won’t talk about side effects today, I won’t talk about negative stories today. Today is about the stories of women with this disease who are living with cancer. That’s my story.
…………………………
And a few links for you non-Twitter folks who might not have seen:
Author Laura Zigman and her Xtrafrenemy videos make me laugh. She made one for me. You can watch the YouTube video here. I’ve heard of Lisa Adams! (Laura, I miss you… thank you for the gift of laughter).
Also, Media Bistro did a really nice piece this week on me. You can see that here.
October 5th, 2012 §
I loved the book The Age of Miracles by Karen Thompson Walker. I had the pleasure of meeting the author a few months ago. In the book, the earth’s rotation starts to slow. The days stretch longer with obvious consequences on daily life with some not-so-obvious effects on personal lives. I found the book immensely readable, creative, and thought-provoking (My teen daughter thoroughly enjoyed it too. It’s absolutely appropriate for that age group).
My own life has suddenly taken an opposite turn. It feels as if the world has sped up. The days are flying by. There just isn’t enough time.
It’s only been four days since we had an inkling from my oncologist that I had metastatic breast cancer, three days since I have known for sure. And now, in the middle of the night, it’s time I long for. The Earth is spinning so fast… how can it be I’ve been awake for two hours? Have I spent them wisely? What else could I be doing with those days, minutes, seconds?
I’ve done so much already.
I wanted to share a few ideas on things I’ve done already, many of them pertaining to my children. In the dizzying days after a metastatic cancer diagnosis there is so much emotion that it might be hard to think about what to do. You feel helpless. In some ways you are helpless until you get more information. But in the meantime here are some tips about what you can do.
I understand that not all of my readers have children. But for those of us who do, helping children adjust to this news is vital. It not only helps the children but can help relieve some associated stress for the parent.
- Don’t share your news until you know for sure what your particular diagnosis is. I don’t think you need to know your exact treatment; that takes time. But even knowing a general range of what might be used is helpful. If you have had cancer before, children will usually want to know if you will be doing the same thing (especially if it has to do with hair loss) or if it will be different.
- In my case I needed to have a mediastinoscopy with biopsy after my status was confirmed. It’s an outpatient surgery that inserts a camera through an incision in your neck to grab some lymph nodes for biopsy. I decided to focus on that concrete event mostly… it’s something children can wrap their heads around… Mom is going to the hospital (not uncommon in my household), having a small operation, will be back tomorrow night. I explained the cancer, the metastasis, and answered lots of questions, but I think the “one step at a time” was more easily tangible with the surgery as the immediate hurdle. If you will need an overnight stay for your particular surgery I think it’s best not to spring that news on children if possible. An overnight absence is best with a few days’ notice. Children, in my experience, are usually a bit clingy after bad news and that would provide the opportunity for follow-up questions and reassurance.
- Be sure you understand your diagnosis. Explain what words mean to children and to your friends. There are many misunderstandings about cancer and stage IV cancer. The word “terminal” might be scary. Stage IV cancer is not the same diagnosis in different diseases. Prognoses vary and some types of metastatic cancer can be slow-growing or respond well to treatment, allowing years of life.
- I think the phrase “it’s not curable but it is treatable” is important to teach and use.
- Wait to share your news publicly until after you have told your children (except with a few close friends you can trust to keep the information to themselves. This determination may not be as easy as it sounds). This also gives you a day or two to begin adjusting to the news so that when you do discuss it with your children you might have emotions a little more in check.
- As soon as you tell your children, be sure to tell adults who work with your children on a regular basis. If your children have learned the news, by the time they go to school, lessons, and sports, their teachers need to know. Email coaches, teachers, school administration, guidance counselors, school psychologists, and music teachers. Grief in children is complicated and it’s important that all of the adults know and can be on the lookout for odd behavior. Also, they need to be understanding if things don’t seem to be running as smoothly at home or a child seems tired or preoccupied. Two-way communication is key. Adults need to know they have the opportunity to bring any problems they see to your attention easily. Encourage them to do so, whether what they observe is positive or negative.
- Use counselors, especially school psychologists. My first call yesterday morning before I left for surgery was to reach the high school psychologist. Because Paige is in a new school (high school) I didn’t even know which person it would be. Even though it was only 9 in the morning when I called, the psychologist had already received my email (forwarded from the guidance department to the appropriate person) and had a plan in place to find my daughter during 2nd period study hall. She was able to introduce herself, talk to my daughter, and let her know how to get in touch with her as needed. They set up an appointment to meet to talk more in depth after their initial chat. Paige likes her, feels comfortable with her. This resource is invaluable. After my mother-in-law was killed in a car crash 3 years ago, the middle school guidance counselor became a refuge for Paige. When she was sad, distracted, needed a place to go have a good cry or talk, she had a safe place with an adult to help her. These individuals are part of my team. We are working together and it’s so important to use them.
- I have always felt that it’s important to be honest about a diagnosis; that is, open and public. I know this doesn’t work for everyone. The downsides of being public about a diagnosis are outweighed by the negative pressure for children if they have to keep a secret and bury feelings about such a serious topic. Children take their lead from you. If you are up front and comfortable discussing it, your children will learn to be that way, too.
- Call your other medical professionals and tell them of your diagnosis. Not only will they want to know because they care, but there may be instances where treatments may need to be examined or medications evaluated more often (for example, my endocrinologist wants to monitor my thyroid hormone levels more often than usual). They are all part of your team. They want to know. Many of the most touching and heartfelt phone calls I got were from my doctors this week. They cried with me, gave me information, offers of help, and caring. It also means if you have a situation when you need urgent medical care their office will already be aware of the situation and will likely respond more quickly to get you in to see the doctor.
- A carefully worded email is invaluable. Accurate information is documented so people don’t spread rumors. Friends can refer back to it if needed without asking you. They can forward it to other individuals easily, as can you. Choose your words carefully. The words you use will be repeated so make sure the email says what you want it to say to friends and relatives. The right explanation is much more helpful than a quick one sentence Facebook status update. People will have questions, and you can head many of them off by including that in your email (if you so desire).
I will be posting more tips about what I’m doing in the weeks and months ahead. Hopefully they will help you or someone you care about. There is so much you can’t control during this time, and that’s unnerving. Even taking steps like these can give you concrete tasks and a feeling of accomplishment that you are helping yourself and those you love.
April 2nd, 2012 §
We gather friends like seashells throughout our lives, tucking the treasures away to take with us as we walk. At different times, we appreciate different qualities of those friends; characteristics that initially attract us to someone may later be a source of discomfort. Some friendships last entire lifetimes, others are brief but intense. Friendship is an art form, one we must learn and practice daily.
I recently read Lindsey Mead’s post about friendships made during life transitions. She writes, in part: “It strikes me that it is not an accident that our truest and most lasting friendships are forged during times of life transition; we are closest to those who have shared experiences that changed who we are. Whether it was childhood, college, or becoming mothers, this is true for me.”
I’ve thought about this for weeks because while I absolutely understand what she is talking about (and do have some friends like this), I’ve also seen many of those friendships fall by the wayside. I have written before about the ways cancer and friendship sometimes don’t mix. There are friends who just can’t deal with a friend’s illness and/or death of a family member and they just disappear. In contrast, there are friends who seem to thrive on helping when there is a crisis underway.
When I was diagnosed with breast cancer at 37 I did not have any friends who had already had the disease. One of my closest friends has a son who had experienced leukemia twice and received a bone marrow transplant from his sister that saved his life. I talked with her a lot, not only because she had some sense of the fears I had but also just because she is my friend and a great listener. While I treasured that connection, though, I didn’t know anyone who had recently had a double mastectomy, chemotherapy, or needed to figure out how to balance those treatments with caring for three young children. My diagnosis preceded my involvement with Facebook and Twitter; social media would have greatly changed my experience with cancer.
I didn’t like support groups; they just weren’t right for me. Instead, I found myself talking to and finding support from a few women who used some of the same surgeons I did. We’d see each other in the waiting room at the plastic surgeon’s office when we went for weekly “fills” to add saline to the tissue expanders in our chest that were stretching the skin and making space for the implants some of us chose to receive. During chemo, nurses would often try to put younger patients in the same semi-private chemo room so they could meet and pass along wisdom and support.
Not every interaction I had led me to a friendship, of course. Sometimes in stressful situations we just need someone to help get us through. Like the stranger in the seat next to you during a turbulent airplane ride who chats with you and passes the nervous minutes, we rely on strangers to steady us when we wobble. We look for cues that everything is okay, that our experience is in the range of what might be expected.
But as my chemo and surgeries and constant doctor appointments waned, there was more room for “the rest of our lives” in the conversations I was having. One woman and I became quite close; we’d meet for coffee and spend hours talking about cancer, its effect on us, our children, our spouses. We were different kinds of people, though, in dealing with our similar cancer diagnoses. As time went on, it became more and more apparent. For example, she didn’t want to share as much information with her children about her cancer as I did. She turned to controlling food as a way to deal with her fears of a recurrence; she felt she would be immune from a recurrence if only she only ate certain foods. She wanted to train to be a Rekei healer. Eventually, though, it was our disparate attitudes about cancer that drove a wedge between us. She felt it was important to always put a sunny face on cancer; she felt it was necessary to find the joy in it. She had a “head painting party” when she went bald from chemo. She had her daughters paint her head with designs and words. She collected positive sayings into a little book that extolled the virtues of positive thinking as a key to remission success.
I could be her friend and listen but I could not agree with what she believed. The thought of someone placing their hands over my skin but not touching it and transferring energy to me (Reiki) did not work for me. I didn’t believe that food was key to avoiding cancer (after all, I had friends who had been vegetarians before they got cancer; if food were the simple key to avoiding cancer we’d have figured that one out by now, I thought). I felt control of food was a grief reaction, a way to manage fear in an uncertain world. That difference alone would not have come between us, though. I think it was the “positive thinking is the key” that I think was the biggest stumbling block. We just fundamentally differed about how to approach this disease that dominated that period in our lives.
I was strong, determined, motivated. I researched the available options and discussed them with my medical team. I pushed back when they suggested certain treatment options. I was a participant in my treatment plan. But I also felt that this thing called cancer SUCKS. And it was okay to say that. It was okay to have a bad day, or hate shaving my head. I didn’t have to have a head painting party and rejoice in the experience of going bald from chemo. It was okay for me to get halfway through shaving my own head in my garage on the morning of my second chemo and tearfully ask my father to help me finish because I couldn’t get it all. It was okay to cry, to scream, to pout for a bit. Then I picked myself up and moved on. That’s what worked for me.
Every time I got a piece of bad news or felt overwhelmed after a doctor’s appointment I allowed myself 24 hours to recover. That day I could complain, feel the injustice of it all, just react. But the next morning: it was time to get on with it. Those negative feelings were important to me. They were real. They were how I felt. And having someone constantly saying that I should only think positive rubbed me the wrong way. It was, to me, “pinkwashing”: making breast cancer seem less awful than it often is. If the only things I expressed were how “cancer is a gift” and I “had to find the beauty in it” (as she did) that denied a very real truth to me: cancer had fundamentally changed my life and those around me, and those changes weren’t always positive.
It didn’t mean there weren’t experiences or people or lessons that I appreciated. It didn’t mean I didn’t want to emerge a wiser person for having gone through it. But “cancer is a gift”? No way. I saw blogs and books where survivors wrote, “Cancer is the best thing to happen to me.” I will never say those words. I think of all of the people in the world who live with cancer every day, whose lives will be cut short by it, who have lost people they love to the disease. In my mind it diminishes their deaths and diminished quality of life to say their disease is a gift. I will not say that cancer was the best thing to happen to me.
My friend and I just sort of fell out of touch, though we have talked a few times in the last few years. We have only warm feelings for each other and wish each other good health and happiness. But we aren’t close. And what that tells me is that cancer is a part of life. You can’t make a relationship work just because you have the same disease. We have different kinds of friends for different reasons. Some we love them because they are “just like us” and share common interests or senses of humor. Some we love them precisely because they are different– they push us in ways we are not accustomed to or expose us to interests or information we otherwise might miss. In this day and age we have Twitter friends, best friends, school friends, Facebook friends, etc. We interact with a variety of people in very different ways.
I also realize that we have different levels of patience for conflicts at different times in our lives. Maybe the differences I had with my friend about cancer wouldn’t bother me so much now. Maybe we were both raw and stressed about managing our illnesses and our families. We supported each other through the hardest times and once that period was over we just moved on in different ways. Maybe that wasn’t even what really caused our relationship to cool off in the first place; after all, we didn’t part ways on bad terms, the friendship just “fizzled.” It happens.
I realize I’m more likely to make friends in the daily grind of life, and my life is full of more people I consider friends than ever before. I have a rich network of people I like, trust, and enjoy spending time with. We are not always similar, and we don’t even have to share the same beliefs all of the time. Respect and kindness are hallmarks of friendship, and every relationship for that matter. I really enjoyed thinking about the friendships I’ve made, how I’ve made them, and which ones haven’t worked. The topic of cancer and friendship is one I will continue to write about. I treasure the friends I have. I am fortunate.
Thank you to Lindsey for planting the seed for me about this topic; she and her blog frequently push me to think, learn, and grow. I’m still ruminating on this subject… and I like that.
December 14th, 2011 §
My mother retired a few years ago. For much of her adult life she was a psychologist specializing in grief and loss, death and dying. She wrote her dissertation on the impact a child’s death has on family dynamics. She used a case study method, doing in-depth interviews with surviving family members of various tragic events that happened. In one case, a house fire killed a child; in another, a baby died of SIDS.
They were heart-wrenching stories, and even as a child I could tell this was “heavy stuff.” Of course I couldn’t comprehend the magnitude of a parent’s love for his/her child until I had my own; but, I realized in reading the transcripts that grief is a multi-faceted emotion. And that loss is a process.
Having my mother work in this somewhat unusual profession was excellent training. I learned at an early age so much about sympathy, empathy, guilt, regret, and the discomfort our society feels about the subject of death. Despite the fact that it is the one thing that unites us all, the one common thread in all our lives, most people just don’t want to explore the subject of death. It makes people uncomfortable, makes them squirm, and almost universally makes people change the subject.
When you have had a death in the family, people don’t know what to say. In fact, it is likely many people won’t bring it up. Often, they worry that they will be reminding you of the tragedy, as if you have forgotten it. Anyone who has experienced a death of a loved one knows this isn’t true. The deceased person is never far from your mind, from your heart. And more often than not, you want to talk about that person. My mother taught me this. She taught me that people will never be upset if you remember and talk about the person they loved; it means their legacy lives on. Everyone wants to be remembered. You honor this desire when you talk about a deceased person.
I have said many times that growing up with my two parents was the best training for my string of illnesses through the years. While cancer has been the most serious, it has by no means been the only medical challenge I’ve had. But having a surgeon for a father and a psychologist for a mother was perfect.
I was able to digest complex medical information. When surgeons told me what needed to be done I could weigh my options methodically. I could weigh options of treatment and ask good questions to determine the best course of action for me. I could read pathology reports with ease. And then I could be insightful into my emotional response, being introspective and analytic
And being insightful and analytic about a life-threatening disease means confronting mortality. Often I hear stories of people dying without a will. In fact, often it’s only once people have children that they feel sufficiently motivated to create a will, because their love for their child (and making plans for a guardian) is the only thing that can make them confront this fear.
Often when I was in the midst of chemotherapy I wanted to have conversations about the “what ifs.”
What if they didn’t get it all.
What if the chemo doesn’t work.
What if the cancer comes back.
What if I get another (worse) kind of cancer from the chemo.
What if I die.
No one really wanted to talk about the last possibility even though it wasn’t outlandish. (Interestingly, people are very intrigued with my recurrence likelihood and mortality statistics… they view the numbers as easier to talk about in the aggregate rather than just discussing my own death).
I viewed talking about my death as responsible. I wanted to make sure Clarke understood that if I died, I wanted him to find another wife. I wanted him to be happy and loved. I wanted our children to have a mother to love them. Unsurprisingly, my greatest worries centered on my children.
I sat with a friend at coffee one day and voiced some of these concerns. With 5 children of her own, my friend is an amazing wife and mother in all respects. At first she was resistant to talk about my death with me. She didn’t want to entertain that notion. But I pressed the issue. And finally she looked me in the eye and said, “If you die, I promise I will watch over your children. I promise I will make sure they have the right person love them and raise them. I promise you that I will make sure that happens.” I think she figured it was the fastest way to shut me up. I think she figured she would agree to anything I was asking just so we could get off the subject. But at some point I think she realized that it was really important to me. I wasn’t going to let it go. And I wasn’t going to be able to get past it until I felt they would be safe and watched over. So she told me what I needed to hear. And I know she meant what she said.
Like a balloon slowly deflating, I felt my body go lax. Finally, I could let it go. She had promised me she would do for me what I wanted. I could trust her, and I could move my worry to something else. She did more for me by making this promise than she will ever know.
Here is one of the things I’ve learned from my mother: When someone you love is talking about death, don’t change the subject. Don’t trivialize their worries. Don’t say, “Let’s not talk about that now.” If they want to talk about it, it means it’s important to them, it’s weighing on them.
Focus on the fact that while we don’t need to sit around thinking about death all the time, there unfortunately might be times in our lives when we might not be able to think of anything else. If you haven’t experienced that, I applaud you. But sooner or later, you or someone you love will.
October 18th, 2011 §

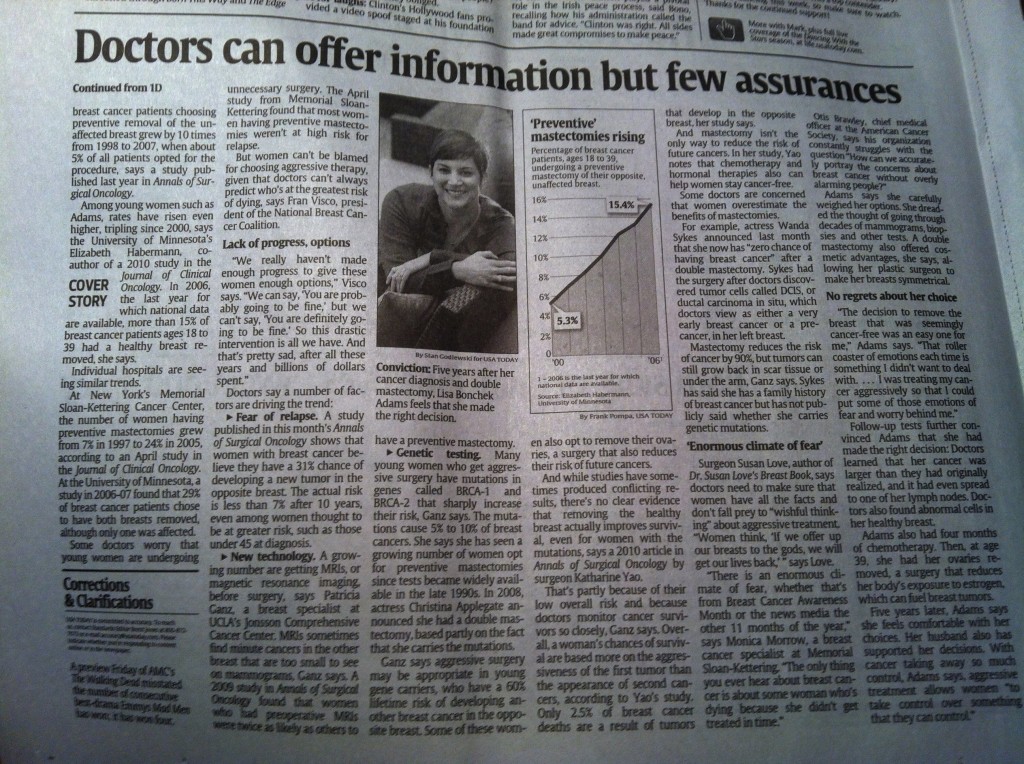
For those of you who missed it yesterday, click here to the USA Today piece that Liz Szabo did about the decision for some women with breast cancer to have a mastectomy.
Everyone was so supportive in sharing publication day with me… thank you. The enthusiasm from Facebook and Twitter friends was truly touching.
The kids feel like celebrities! The photo on the cover page of the Life section was huge and the photographer captured a great laugh with the kids. The children were so patient during the 1.5 hour photo shoot.
I’m still working on a big post with more about the subject of mastectomies for breast cancer. I promise to have that up as soon as I can.
The response was overwhelmingly positive but there were a few criticisms of my decision. Here is what I reply:
I don’t believe that my decision to have a double mastectomy was a guarantee that my cancer won’t come back. There was much I could not control about cancer; some of that uncertainty still remains. However, how you treat your cancer, live with it, and monitor it are things you can control.
The shame is that when observers (many whom have no direct experience with cancer) decide to be critical of people with the disease, survivors may be afraid to tell their stories. Cancer awareness– true awareness– can only happen when men and women with breast cancer feel comfortable enough to talk about their experiences, their choices, and their disease without fear of being challenged.
I will continue to tell my story.
September 27th, 2011 §
A previous discussion about inspiration and setting an example provoked my friend Laura to write to me, “If something ever happens to me where I have to dig deep to find that strength that you have found (and shown), I will think of you. Often. And re-read your blog. Often.”
This was the highest compliment and I appreciated those words immensely. Her words got me thinking.
So many of my friends have mothers who’ve had cancer. In college, my two closest friends, Alex and Deb, both had mothers who had breast cancer. Somewhere in that experience was an expectation for them that someday, inevitably, they would have it too.
It was many years before my own mother did. And then right on her heels, so did I. Before Alex and Deb did. And so, like my mother was for me (see Everyone Needs a Trailbreaker), I suddenly became the trailbreaker for my best friends.
I’ve gone through some cancer scares with friends and acquaintances over the past three years. I’ve sat in waiting rooms, taken phone calls, written emails, met with women in person. I’ve helped friends, strangers, and friends of friends.
When I was young someone teasingly called me a walking encyclopedia. Somehow it still seems true. My husband only half-jokingly shakes his head when he hears some of the questions people ask me. He sometimes says, “They do know you’re not a doctor, right?”
I know that I’m the first of my friends to have breast cancer. And have it “bad.” The whole nine yards. That experience comes with responsibility. I know that having cancer at 37 means that I will be that resource, that friend, that support system.
In the future, others will need me. Friends will ask me how to help, what to do, what things mean.
There is a lot of pressure coming my way and I think about it already: what if I let them down?
That’s the kind of person I am.
I am already worried not only about getting through my own experience; I’m worried how I can help my friends if their time comes.
And statistically it will.
I’m worried who will be next.
I’m angry someone will be next.
I want to be the lightning rod.
I want to take in on for them.
I want to protect them.
Laura, I want to protect you:
I don’t want you to have to read my blog for strength.
I want you to read it because you want a window into a world you never have experienced. And never will.
That is my greatest hope, my greatest dream.
If I could sleep, that would be my dream:
To keep you all safe.
July 14th, 2011 §
Sunday will be the four year anniversary of the day I had breast recontruction surgery after cancer. My tissue expanders were removed once chemotherapy was over and my silicone implants were put in. Last week I had my annual visit to my plastic/reconstructive surgeon and received the all-clear to now have a visit every two years. It’s always gratifying when the time in between visits gets longer; I remember when I was there at least once a week during the reconstruction process.
“Did you know it’s been four years since your surgery?” my surgeon asked. Immediately he chuckled, “Of course you know that,” he said, realizing my mental calendar was certainly more precise than his– of course I marked the days off in my head.
Whenever I sit in a waiting room I am instantly transported to that place and time. I sit and watch patients walking in and walking out. I can tell by hearing what the time interval until their next appointment what stage of treatment they are in.
I sit in the chair, the same one I did four years ago.
It’s the same chair, but I am not the same person.
My body is not the same.
There is continuity in that chair.
There is a story it tells me.
I wrote this piece to the next person who sits in that chair.
………………………….
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
A cure.
Don’t you think that would be amazing?
I think so too.
July 5th, 2011 §
I met a woman who told me something shocking.
It wasn’t that she’d had breast cancer.
Or had a double mastectomy with the TRAM flap procedure for reconstruction.
Or that she’d had chemotherapy.
What made my jaw literally drop open was her statement that she has never told the younger two of her four children that she’s had cancer.
Ever.
Not when she was diagnosed.
Or recovering from any of her surgeries.
Or undergoing chemotherapy.
She never told them.
To this day– five years later– they do not know.
I like to think I’m pretty open-minded. But I confess, it took a lot of self-control not to blurt out, “I think that is a big mistake.”
I’m a big believer in being open and honest with your children about having cancer. My caveat, using common sense, is that you should only give them age-appropriate information.
When I was diagnosed with breast cancer Tristan was six months old. Of course he didn’t understand what cancer was. Colin, age 5 at the time, understood some of what was happening. I explained to him what cancer meant, that I was going to need surgery to take the cancer out, where the cancer was, what chemo was, what it would do to my appearance and energy level. Using words like “I will be more tired than I usually am. I might feel sick to my stomach and need to rest more” explained things in words he could understand.
Age 8 and the oldest at the time, Paige understood the most when I was diagnosed. She had bigger questions and well as concerns about me (“Will I get it too? Who is going to take care of us? Are you going to be okay?”).
It’s not that I think small children always understand everything. But they are certainly able to sense that things are not “normal.” They can tell when people are acting strange. I think it’s important that they know there is a reason for that change. Children have a tendency to be egocentric; they think that everything is their fault. They may think they have done something wrong if everything at home feels different.
The woman told me she didn’t want to worry her children. She thought it “unnecessary” to tell them. She said when they got older she would explain it. I argue that by keeping her cancer a secret, she runs the risk of doing the opposite: making cancer seem scarier and more worrisome.
If children hear words like “cancer” casually in conversation as they grow up they will be comfortable with them; in that way, they won’t be frightened of them. If they understand the truth of the diagnosis and treatment they are dealing with reality. By hiding the truth, the unintended consequence is to make it seem worse than it is. By not telling children, and waiting until they are older, it reinforces the idea that cancer IS something “big and scary.” After all, if it weren’t, you would have told them already.
I think being secretive is a step backward to the days when cancer was only talked about in hushed tones: the “C” word or “a long illness.” These concepts might seem primitive to us now, but it wasn’t long ago that these vague labels were the norm. By showing our children, our friends, our neighbors, that we can live with cancer, live after cancer, we put cancer in its rightful place.
To me, the deception that goes on to lie to children about where you are going, what you are doing is lying about a fundamental part of your life. Cancer isn’t all I am — but it is a part. And it’s an important part of my medical history. If for the past 3 years I’d covered up where I was going and what I was doing, the web of deceit would have been extensive. I can’t (and won’t) live a life like that.
Further, I think it’s a poor example to set for my children.
Lying,
covering up information,
and omitting important information are all wrong.
With rare exception, the truth is always best.
Presented in the proper way,
commensurate with a child’s age,
a difficult situation can be not only tolerable but surmountable.
It takes work. It takes parents who can manage not only their own emotions about having cancer but also be involved with helping their children cope with it. It’s more work, but it’s worth it.
I think that woman made a mistake. I think her decision was harmful. I am sure she thinks she was doing her children a favor. I totally disagree. I think keeping this type of information from children “in their own best interest” is rarely– if ever– the right thing to do.
April 9, 2010
June 30th, 2011 §
It’s not that I didn’t like my right breast.
It hadn’t really ever done anything “bad” to me, except for the few times when it wouldn’t keep up with the milk production of the left one during the months when I nursed my children.
I didn’t harbor any negative feelings for it. In fact, I didn’t think about my breasts much at all except to chuckle at the sagging that inevitably comes with middle age and three pregnancies.
But all of that changed with four words: You have breast cancer.
The cancer was in my left breast: I needed a mastectomy. But what about the “good” breast?
Note the popular lingo: the non-cancerous breast quickly becomes tagged as the good one– like a good child who behaves and does what it’s told, the non-cancerous breast has faithfully done its duty and stayed healthy.
The left breast?
Well, that’s the traitor.
I had a decision: what would I do with the right breast?
Keep it?
Toss it out in biohazard trash?
With four words, that part of my body became a liability. I didn’t want that breast anymore, thanks. I’d rather have no breasts than one. Mentally, it was much easier to me to part with both, not live the rest of my life in fear of what might be lurking in that tissue.
To be clear, surgeons and oncologists explained that in their opinion, my chance of getting cancer in the right breast was no higher than my chance of getting breast cancer in the first place; I wasn’t necessarily at increased risk of breast cancer on the other side.
But:
I had already been a statistical anomaly.
I had gotten cancer at 37.
I was BRCA-1 and 2 negative (but didn’t know it at the time).
In my mind I thought:
Go ahead and tell me that, but I don’t believe you.
And so I heard their words.
I understood their words.
But I didn’t believe them.
And time proved me right.
I opted for bilateral mastectomies. And when the pathology came back, there was abnormal tube proliferation and some cell dysplasia. Things were awry in my right breast even though nothing had shown up on the mammogram.
Now, yes, eventually I would have found the problems when the cell proliferation got large enough to be detected on a mammogram or MRI. And maybe my chemotherapy would have gotten these cells anyway.
But are you really going to take that chance?
I wasn’t.
Body parts become liabilities.
My perspective about my body has changed so much in the last four years. My body itself has changed so much too.
I’m not exaggerating when I say that, like aging itself, the side effects of removing my ovaries one year after my mastectomies has changed almost everything about my health as I know it.
I went to the kitchen just now and pulled out my binder of cancer records to double-check my pathology report to write this blogpost.
And there it says, quite plainly, that my cancer was 1 mm from the deep margin (chest wall).
One millimeter.
A hair’s diameter.
A grain of sugar.
It always takes my breath away.
A millimeter.
So many people link their happiness to pounds, or inches, or dollars.
Me?
I think part of my future might hinge on that millimeter.
I’m counting on it.
And moving forward.
June 3rd, 2011 §
More often than not, cancer creeps into conversations with friends. New friends, old friends.
I don’t think I’m obsessed with it. I don’t have to talk about it. Why does it come up?
Is there a cancer radar?
Is it just that when cancer folks are together we let our guard down to share?
Do we want to compare notes and try to get information from each other?
Probably all of the above.
Here’s also where I think it comes from: talking about illness is grounding. It puts the emphasis where it should be. I have many friends who have family members who either have had or currently have cancer. We’re a club. There is a support we can provide for each other, a language we can speak. Stages, grades, blood counts, oncologists, PET scans, MRIs, tumor markers… and on it goes. I really think I should get credit for CSL… cancer as a second language.
I like people who “get it”; I find more and more that I am naturally drawn to them. I’m rarely surprised to find that new friends of mine have had some type of hardship in their lives.
Maybe it’s just that more and more people have “something” in their life story.
Maybe those are the people I gravitate to.
Maybe they are drawn to me (or the “vacuous people need not talk to me” sign I have on my back scares others away).
It’s not that I don’t like talking about shoes or The Bachelorette or movies. I do– a lot. And I actually do think they matter. It’s important to have a break from the heavy, serious stuff. Some people think that the small stuff is all there is– that it matters. Those people are hard for me to take.
One day, shortly after I was diagnosed, I sat watching my son take a tennis lesson. I was still numb and reeling from the news that I had cancer. I hadn’t started chemo, and was still awaiting surgery. I knew what I was facing: double mastectomy and chemo. But to the outside world I looked totally normal; no one would know what news I had received.
There were two moms sitting near me chatting loudly while their kids had their lesson. These were the days before the recession, when women in my town were flush with cash, and living high on the hog. They were talking about vacations. “I just can’t decide where we should go for vacations this year,” one said, “John has so many vacation days it’s going to be hard to use them all. We could go to Switzerland again. But that’s kind of boring. And there’s the Caribbean. But I kind of want to do something different. What do you think?” she said to her friend.
I know what I thought. I thought someone needed to hogtie me to the chair before I punched her out. That was a problem? It was one of the few times I really wanted to say “Lady, let me tell you about a problem.” But I didn’t.
Why?
Because maybe her mammogram was the next day.
Maybe she was a day from being told there was something suspicious on it.
Maybe she was a week away from having a biopsy.
Maybe she was a month from having a double mastectomy.
Maybe she was six weeks from starting chemo.
Maybe she was just about to learn the lessons I was learning.
May 1st, 2011 §
In the weeks before my surgery, I looked at pictures of double mastectomy patients on the Internet. I Googled “bilateral mastectomy images before and after” thinking I was doing research. I thought I was preparing myself for what was coming.
In reality I was trying to scare myself. I wanted to see if I could handle the worst; if I could, I would be ready. My reaction to those images would be my litmus test.
Some of the pictures were horrific. I sat transfixed. I looked. I sobbed. I saw scarred, bizarre, transformed bodies and couldn’t believe that was going to be my body.
Days later, when I met my surgeon for my pre-op appointment he said, “From now on, don’t look at pictures on the Internet. If you want to see before and after pictures, ask me– look at ones in my office. You can’t look at random pictures and think that’s necessarily what you are going to look like.”
All I could do was duck my head in an admission of guilt. How did he know what I’d done? I realized how he knew: other women must do this. Other women must have made this mistake.
The aftermath is terrible to me though not in the ways I’d anticipated. I have no sensation in most of my chest. I never will.
A major erogenous zone has been completely taken away from me. Yes, I have new nipples constructed, but they have no feeling in them; they are completely cosmetic. The entire reconstruction looks great but I can’t feel any of it. It does help me psychologically beyond measure to have had these procedures though.
Here I sit, two gel-filled silicone shells inside my body simulating the biologically feminine body parts I should have. And sometimes that thought is disturbing.
To be clear: I don’t regret having them put in. I’ve never regretted that. It was a decision I made, and made deliberately. I knew that reconstructing my breasts was the right decision for me. I’m getting used to them– I’m almost there.
I definitely don’t remember what my breasts looked like before. I only remember these.
I once asked my plastic surgeon to see my “before” pictures a year or two after my reconstruction was over. You know what? My “before” breasts didn’t look so great. In my mind they did.
In my mind, everything about my life before cancer was better.
But that’s not the truth.
My mind distorts the memory of my body before cancer. Then forgets it.
My mind distorts the memory of my life before cancer. Then forgets it.
With time, I can get used to a new self.
It’s like catching my reflection in the mirror: only lately do I recognize the person staring back at me.
For over a year the new hair threw me. It’s darker than I remember it being before it fell out. It’s shorter than it was before, too.
And the look in my eyes? That’s different also.
I just don’t recognize myself some days.
Sounds like a cliché if you haven’t lived it.
But it’s true.
April 15, 2009
April 28th, 2011 §
I almost stole it: the tape measure with the purple finger prints.
After all, my surgeon had left it in my room by accident. After he had marked me with his purple pen and left my room on his way to get ready for my surgery, he left it sitting on the counter by the sink. In my nervousness and tranquilized haze I didn’t see it until after he’d left. I figured I shouldn’t hold onto it as I was wheeled in (“Who knows what germs lurk in tape measures!” I thought), and that if I gave it to a nurse it might get misplaced. So I shoved it in my bag of personal belongings knowing I’d be in for an office visit shortly after surgery.
I actually forgot about it during the days I was home after my two-day hospital stay. The drugs, the pain, the shock of my breasts gone and numb chest filled with temporary tissue expanders were all I could think about.
I forgot all about it as I was shuttled around for weeks unable to drive. I wasn’t living my normal life, my normal routine. I wasn’t carrying my purse and keys daily. I was living in pajamas and constantly trying to adjust to a new body once the drains were removed.
Then while I was looking for my keys a few weeks after my operation I saw it: the tape measure.
The yellow fabric one with the purple fingerprints up and down its sides.
The one.
The one that had measured and determined where my body was to be cut.
It was there in my bag.
There wasn’t anything particularly special about its practicality; it was just a tape measure.
Just like the ones I have sitting around with all of the odds and ends that inhabit kitchen drawers.
But that doesn’t capture the social meaning of it.
It wasn’t just any tape measure. It was mine.
But it wasn’t just mine, I argued with myself—it wasn’t a personal momento for me.
For a moment or two I wanted it.
I needed it,
as if to remind myself what had been,
of what I had been.
It wasn’t mine, I thought– it was his.
But more than that, it was theirs; it was ours… the other women who had needed it.
Now I was one of them. It was a shared history we had: strangers who had endured the same surgery, whose faces and names I would not know.
We were bound together by this object which had literally touched all of us.
And then I realized it was my responsibility to give it back.
Not for the obvious reason that it didn’t belong to me.
But as usual, I thought of the other women: the ones who didn’t even know they had cancer,
the ones who were going about their normal lives that day, and in the days ahead, only days or weeks or months from learning the life-altering news that would change their lives.
I felt giving back the tape measure would be my way of being bound to them, of saying “I know what you have ahead of you. I’ve come from there, and we are in it together.”
And so when I went to one of my office visits, I took it out of my bag and casually handed it to my surgeon. “You forgot this in my room when I had my surgery,” I said. He thanked me and said “I wondered where it had gone to.”
Little did he know the journey it had taken.
April 13th, 2011 §
It seems like you can’t rank anguish. You shouldn’t be able to “out-suffer” someone. How do you quantify misery?
And yet, somehow we do.
“My problems are nowhere near as bad as yours.”
“I feel terrible complaining to you about it when you are going through so much yourself.”
I hear these types of comments all the time.
I make these types of comments all the time.
Placing ourselves in a hierarchy of pain and suffering serves to ground us; no matter how bad our situation is, there’s comfort in knowing there’s always someone who has it worse. Like being on a really, really long line at the movies or at the check-in at the airport, as long as there is someone behind you, it somehow seems better.
Hospitals use a pain rating scale: “On a scale of 1 to 10, how bad is your pain?” I was very intrigued when my son Colin was in the hospital for a week with a ruptured appendix and they asked him to rate his pain. At the time he was 5 years old and didn’t understand what they wanted him to do. He didn’t understand the concept of comparing one level of pain to another: it hurt… that’s all he knew. He used a binary scale to assess his pain: did it hurt or not? But as adults we know better: pain is not a yes-or-no question. Rather, there can be levels, ranking, quantification, and comparisons.
These mental exercises are necessary to keep us going through hard times, no matter what type. Before I got cancer, cancer was a “go-to” negative reference point. I mean, how many times have you thought “I’ve got health problems, but at least it’s not cancer”?
I did that. A benign lump needs to come out? At least it’s not cancer. A mole needs to be removed? At least it’s not cancer. My son has a cyst in his spinal column? At least it’s not cancer.
Then one day it was cancer.
So what could I pacify myself with?
At least it’s not terminal.
At least they can remove the body parts it’s in.
At least I have tools to fight it.
Then there was the big one: at least it’s happening to me and not my child.
I have a few friends with children who have had different types of cancer. These men and women (and their children, of course) are tough and have my utmost respect. I have thought many times, “That is harder. At least that’s not me. I don’t know what I would do.” When my son Tristan was diagnosed with deformities in his neck I thought “at least it’s something physical. At least it’s not something wrong with his brain. At least it’s not something that is fatal.” It’s cold comfort though. It’s still pain. It’s still grief. It is still hard.
I have often said I hate becoming anyone’s negative reference point. “At least I’m not her” someone might think of me. I always thought that meant they pitied me. I didn’t want that. But now I realize that it is okay for people to be glad they haven’t walked in my shoes– in reality, that’s what I want. I don’t want anyone to be where I have been; I’d like to be the lightning rod that keeps others I know safe. But, if it gives comfort to anyone to know that at least for today, their problems are not as big as mine, I think that’s good.
Because actually, at least for today, I’m doing just fine. I had laughs, and warmth, and hugs, and a day without pain—and I know that there are many people out there who can’t say the same.
Today I’m not the last one on line.
March 9th, 2011 §
Just because you know someone who died from cancer doesn’t mean I will.
Just because you know someone who:
felt sick,
felt great,
felt tired,
felt strong,
looked great,
looked awful,
lost her hair,
kept her hair,
ate healthy,
ate crap,
took vitamins,
ignored medical advice,
got acupuncture,
believed in holistic medicine,
ate no soy,
ate no sugar,
never laughed,
never cried,
had surgery,
had radiation,
received chemotherapy,
got silicone implants,
got saline implants,
had a great attitude,
had a terrible attitude…
Just because you know someone who did
one of these things,
many of these things,
some of these things…
doesn’t mean it will work for me.
It doesn’t mean it will kill me.
It doesn’t mean it will make me live.
Just because it worked for someone else doesn’t mean it will work for me.
It doesn’t mean it won’t.
Or can’t.
It might.
It might not.
Just because you know someone who died from cancer doesn’t mean I will.
January 18th, 2011 §
July 18, 2009
I went by my friend’s house today– the one who was just diagnosed with breast cancer. I wanted to put something in her mailbox. When I opened the mailbox it was full of mail already. She hadn’t taken in yesterday’s mail yet.
Of course she hadn’t. Why should she worry about mail when they are worrying about cancer and what it means for their family?
I left the bag in her mailbox on top of the day-old mail and went away, remembering:
Remembering that time in my life two years ago when I was diagnosed with cancer.
I managed to get the kids where they needed to go (I have no idea where that was).
I did the things I needed to do (I have no memory of what they were).
I went the places I needed to go (I can’t remember where they were).
There is no room for anything else in these days, these days in the beginning.
There is no room for anything else except to hear the words again and again,
as if you need to convince yourself that they are true: “You have cancer.”
There is no room to
do anything,
think anything,
say anything,
be anything,
fear anything,
hope anything,
dream anything,
live anything,
love anything,
breathe anything.
In these days there is no room for anything but cancer.
But these days will pass.
You don’t believe it.
Can’t believe it.
But it’s true:
these days will pass.
Your life will change.
You can make room for other things,
better things.
And once again,
there will be room in your mailbox.
You will remember to get the mail because you won’t be thinking about cancer.
You’ll be thinking about the things you should be thinking about,
that you deserve to be thinking about.
Each day.
Every day.
Today
January 16th, 2011 §
A previous discussion about inspiration and setting an example provoked my friend Laura to write to me, “If something ever happens to me where I have to dig deep to find that strength that you have found (and shown), I will think of you. Often. And re-read your blog. Often.”
This was the highest compliment and I appreciated those words immensely. Her words got me thinking.
So many of my friends have mothers who’ve had cancer. In college, my two closest friends, Alex and Deb, both had mothers who had breast cancer. Somewhere in that experience was an expectation for them that someday, inevitably, they would have it too.
It was many years before my own mother did. And then right on her heels, so did I. Before Alex and Deb did. And so, like my mother was for me (see “Everyone Needs a Trailbreaker”), I suddenly became the trailbreaker for my best friends.
I’ve gone through some cancer scares with friends and acquaintances over the past three years. I’ve sat in waiting rooms, taken phone calls, written emails, met with women in person. I’ve helped friends, strangers, and friends of friends.
When I was young someone teasingly called me a walking encyclopedia. Somehow it still seems true. My husband only half-jokingly shakes his head when he hears some of the questions people ask me. He sometimes says, “They do know you’re not a doctor, right?”
I know that I’m the first of my friends to have breast cancer. And have it “bad.” The whole nine yards. That experience comes with responsibility. I know that having cancer at 37 means that I will be that resource, that friend, that support system.
In the future, others will need me. Friends will ask me how to help, what to do, what things mean.
There is a lot of pressure coming my way and I think about it already: what if I let them down?
That’s the kind of person I am.
I am already worried not only about getting through my own experience; I’m worried how I can help my friends if their time comes.
And statistically it will.
I’m worried who will be next.
I’m angry someone will be next.
I want to be the lightning rod.
I want to take in on for them.
I want to protect them.
Laura, I want to protect you:
I don’t want you to have to read my blog for strength.
I want you to read it because you want a window into a world you never have experienced. And never will.
That is my greatest hope, my greatest dream.
If I could sleep, that would be my dream:
To keep you all safe.
January 14th, 2011 §
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
January 13th, 2011 §
There are ways in which I will never make you as readers understand what it’s like to have cancer if you haven’t. However, part of the reason I write this blog is to try to explain some of the cancer patient “mentality” (if you’ll accept such a generalization) to those of you who haven’t had cancer. To that end, you can hopefully be better friends, partners, spouses, sons, and daughters. There are things I didn’t know before I had cancer that I wish I had understood.
It’s not that I am special. It’s not that I am so smart. It’s that I have been there. Hopefully sooner than you have. And so I am reporting back from the field. To try to help you. Prepare you. Because if there is one thing I know, one thing I know for sure: you will know someone. It might be your friend. Your parent. Your child. Or even yourself. Maybe you already know someone. But one thing is for sure: you will know someone who gets cancer. And you know what? You already know me.
One of the ways your life changes when you have had cancer is that you begin to understand the phrase “It’s never over” in a whole new way.
As soon as you hear the three words, “You have cancer” your life changes. From the time you hear those words everything is different. You now have a history of cancer — even if it’s a cancer that can be removed and you don’t need any other treatment. It is now a history that puts you at risk. Now every medical problem, every medical history you give, every question mark, every medical mystery must be filtered through the lens of a history of cancer.
A woman I know from college was writing a brief note to me by email to thank me for something nice I’d done. The last part said, “Hope you’re feeling on top of the world (or close to it).”
My reaction? First I burst out in laughter.
Ah, the naiveté of the healthy!
On top of the world! Ha!
Then it actually got me riled up.
Angry.
How dare she think it was over.
Then I got angry at myself for lashing out.
I became contrite.
Why should she know better?
How could she know better?
It isn’t fair to expect people to know better.
Only once you know better can you do better.
If she only knew.
What was I going to do?
Write back and explain to her the error in her thinking?
Should I write back and say:
I counted every day, every hour, every minute, every second to be “done.” But when each thing was “done” there was always something else I was counting toward. Always something else looming. I’m never “done.” It’s never “done.” It’s never “over.”
The language we use reveals a lot.
When someone says,
“You must be on top of the world,”
that means:
“You should be”
“You ought to be”
or
“I expect you to be.”
For someone like me, if I don’t feel like that it’s hard.
I get angry. I want to say all of the reasons why that’s not realistic– why that’s wrong. Why that’s precisely what I’m not feeling.
But then, when my anger cools, I take that and turn it inward. And all I feel is disappointment. Disappointment in myself. Maybe I should feel like that. Maybe I really should feel on top of the world. The fact that I don’t means I’m not as far through this thing as I thought. It reminds me I’ve still got a lot of work to do.
Maybe the battle is not really with cancer. Maybe it’s with myself.
But I think the point remains: just surviving cancer isn’t necessarily enough. It’s not enough to make you feel on top of the world.
You can help those who have had cancer by not making the leap that just because they have lived through this round that they have “won”; don’t assume that they will necessarily be ecstatic, “done,” and ready to move on.
Rather than telling people what they “must” feel, we all can be better friends and listeners by asking questions rather than making statements.
Rather than saying “you must feel on top of the world” think of the difference it would have made if my friend had said, “Now that your treatment and surgeries are over, how do you feel?”
An open-ended question is always a safe conversation starter. I’m going to try it more often in my everyday life; I hope you will too. My wish is that it begins some good conversations between you and someone you care about.
January 12th, 2011 §
That chair you’re sitting in?
I’ve sat in it too:
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too:
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too:
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too:
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too:
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too:
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too:
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too:
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
No more cancer.
Don’t you think that would be amazing?
I think so too.
January 10, 2010
January 11th, 2011 §
June 18, 2010
There. I did it.
This picture shows me one month after I finished chemo. Peach fuzz growing. Eyebrows gone. Eyelashes gone. Both pencilled in to hide their absence.
 This is the only picture I have of myself bald. When I was a shiny cue ball it never occurred to me to document it. If you look closely at my left eye, you’ll see a tear resting on my lower lid. I had just stopped crying. Long enough to put on makeup and flash that killer smile. I was just about to get my tissue expanders out and have my silicone implants put in. It was right before my 38th birthday. That’s what I told my plastic surgeon I wanted for my birthday– to be done with that next phase of my reconstruction.
This is the only picture I have of myself bald. When I was a shiny cue ball it never occurred to me to document it. If you look closely at my left eye, you’ll see a tear resting on my lower lid. I had just stopped crying. Long enough to put on makeup and flash that killer smile. I was just about to get my tissue expanders out and have my silicone implants put in. It was right before my 38th birthday. That’s what I told my plastic surgeon I wanted for my birthday– to be done with that next phase of my reconstruction.
It was hard to go in for that particular surgery at that particular time in my treatment regimen. When the staff came to wheel me in I had to remove my scarf. My surgeon hadn’t seen me bald. The nurses, my father, my doctor… all of them saw my head then. Of course it was run of the mill for them. They saw cancer patients all the time. But for me it was another way my dignity, my identity, my humanity were being stripped from me. I donned the fabric shower cap gladly, happy to have something (albeit flimsy) to conceal my naked head.
Only moments before, I stood in the bathroom with my plastic surgeon while he marked my body once more with his ubiquitous purple Sharpie pen. We talked again about final details of my breasts. I realized how these conversations had become so routine between us. While the subject of my breasts was no longer one that even caused a pause in chatter for us, I didn’t want him to see my head. Somehow it was more personal, more private, more embarrassing to me than the fact that he not only saw, but touched, drew on, and even photographed my breasts on a regular basis during reconstruction. Those interactions were scripted. Defined. But my head? I hadn’t realized he was going to see that. And there was embarrassment there. It wasn’t happening on my terms.
So today I am taking control and doing it on my terms. When Melissa Etheridge performed bald at the Grammys in 2005 (before I was even diagnosed) I remember thinking, “She is strong. She is real. She is brave. She is beautiful.” What she did in that moment was important. I bet it was liberating to her. So I’m going to try it. It’s too late for me to try it in reality (and I don’t want to pull a Britney Spears and shave my new hair off to be bald again).
Today is the 2 year anniversary of the day I finished chemo. So, in celebration, I’m taking off my metaphorical scarf. I’m going bald here today. I want to see how it feels.
January 10th, 2011 §
January 30, 2009
I had two surgeons that day:
one just wasn’t enough for the job.
The surgical oncologist would take away,
the reconstructive surgeon would begin to put back.
Before I headed off into my slumber,
I stood as one marked me with purple marker.
He drew,
he checked,
he measured.
And then a laugh,
always a laugh to break the tension:
Surgeons must initial the body part to be removed to ensure
they remove the correct one.
But what if you are removing both?
How silly to sign twice,
we agreed.
And yet he did,
initialing my breasts with his unwelcome autograph.
The edges of the yellow fabric measuring tape he used
had purple fingerprints up and down their sides;
use after use had changed their hue.
And now it was my turn to go under the knife–
a few more purple prints on the tape.
I got marked many a time by him that year.
Endless rounds of
purple dots,
dashes,
and lines
punctuating my body
with their strange, secret blueprint
only those wearing blue understood.
We stood in front of mirrors
making decisions in tandem
as to how my body should and would take new shape.
Two years today and counting.
Moving forward.
Sometimes crawling,
sometimes marching,
and sometimes just stopping to rest
and take note of my location.
Numb inside and out,
but determined.
Grateful,
hopeful,
often melancholy.
Here comes another year
to put more distance
between
it and me.
Let’s go.
January 6th, 2011 §
Some days I say to myself, “Enough with cancer.”
Some days I say, “That’s enough. No more.”
No more thinking about it.
No more doing.
No more helping.
No more advocating.
No more educating.
No more communicating.
But then I say, “There’s still so much to do.”
There’s still so much to say.
There’s still so much to hope for.
There are still so many who suffer.
And so I am pulled back in,
Writing, talking, sharing.
Some days I want to talk about anything but cancer.
But I remember this is the new me,
This is my new life.
This is who I am.
And as long as there are others who come after me,
I will do what I can…
to hear,
to help,
to hope.
December 30th, 2010 §
One of my favorite romantic movie moments occurs between Denys (Robert Redford) and Karen (Meryl Streep) in the movie Out of Africa. The two lovers are out in the African desert at a fireside camp. Karen leans her head back into Denys’s hands. He washes her hair gently, then cradles her head in one hand and pours water from a pitcher, slowly and gently rinsing the soap from her hair after he’s done washing it. It’s a tender moment, to me utterly soft and sensual.
Before I left the hospital after I had a double mastectomy, the staff told me I might not be able to lift my arms over my head. With both sides affected, they said, I’d likely be unable to wash my own hair.
Recovery is slow in the week after surgery. A clear thin tube (like aquarium tubing) is literally sewn into a small hole in the skin under each arm. It carries excess fluid away from the mastectomy site as it heals. Fluid is collected into a small “bulb” and measured every few hours. After certain medical criteria are met, the drains are removed, the incisions sewn up, and then you can finally take that longed-for shower. Eight days after the surgery I received the all-clear. As any mastectomy patient will tell you, the day you get your drain(s) out is a great day.
Only then did I try to lift my arms. And hurt it did. I tried to shrink down into my body. I tried to be a tortoise withdrawing my head back inside my shell, shortening my height so I wouldn’t have to lift my hands so high to reach my hair. It was a painful challenge. I worked up a sweat trying to get my fingers to touch my scalp. I knew it was a questionable proposition. But I thought I could do it.
I thought about that scene— that romantic tender scene from Out of Africa. And I started laughing. I laughed and I laughed and tears came down my face. That cry hurt. It was one of those “I’m laughing and I’m crying and I’m not sure if it’s funny or sad or both and I don’t want to think about it so I’ll just go with it and I hope I’m not on Candid Camera right now…”
I was laughing at the absurdity of it. Here I was. It was my chance to get Clarke to wash my hair. My big fantasy moment. I was going to be Meryl Streep and he was going to be Robert Redford and he was going to wash my hair. Except I couldn’t move without pain. And I certainly wasn’t feeling romantic. I had just had my breasts removed. And I had these weird temporary breasts (tissue expanders) in their place. And my chest was numb. And my underarms hurt from having tubes in them for a week.
Because I hadn’t properly showered I still had purple Sharpie hieroglyphics all over my chest. And I had no nipples. And I had big scars and stitches in place of each breast. And a small angry scar with stitches under each armpit where the drain had just been removed. Let me tell you… this was clearly not how I envisioned beckoning my loving husband to come make my little movie scene a reality.
Now, don’t get me wrong. Had I called him from the other room, he would have done it in a second. He would have been there for me, washed my hair, and not made me feel the bizarre, odiferous (!) freak I felt at that moment. And I would have loved him for it. But I did not want him to see me like that.
In that moment I had a dilemma. What kind of woman was I going to be?
What kind of person was I going to be with this disease from that moment going forward?
I was going to push myself. Do it myself.
I wasn’t going to be taken care of if I could help it. I knew I was going to have trouble asking for help, have trouble accepting help. I knew these things were going to be necessary. But I also knew they were going to cause me problems. That’s the kind of person I am.
I knew asking for and accepting help were actually going to make me feel weaker than I was already feeling. And it was only the beginning. I knew these actions were going to make me feel weaker than I knew I was going to get. I wanted to do everything myself for as long as I could. That was what was going to make me feel alive: doing it myself.
I am not sure I did the best job washing my hair. I probably missed a spot or two. But I did it. And I didn’t ask for help.
Granted, it was something small.
But in that particular moment, on that particular day, that particular act gave me a feeling of pride as big as anything else I could have possibly accomplished.
a postscript: I wish I had been more accepting of help in the early days. I wish I had not seen it as a personal “weakness” the way that I express here. I don’t want to change what I wrote then, but I do want to say that I don’t think I was right to push myself so hard. If I had it to do over again I would accept help more often; maybe not for the hair-washing, but definitely for other tasks that I should have outsourced. I have learned from my experience.
December 24th, 2010 §
Originally written December 25, 2008
(three weeks after my salpingo-oophorectomy and two years after my diagnosis of breast cancer. This was actually the first blogpost I ever wrote.)
I’ve only cried once today. That’s not too bad. But the day is not yet done. Today, again, I’m thinking of the things that cancer has taken from me. First, let me say that I am well aware of the blessings I have. I remember them each and every minute of every day. They are what keeps me going, keeps me fighting. But today, again, I’m pulled into what’s gone, what’s irretrievable, what’s changed.
The body parts are gone, of course. My feeling of immortality. Of safety, of security. I’m vulnerable now. And I feel it. Part of me wants to blaze down I-95 at 100 miles an hour because I’ve stared down cancer, so what can touch me now? Taking risks is a popular grief reaction. On the other hand, a part of me wants to curl up in bed and not come out.
Today, on Christmas, when the childlike wonder is all around, I feel like I am watching it from high above me, as it happens TO ME, around me. I smile, I do what I am supposed to do, I play the “Santa game” with my children. I eat delicious food. I gather up the gift wrap strewn about the living room. I pile the presents in the kids’ rooms. I pack their suitcases for their 3:30 a.m. wakeup for their winter vacation. Half my family is leaving me tomorrow. They’ll be back, of course, but they are leaving. And while they are gone I will ponder the sadness that has settled like a cloud since my latest surgery almost a month ago.
I know I’ll be fine… everyone tells me so, as if to will it to be that way. Even in my darkest moments I know it is only temporary. But I am angry at cancer. Angry at the bad twist of fate that makes me unable to travel this year, unable to be myself, unable to shake this feeling that the dark cloud just seems to keep following me, like those creepy paintings in the museum whose eyes seem to follow your every move.
And knowing the other people who are similarly sad today, those who are remembering loved ones lost, and those who are suffering in pain, and those who will head in for more chemo and surgery and therapies before the year is out are also forever changed by the great equalizer of cancer.
To anyone who reads this and thinks it sounds so odd, so foreign– something that happens to “someone else”… I am so happy for you. I am jealous of you. I remember that feeling, but I am almost getting to the point where I am unable to remember it. I never thought it would be me thinking this way, feeling this way. But it is me. And it’s taking a long time to grieve for that life I thought I would have.
Maybe that’s what it is.
I’m in mourning.
I’m mourning the life I thought I would have.
And only time can help that.
December 20th, 2010 §
Four is just a word. So is three. But once again today I will change one word on the welcome page of my website.
“It has been three years since hearing the words ‘You have cancer,'” the first sentence says.
And now, today, it becomes four.
I think about days like the one four years ago — days that start innocently, normally, benignly. In the hours leading up to the mammogram I wasn’t worried about anything.
I think about the sentence that changed my life.
I think of where I’ve been, where I am, where I am going.
I think of those I’ve met along the way: new friends, doctors, nurses, strangers.
I think of those who have died from cancer and other causes since I was diagnosed.
I think of the progress we’ve made and the distance we have yet to go.
I think of what today might bring, and tomorrow.
And then, in a sudden reversal, I stop myself from thinking too much.
“It’s time to go live my life,” I tell myself. Thinking is good, but only so much.
“It’s time to go live my life,” I tell myself…
Right after I change that one word.

To read about the chronology of my diagnosis, go here.
December 17th, 2010 §
originally published September 12, 2009
My friend Andrea found out she needs to have chemo. I cried a lot the day I found that out. Last night she emailed me that she was thinking about the whole “losing her hair” thing. She has gorgeous hair. Thick. Straight. Reddish-brown, in the sun I’d say it has a honey shine in it. She usually wears it back in a ponytail, as she says, “taking it for granted.”
I started writing her back to tell her that focusing on her hair wasn’t silly. There are many things about cancer that are real worries. One of them is going bald. Especially for a woman. And as I typed to her I realized the words were flowing fast and furious.
I realized all the things people had said to me when I was worried about losing my hair and all of the things people had said to me after it eventually happened.
Everyone wants to reassure you that it isn’t as bad as you think it is.
Some days you convince yourself it isn’t that bad.
Some days you are sure they are all lying to you.
Either way, you get through the days.
The day you take that hat or wig or scarf off and wear your newly-grown stubble or “mouse fur” out in public is a great day (My first hair was so fine and soft and thin that it didn’t resemble hair at all… I called it mouse fur because while it blissfully covered my head and was dark, it couldn’t be cut or styled).
So, for my friend, and for other women who are getting ready to start chemo (and those who bravely walk through the world every day without hair because of alopecia and other conditions), no matter what, it matters.
No matter what anyone says…
all the things they will say:
It’s only hair.
It’ll grow back.
You’ll look so pretty anyway.
With a face like yours it won’t matter.
We’ll get you a cute wig.
We’ll get great scarves.
It’ll grow back in no time.
Maybe it’ll be better after it grows in.
It might be curly.
It might be straight.
I know someone whose hair came in gray.
I know someone whose hair came in red.
I know someone whose hair came in black.
I know someone whose hair came in white.
Hers came in curly.
Hers came in straight.
Did you see hers?
It looks great.
Did you see hers?
It looks awful.
I like her better with short hair.
I liked her better with long hair.
You’re gonna look great.
I don’t know what I’d do.
I don’t know how you do it.
I don’t know how you’re gonna do it.
You are so brave.
You are so strong.
You can do it.
You can beat this.
No matter what anyone says–
It is just going to suck.
Bigtime.
You may shed many tears over this one.
It may be harder than you thought.
I’ve heard brave women say it was harder than the actual chemo.
Reports show women actually turn down the chemotherapy they need because they don’t want to go bald.
It’s real.
It’s hard.
If it weren’t,
Women wouldn’t cover their heads.
They would just walk around bald.
They wouldn’t care.
But hair matters.
To us,
To our kids,
To our husbands,
To our friends.
My hair has never been the same since chemo.
I’m not alone in that.
In fact,
My hair now grows “the other way”…
My part is on the opposite side of my head than it used to be.
I think that’s kind of neat.
There’s the way my hair was B.C. (before cancer)
And the way it is now.
It is a big deal.
Don’t let anyone minimize it.
If they do, make them go shave their heads.
Not just clipper cut.
Straight razor shave it until there’s nothing left.
Then the eyebrows.
Then the eyelashes.
And then the stuff they might not think about.
Every piece of body hair.
Of course there are jokes.
And giggles.
The Brazilian wax done for you.
It’s funny.
But not so funny.
Then when your nose hairs fall out you suddenly realize how
Much you needed them.
Your nose runs constantly.
And it’s embarrassing.
Mine dripped clear liquid constantly.
I was so embarrassed.
No one had told me about that part.
I had a tissue stuffed in every pocket.
Because there were no hairs to stop the drip.
Chemo drip.
You try to imagine what it will be like.
You try to picture what you will look like bald.
You pull your hair back,
Slick it back,
Try a wig on to see what it might look like.
But nothing can prepare you.
For that crappy day,
Two weeks in.
When you scratch an itch
Or touch your head
And take away a handful of hair
Or find it on your pillow.
And the sight of it is so sad,
But so disgusting
So repulsive,
That you need it gone.
And then if you need me
You will call me.
And I will come.
And I will cut it.
Or maybe I will just come and cry with you.
And remember what it felt like.
No matter what anyone says,
It isn’t nothing.
It is something.
And even in the scheme of all of the things to be afraid of with cancer,
How you feel about losing your hair is real.
It matters.
And I remember.
December 8th, 2010 §
Today I was interviewed in The Washington Post about my perspective on the news of Elizabeth Edwards’s death. Melissa Bell’s article is entitled “Elizabeth Edwards and the cancer question.” Click on the title to read the piece on the Post website.
Thanks so much to all of you who read the two pieces I wrote about Ms. Edwards and passed them on to friends:
On Resilience and Why I’m Crying.
Your comments mean so much.

December 7th, 2010 §
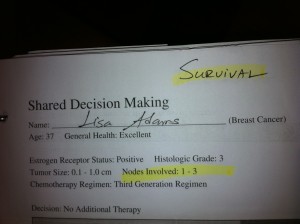 Doctors diagnosed my mother with breast cancer the exact same day Elizabeth Edwards heard those words in November, 2004.
Doctors diagnosed my mother with breast cancer the exact same day Elizabeth Edwards heard those words in November, 2004.
Two years later, I too received a diagnosis of breast cancer.
After my diagnosis I went for consultations with two oncologists. Each doctor handed me two pieces of paper displaying bar graphs of the risk of my cancer returning and the risk that I would die from my cancer. These risks were broken down and calculated for four separate conditions: 1) if I did nothing, 2) if I received chemotherapy, 3) if I received hormonal therapy, and 4) if I received “combined” therapy (chemotherapy + hormonal therapy). On the top of the stark white pieces of paper in my doctor’s writing it says “Survival” on one and “Recurrence” on the other.
I made my decision rather easily: to treat my Stage II cancer I opted for a double mastectomy, chemotherapy, and adjuvant hormonal therapy. I had a husband and three young children; I wasn’t taking any chances– I would do whatever it took to get me into remission and give me the best possible chance of survival.
My mother, because of the particulars of her Stage III cancer opted for a lumpectomy, radiation, and chemotherapy.
And so, my mother and I had different treatment plans. But while our treatment protocols differed, we both required the same character trait to get us through: resilience. Appropriately, this is also the title of Elizabeth Edwards’s book.
Resilience has carried me through my mother’s diagnosis and mine. My son Tristan’s surgeries and treatments for congenital spine and hand deformities. The sudden death of my beloved mother-in-law in a car crash one year ago.
Resilience is the ability to bounce back, the ability to find strength and reserves when you think there are none, the guts to wake up each morning and, knowing something else might be just around the corner, say, “Okay, world, bring it on. I can take it.”
It’s also the manner in which you take it. Do you feel defeated? Resigned? Depressed? Angry? Do you channel those negative emotions into something positive?
Some people believe that negative things like cancer and grief are gifts. Books I’ve seen preach that you should change your thinking: these events are not traumas or tragedies; they are gifts, positive intrusions into your life.
I don’t think so.
I don’t think cancer is a gift.
I don’t think grief is an opportunity.
I think these things suck.
I think they hurt.
There’s a difference between thought and action: what you do with those feelings is what counts.
People don’t need to have the same beliefs or think the same way to feel a magnetic pull to one another.
Resilience is like a magnetic pull to life, a force that keeps me coming back for more
with grit,
determination,
heart,
hope.
Resilience whispers in my ear,
“You can do it.
Just keep going.
One foot in front of the other.
It will get better.
And, if it doesn’t, well…
you can take it.
Bring it on.”
Elizabeth Edwards reached many people because she was in the public eye, but inspirational people also live quiet lives. We can be inspired by Edwards’s grace and courage as she dealt with the challenging parts of her life in the same way we can find inspirational people around us each and every day. These are all people we can connect with and learn from. In doing so, we better ourselves. In doing that, we honor their struggle.
My mother is alive, and in remission. And the joy that I feel about having my own mother here is shared in equal measure by the sorrow I feel for Ms. Edwards’s three living children, Catharine, Emma Claire, and Jack, over the loss of their mother.
December 7th, 2010 §
I didn’t know Elizabeth Edwards. In fact, I wrote a piece critical of her when she initially stood by John after his affair. I was disappointed when she gave an interview on CNN in May of 2009 and spoke only of John’s “imperfection” rather than calling him the cheater he was and kicking him to the curb. I was angry she hadn’t used her interview time to talk about herself, her cancer, her life: the topics I wanted to hear about. I was angry at her for not claiming her remaining years of life as her own.
So why am I sitting with tears in my eyes because she has died?
I cry because it makes me feel vulnerable and scared of what this disease can do to me: what it did to her.
Yes, I know… there are plenty of men and women who get cancer, have treatment, and stay in remission for the rest of their lives. And, in essence, isn’t that what every cancer patient hopes for, as Betty Rollins wrote, “to die of something else”?
I don’t think it makes me pessimistic, depressing, or negative to think that I am vulnerable.
It’s the truth. It’s my truth.
Anyone who hasn’t been to the oncologist with me to see my risk-of-recurrence charts, my mortality charts, my decision-making discussions along the way can’t say to me “Oh, don’t worry, that won’t be you.” No one, including me, knows how it will go.
People tell me: stay strong, just think positive, you can’t generalize from her situation.
I respond: I am strong, I hope for the best. I don’t think positive thinking is going to save me if there are remaining cancer cells still in me.
I hope that people won’t say to someone who has been diagnosed with cancer, “Don’t worry, what happened to Elizabeth Edwards won’t happen to you.” Because while we do everything we can to ensure we die of something else, it just isn’t always the case. In 2006 her oncologist told her that there were many things going on in her life, “but cancer was not one of them.” Things change quickly, cancer can recur when you least expect it.
I have sympathy for her family. I cry for her children. I am saddened about the years she spent with a man who didn’t deserve her. I am angry about the time she wasted on him. I hoped she would be an example of someone who would keep cancer at bay.
I grieve for that hope, now gone.
November 30th, 2010 §
I spent this afternoon at Sloan Kettering meeting with my consulting breast oncologist. I learned a lot of new information about estrogen loss after my surgical menopause two years ago. I’ll write more about what I learned at that meeting in future days.
I had a long trip home from New York City after there was an engine fire on the train I was riding on. Once home, however, I was happy to discover that an interview I gave for a new website on bone health after cancer was published!
 Click here to read the piece.
Click here to read the piece.
November 21st, 2010 §
One of the most destructive emotions in my life is regret. Thankfully, I don’t have many decisions in my life that I would change if I had the chance. But there is one big medical one that I question daily: my decision to have my ovaries removed 18 months ago to put me into menopause and remove/significantly decrease some major hormones from being produced in my body.
In consultation with my oncologist, after chemotherapy was over I decided to take ovarian suppression injections. My period had come back within a few months of chemo ending even though I was in my late 30s. I was not going to have any more children. The tamoxifen I was taking had already started giving me ovarian cysts and I needed numerous ultrasounds to monitor them. Ovarian cancer was always in the back of my mind.
After one year of the injections (in which a thick needle is plunged under the skin of your belly and a small pellet of medication is placed which dissolves slowly over the course of one month) I decided I wasn’t going back; I couldn’t tolerate the questions every month with a menstrual cycle and hormone fluctuations. With my kind of breast cancer (estrogen and progesterone receptor positive), any remaning cancer cells in my body would be “fueled” by these hormones. I wanted to minimize them, and hopefully reduce my chance of cancer recurrence.
And so, after the year of injections I consulted with some surgeons. They felt that the ovary removal (oophorectomy) would be no harder on my body than the injections I’d already been taking. I had laparoscopic surgery in December of 2008 and felt good about the aggressive stance I was taking.
Then my world caved in. Within weeks of the surgery I was depressed. My hormones were bottoming out. Not just the estrogen and progesterone, but other ones the ovaries produce. I was plunged into menopause and all of its agony overnight. My hormone levels went not to the point of a menopausal woman (there are still some hormones present) but as my oncologist told me “of a prepubescent girl.”
I was depressed. I cried constantly. I was still getting over the surgery itself (not exactly the “walk in the park” that had been described to me) and had to miss the family Christmas vacation that year. Clarke and the 2 older kids went to Wyoming while I stayed with Tristan and tried to heal and regroup.
The joint pains started, the bone loss continued, the depression loomed. I had to watch my cholesterol numbers and must take osteoporosis medication after breaking ribs in a fall. I have sexual side effects that can’t be remedied with estrogen creams or pills. In the future I worry about the increased risks of dementia, heart disease and lung cancer without the protective benefits of estrogen.
But worse than any of them, the migraines began. I’d never had them before, but the overnight hormone drop brought them on fast and furious. Up to 15 a month.
It really is “always something.” Each decision is not isolated; everything I do to my body has ramifications and risks. I don’t know if I would have made the same decision if I knew what pain I was bringing on myself. All I know is that fear is a motivator. At the time all I could think about was the cancer. I felt that anything I could do to decrease the chance of my cancer recurring was worth it.
Some days I’m not so sure about that. I believe the doctors I consulted vastly underestimated the effect that this surgery can have. Perhaps as more women electively remove their ovaries if they test positive for the BRCA-1 and 2 genes we will learn more about the effect it has on our bodies (I have tested negative for both of those genes but it is a main reason women opt to have oophorectomies).
There’s no way to know if I made the right decision.
If my cancer stays in remission I will feel better about my decision. But as side effects mount and long-term health issues occur throughout my life because of this surgery and its repercussions, I can’t help but question if my fear may have pushed me too far.
November 21st, 2010 §
Sometimes I think this quality manifests itself in perceived negativity. Every so often, Clarke accuses me of focusing on the negative. I can’t say I think he’s wrong, I just think he’s wrong about what drives the concern.
It’s not that I focus on the negative. I just want to be prepared for whatever I am about to confront—good or bad. Of course, being prepared for bad things is harder. But I’m not even sure that I’m ready for good things to come my way.
Here it is in a nutshell: I have a terrible fear of being unprepared.
I never entered “suitcase parties.” These type of lotteries were popular in college. A business would purchase 2 round trip tickets and donate them to a sorority (or other organization) as part of a fund-raiser. You packed a suitcase and went to the drawing. If they chose your name, you and a guest would leave directly from the party to go to the airport.
The twist was, you had no idea where you would be going. You packed your suitcase and showed up without knowledge of whether you were headed to the Caribbean or Vermont. It could be anything, so you had to pack accordingly.
Sound fun? Not to me. Not appealing—at all. I never entered any of them.
I was always like this. But it really changed in December of 2006. The one time I wasn’t worried I got bitten on the ass. When I went back for my second mammogram I wasn’t concerned– in the least. There was no lump, I had just had a clear mammogram 18 months earlier, I was 37 years old, and I had had multiple benign lumps removed throughout my life. Every time I had needed a lump removed, I had worked myself into a tizzy of fear. And each time I had been proven wrong: the lumps were benign.
So to have vague density issues in one breast a few months after I stopped nursing my third child did not provoke worry in me at all.
So when they kept taking pictures I wasn’t worried. When they did the ultrasound I wasn’t worried. When the technician called in the radiologist to look at the ultrasound images I wasn’t worried. When they took me into a separate “discussion room” I still wasn’t worried.
But then the radiologist said words that scared me… hearing words I wasn’t prepared for was devastating.
It’s as if the words she said weren’t in my vocabulary. And therefore, when I heard what she was telling me… it’s probably cancer… I had no reflex in place to catch me while I fell. Here I was, unprepared in every way to digest the news.
So from then on I was fixated on preparing for what lay ahead. I didn’t want to be unprepared for the biopsy, for the double mastectomy, for the chemo. I walked through the world in a blur for that month while decisions were made. My body shut down and I was anxiety-laden. I knew I needed to get a plan. In getting a plan I would feel more powerful, more in control. And I did. Once my decisions were made about surgery and adjuvant therapy (chemo and long term hormone therapies), I think I became resigned. I needed to know what to expect. I needed to know what I might be able to do to take care of my family and how to carry on during what would likely be one of the toughest physical and emotional challenges of my life.
When my hair started to come out in clumps on the morning of my second round of chemo I went to the garage with my clippers and shaved my head. I needed to take control.
“What ifs” are my lifeblood. What if my cancer comes back? What if I die from this? What if I have such a poor quality of life that it’s not worth it anymore? What if I made a mistake being as aggressive as I have been?
The passage of time is helping me with these questions. I know you can’t control it all. And I don’t have the energy to worry all the time. But I also know that in being prepared I am self-soothing, rubbing my mental worry beads, trying to reassure myself that things will be okay.
I’m not sure I believe that yet. It’s a daily struggle. But I learned my lesson by dropping my guard. As a student of life, I failed once. I won’t do it again. Control what I can, be prepared for what I can’t. That’s as far as I am right now.
 Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).
Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).




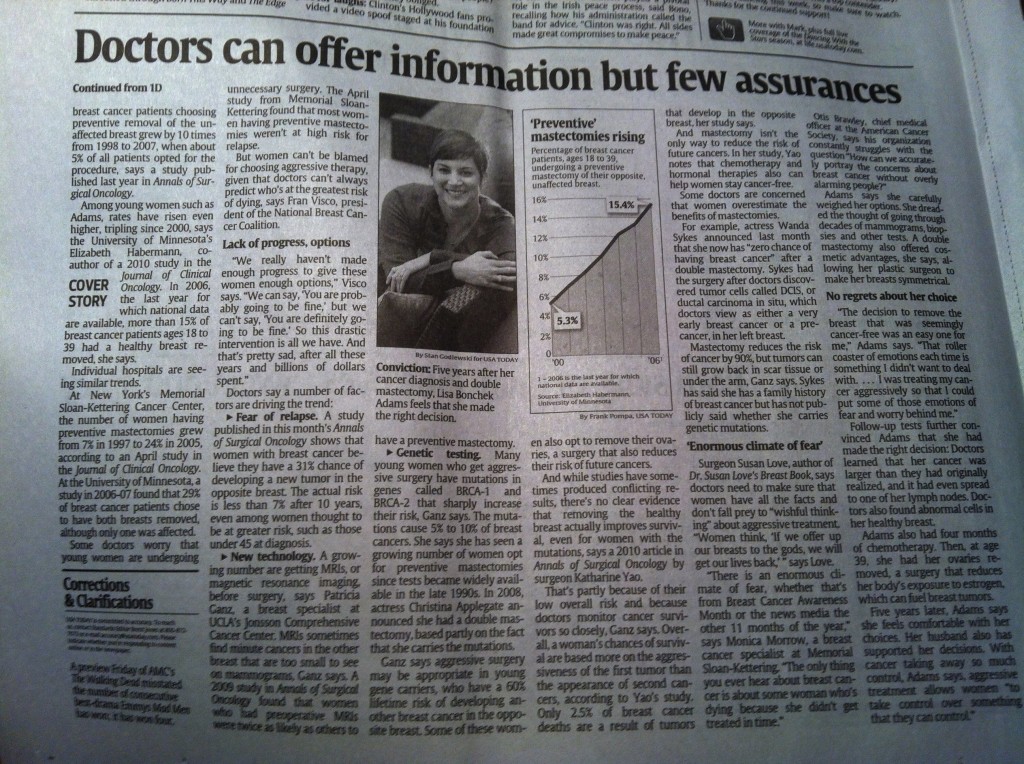



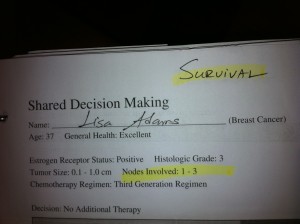

 Link to Twitter
Link to Twitter