April 2nd, 2013 §
 It’s been a wonderful but long few days. I was so run down yesterday that after our egg hunt I got into bed and pretty much didn’t get out for 9 hours. Tristan’s birthday was absolutely delightful. We held a birthday party, something he’s never had before. We’re not big on parties in our family; instead, we always have small family celebrations.
It’s been a wonderful but long few days. I was so run down yesterday that after our egg hunt I got into bed and pretty much didn’t get out for 9 hours. Tristan’s birthday was absolutely delightful. We held a birthday party, something he’s never had before. We’re not big on parties in our family; instead, we always have small family celebrations.
One year, Tristan was at Shriners Hospital for Children on his birthday having hand reconstruction surgery. When the surgeon you want has an opening in his schedule, you don’t say no because it’s your four year-old’s birthday.
When we’ve done parties it’s been my tradition to have a no-presents party. Our children get presents from us and close friends. Party guests, however, are not allowed to bring them (it’s fascinating to me how many people have a difficult time following this rule). Instead, they’re asked to bring the money they would have spent on a gift and donate it to charity (we designate Shriners Hospital for Children). Each party we’ve had in the past has raised at least $500. Paige has had two or three parties through the years, Colin has had two. In those particular years they got the party, cake, and presents from family members. This was more than enough.
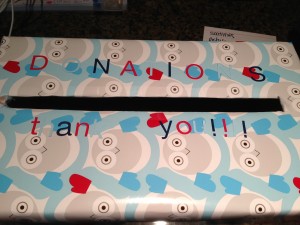 We put a donation box out at the party and everyone can stuff the box. This year Paige wrapped and decorated the shoebox. The children who are bringing the donations also get a lesson in the joy of giving to others. Often the parents tell me that their children don’t understand why they can’t bring a present. That’s okay with me, I think it’s fine to force a discussion about giving to those in need. My children take pride in doing something good, and even when they are young and want to know why guests can’t bring gifts, I feel no guilt in explaining that not all children can afford to pay for the operations they need. When parents say to me, “Oh, I would love to do that but I don’t know how my child would respond,” I never quite understand that. It’s our jobs as parents to be role models, to show our children what’s important.
We put a donation box out at the party and everyone can stuff the box. This year Paige wrapped and decorated the shoebox. The children who are bringing the donations also get a lesson in the joy of giving to others. Often the parents tell me that their children don’t understand why they can’t bring a present. That’s okay with me, I think it’s fine to force a discussion about giving to those in need. My children take pride in doing something good, and even when they are young and want to know why guests can’t bring gifts, I feel no guilt in explaining that not all children can afford to pay for the operations they need. When parents say to me, “Oh, I would love to do that but I don’t know how my child would respond,” I never quite understand that. It’s our jobs as parents to be role models, to show our children what’s important.
When I had my own 40th birthday party a few years ago I did the same thing I have my children do: I asked guests to bring donations to charity in place of a gift. We must be willing to do ourselves what we ask of our children.
Shriners Hospitals provides care regardless of financial situation with an emphasis on orthopaedic care, spinal cord injuries, and burns. Tristan’s complex hand reconstruction helped him tremendously, he was able to have 3 procedures at the same time (a tendon transfer, a z-plasty to widen the web space, and a ligament tightening at the base of his thumb). Should he need cervical fusion surgery for the hemivertebrae and malformations in his neck that is where we will go (I’ve written elsewhere about Tristan’s congenital deformities in his spine and left hand). The team in Philadelphia including Dr. Randal Betz, Dr. Scott Kozin and physician’s assistant extraordinaire Janet Cerrone are very special to us.
 Invitations and stickers from Easton Place Designs and the most adorable cookies from One Tough Cookie helped to make the day special. Tristan loved his karate party, and I love that I’ll be sending a big envelope to Shriners Hospital in Philadelphia from Tristan. I am so grateful to the families who helped to make this birthday so special for Tristan. I thank them on behalf of the children who will benefit from their generosity. Everyone does what’s right for them. This type of birthday celebration is what feels right to me.
Invitations and stickers from Easton Place Designs and the most adorable cookies from One Tough Cookie helped to make the day special. Tristan loved his karate party, and I love that I’ll be sending a big envelope to Shriners Hospital in Philadelphia from Tristan. I am so grateful to the families who helped to make this birthday so special for Tristan. I thank them on behalf of the children who will benefit from their generosity. Everyone does what’s right for them. This type of birthday celebration is what feels right to me.
…………………………………………………….
In case you missed it, Seth Mnookin had a great piece on Slate about the Time magazine cover about cancer. He and I had a great talk about this and I’m quoted briefly in the piece. You can read it here.
** Also, a reminder I’ll be on Doctor Radio (SiriusXM channel 81) this Wednesday, April 3rd at 1 PM EST on the Oncology Show. You can check the schedule here, and it does repeat a few times during the week. I am going to try to get an audio file for those of you interested in listening who won’t have access to it live. The topic? One of the most popular here on the blog: how to talk to people with cancer in a sensitive and caring way.
March 28th, 2013 §
 Limboland is part of stage 4 cancer. On a daily basis I don’t know what’s happening inside my body. I often think about the cancer cells and wonder what they’re doing. Are they dying? Multiplying? It would be so nice to have a reliable blood test to easily and accurately measure how many of them there are at any given time. But these tests do not yet exist for us.
Limboland is part of stage 4 cancer. On a daily basis I don’t know what’s happening inside my body. I often think about the cancer cells and wonder what they’re doing. Are they dying? Multiplying? It would be so nice to have a reliable blood test to easily and accurately measure how many of them there are at any given time. But these tests do not yet exist for us.
My CA 15-3 test again showed a slight elevation from two weeks ago. The numbers have been bouncing around over the last few months (expected) with a slight upward trend (undesirable). It’s hard to know what this means. A few points here and there are not cause for alarm. This volatibility is inherent in this test (which is why some oncologists don’t do this test at all, and why it can’t be used as a screening device. Also, in some people the test doesn’t reflect changes in the amount of cancer present at all). So… it’s a bit to me like trying to juggle Jello.
Of course I want to walk in and have my number be lower than the previous time. But that’s not always possible. With the exception of my hands I’ve felt good for the last two weeks. I’ve been in a frenzy of activity this week with Tristan’s 7th birthday this weekend (more about that in the next few days) and lots of activities with the kids. How I feel is important; while blood tests can show how my counts are, lack of pain in new areas is good too. I received my monthly injection of Xgeva today as well.
I’m back at Sloan Kettering next week and Dr. Dang and I will huddle and strategize. Today my local oncologist and I talked about some ideas about how to treat this test result and what it potentially really means. Right now it seems we are in watchful waiting (not that there is anything new about that). As of today no repeat PET scan is scheduled. We will see if that decision changes next week. My prediction is we wait two more weeks to see where the levels are then and re-evaluate at that time.
Chemo starts this Sunday. I’ve been doing the maximum recommended dose for 5 days, and a slight decreased dose for 2 days. I think this time I’ll be pushing to the maximum dose for all 7 days. It’s hard to know what price I’ll pay for doing so, especially during a very busy week next week (Sloan appointment and then another gig on the Doctor Radio Oncology Show on Wednesday at 1 PM which I hope to attend in person). My hands are my biggest issue, this is just what happens with Hand/Foot Syndrome. I continue to treat my hands with all sorts of products and care, but the truth of the matter is that this is what Xeloda does when it is taken and leaches out of the capillaries. The only true remedy is a decreased dose or discontinuing it altogether. That’s not in the cards right now (thankfully).
It is always hard to hear news that’s not what you want. I’m sure some people would be filled with anxiety and upset after this type of news. I like to give myself a ten minute pity party and then get on with life. If I give myself up to worry and dread for the next two weeks, what have I accomplished besides ruining two precious weeks of my life? Instead I went to the grocery store and stocked my house with food for the long weekend. I came home and played with my new dog (sweet Lucy is especially lovable in times like this).
I am a role model: my children are watching how I handle all of this. Raising polite and kind children is not enough. My children’s mastery of resilience is as important as any other life skill I can teach them. If I become debilitated by anxiety, don’t pick myself up and press forward, I am teaching them a lesson they do not need.
It’s okay to be emotional or upset at bad news. Complete denial serves no one. Acknowledging emotions of anger, sadness and fear but still displaying strength, stamina and persistence is what I try to do.
I hate the turn my life has taken. I hate that this is what is happening to my family and to me. For now, though, I continue to focus on all of the things I can do, and am doing. I pour my heart out on this screen. Some people think I must be depressed all of the time if I have these dark emotions evident in my posts. I can assure you that this is not what I am like all the time. Those feelings exist, and are important. I wouldn’t be human if I didn’t have them. It’s important to get them out not only for my own well-being but also because I know many readers with cancer tell me I’m speaking for them.
So, it’s not what I wanted, but I’m not sounding the alarms. We watch, we wait, we treat. I consciously do the best I can every day. Some days I do better than others. Some days I have a short temper and take my anger at cancer out on my husband or my kids. I’m not perfect. I apologize to them. I tell them I’m trying my best but sometimes it just breaks through. They see that I am human too. I make mistakes.
I draw strength from you all every day. Thank you for your support.
March 22nd, 2013 §
 The moving truck has been in their driveway all day.
The moving truck has been in their driveway all day.
Six year old Tristan came sobbing to my bedroom a little while ago.
“The truck is in their driveway. My best friend is moving. I am so sad. I’m so very sad.”
I brought him into my bed and held him as he cried, hiccuping and shaking and hanging his head.
“I know you are sad,” I told him. “I’m sad they are leaving too.”
I told Tristan that he will still see Alex again before he leaves. He can write Alex a letter before he goes and we’ll be able to call him and even FaceTime him too.
I told Tristan I know it is hard when you have a friend leave you. I explained that what he is feeling means he loves Alex a lot.
I was crying too, tears running down my cheeks onto his shirt. I was crying for his pain over having a friend move away but I confess that’s not all I was crying about.
Tristan doesn’t fully understand why this hurts me so much.
I hurt because I can’t stand the thought of it…
I cannot help but wonder: if this is how he feels when a friend moves away, how will he cope when I go away forever?
I know my family will accept my death. There is no other way. But the fact I have to spend my days thinking about these things tears me apart.
I know the impact of the death of a parent is everlasting.
I know it is something you deal with but never get over.
I hate that I will do this to my children.
I hate that I cannot ever fully have this out of my mind.
I hate cancer.
But I love my family more.
Tristan, I’m doing everything I can to make that horrible day as far from now as I can. I don’t want to die and leave you, or Colin, or Paige, or Daddy, or Nana, or Grandpa, or Uncle Mark. I don’t want to leave my friends. I don’t want this life to end, and certainly not so soon.
But when that day happens and I do die, it is more than just about being what I want.
Not everything is in my control. If it were, we wouldn’t be where we are now. Trust me.
Wanting my life to be long, wishing for it, hoping for it… these things just aren’t enough.
Cell biology and tumor features and available treatments will have more to do with the length of the rest of my life than any wishes or hopes or dreams.
But I’ll still keep those wishes and hopes and dreams, sweetheart, because I won’t give up on you.
March 19th, 2013 §
Alone.
Willing myself to recharge, gather strength, get ready, be stronger.
Chemo starts again.
One more week.
My relationship status with chemo on Facebook would read: It’s complicated.
Chemo keeps me alive.
Buys me time.
Gives me days, weeks, months.
But
Makes me sick.
Causes my hands and feet to numb, get tender, peel, redden, swell, ache, burn, throb.
Tires me, sickens me, weakens me.
How can I hate that which gives me hope?
I check in with friends on Twitter.
I see photos of beautiful people in watercolor places doing things I want to be doing.
I am jealous.
The light hits her hair so perfectly, magically, like a mermaid.
It makes me cry.
I literally weep at the beauty of a friend,
wishing I could be with her,
with them,
anywhere but here.
I had a dream of being at Sirenland.
I set a goal, but it has come and gone, unfulfilled.
I cannot decide if stage IV means I must downsize my dreams or shoot for the moon.
Is there nothing left to lose or simply nothing left?
It is late night in Positano now.
They have done their work for the day.
They have their late European dinner, their drinks, their views of the water shimmering at the base of the hill.
I was supposed to go on a trip there once, coincidentally.
A fifteen year anniversary present and celebration of finishing cancer surgeries and chemo six years ago.
Plans were made, everything was set.
Four days before planned departure, our (then) five year old son’s appendix ruptured.
Nine days of round the clock hospital bedside vigils followed.
No trip. No rebooking. No celebration.
But no regrets at being where our son needed us to be.
Wistful I remain.
Unsure I will see that place now.
I envy those who are there.
I wonder if they know.
How I envy them.
March 18th, 2013 §
Metastatic cancer is an introduction to topsy-turvy world.
Things I once counted down to now I must cheer.
The first time I was diagnosed with breast cancer (stage 2, in December of 2006), I counted my chemo treatments down. “Only 2 more adriamycin/cytoxans to go,” I might say, or “Only 4 Taxols left.”
Now I’m forced to be glad for the chemo rounds.
I started my 12th round of chemo yesterday, on Sunday the 17th. After being sick with a bad cold and stomach virus this week I’m feeling not-quite-ready to start again. I haven’t had enough time to rebound and my side effects are not as reduced as they traditionally have been. My feet and especially my hands are not in great shape and I’m limited as to things I can do. For a few days I had trouble walking. Some days I can’t hold a coffee mug. Most days buttoning and unbuttoning are a lengthy challenge. Typing is sometimes painful as well.
Whereas before I could look forward to the time when chemo would be over, now I must be happy for each round. I must realize that it means another week alive, another week the drugs are working.
Another week to be a wife, mother, friend, daughter.
Another week to write, another week to love.
Another week to hope there is a new treatment brewing.
My milestones used to be measured in how much time I had invested to get through to the other side: putting cancer in the back seat. The goal was successfully completing surgeries and chemo so cancer would be more like background noise rather than an attention-greedy headliner in the spotlight.
But now all of that is backwards. I don’t count down until my treatments are over because they are going to be here for the rest of my life. That’s a hard one to accept some days. There is no “when I’m done with treatment.” Not taking chemo would mean I’ve run out of options or the treatment is worse than the disease. There is no after. There is no “looking forward to being done.” Being done now only means death to me.
This is the way it is.
Everything is upside down.
And that’s how life has felt every day since I was diagnosed with Stage 4 breast cancer.
March 11th, 2013 §
When you’re in it
You can’t see your way out.
Some days the only thing that gets you through is thinking
All the days can’t be this bad.
They will get better.
But what happens when you reach the time when they won’t get better?
It does happen,
Eventually.
Each time you sink in the quicksand
You’re never sure if it’s the last time you’ll be able to get back up.
Pretend each time you will rise.
Just get through this spell.
Imagine it’s just another in a string of bad days
That will be followed by a good day,
Or two.
Or three.
That’s how you get through the days, weeks, months, years…
If you are lucky.
There is no option to me.
There is no alternative.
Up. Forward. Onward.
Even when it hurts.
On the outside.
On the inside.

March 7th, 2013 §
 Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).
Everything changes with a diagnosis of Stage 4 cancer. I don’t really think that’s an overstatement. My relationship with my oncologists has, by nature, changed as well. With stage 4 one of the things that’s especially important is good communication between physician and patient. It always is, but now two of the topics that are imperative to review at each meeting are side effects of medications/chemo and symptoms I’m having (especially pain).
I have always had two oncologists’ input on my treatment since my original diagnosis of stage II breast cancer in December of 2006. Even through the more than five years of remission, I continued meeting with them about my adjuvant therapy.
Immediately after I was diagnosed in October with stage IV my oncologists began talking about finding a balance between length of life and quality of life. These two aspects of my life would have to be constantly juggled. The art of medicine and its role in treating cancer suddenly has become crystal clear while the science of decision-making often remains blurred.
For many people it is often reassuring to hear there is a plan, a prescribed protocol. There is a type of comfort in being diagnosed with a disease and being told there are defined steps you need to take. With metastatic cancer it’s not crystal clear. Patients must often help decide what is right for them.
I was offered options about which treatment to try first: a traditional chemo or an anti-hormonal combination. One would attack cancer cells, but also attack the healthy cells in my body. The other would aim to “starve” the cancer of some of its fuel (hormones). One important positive feature about my cancer is that there are choices about how to try to keep it in check. This hopefully will equate to having stable disease for a while so I can live longer. Some types of cancer do not respond to certain therapies and therefore there are fewer options in treating them.
When I went to see my medical oncologist at Sloan Kettering, this week she pulled the chair over and sat only inches from me. I was on the exam table, in the modest red and peach Seersucker bathrobe Sloan uses for their exam gowns. We sat and talked about research and trials and side effects and my blog and my family. She gets emotional sometimes when we talk about the current situation. So do I.
Then Dr. Chau Dang said something that I will always remember. She said that many doctors start to distance themselves from their patients as the patients get sicker and closer to death. She said this is their coping mechanism. Of course I couldn’t help but wonder if the same process is what is behind some of my friends disappearing and rarely contacting me anymore. Some physicians, she said, seem to back away, needing emotional distance not to be weakened each and every time a patient dies.
In contrast, my doctor feels this is precisely the time in her relationship with her patients to embrace them, bring them close, provide them care and comfort as much as possible. It’s important to remember, she always says, that this isn’t a case, this is a life. A person with friends and families who love them. Death happens for all of us. It’s her role to do what she can to prolong life, and when that can’t be done anymore, it’s important to still care for the person, not just treat the disease.
The nature of the doctor-patient relationship changes over the course of illness. Perhaps nowhere is that truer than in oncology. I’ve always been a partner in my care, it’s the only way I know how to be. It’s my life, after all, and the decisions we make as a team are ones I do not want to regret because I gave up control or didn’t have adequate information. However, I also accept that treating cancer is not an exact science.
Some patients do not want to have options. They want their physician to pick the course of treatment that seems best matched for the patient and proceed. A patient sometimes doesn’t want choices; he or she wants the doctor to do the sifting and prescribing. This works for many people, and takes the responsibility off the patient. There is mental comfort in that approach, too. I can understand why some people make that choice.
One of the things that is difficult in being a true participant in your own care is that while you get the satisfaction of partial control, you also must accept responsibility if/when things go wrong. This is part of the deal.
Some things just are.
Some things just happen, even when you do all you can.
I have accepted this jagged truth all along.
But I think some people never do.
March 5th, 2013 §
Today (Tuesday) I’ll be in New York City having my appointment with my oncologist at Sloan Kettering. I won’t be getting any test results and don’t anticipate making any major changes to my chemo regimen so I do not think there will be news to report. Of course I’ll post an update with any information I find out that might be helpful to others.
Because I have so many new readers I want to just make sure everyone knows that I do not necessarily post every day. A day (or a few days) without a post should not be interpreted as something medically severe. I have always felt it might be overload to be trying to get a post out daily; for now, about three a week seems right. Naturally, life gets in the way sometimes– that’s usually a good thing for me, of course. It’s life getting in the way. School events with my children, home repairs, and doctors’ appointments all can wreak havoc on a writer’s day as any writer will tell you!
I am still working on the post about things that are helpful to say/offer when someone tells you he/she has cancer. This post will take a while for me to work on. Bear with me; I’ll be posting other things in the interim, but that doesn’t mean I’ve forgotten.
I appreciate the support each and every day. Twitter is the best place to keep up with me if you want more daily info (@adamslisa) and there are also Facebook pages as well (one here and one here including the fabulous song/video “We Love You, Lisa” by Neil Shurley).
If you want to receive the blog by email it posts every day at about 11 A.M. EST. You can sign up by entering your email in the box in the upper right corner of the website home page, but be sure to open the first email you receive and confirm your request, otherwise it won’t activate.
March 4th, 2013 §
 Once or twice a week I awaken in the middle of the night with a poem in my head. I reach for my phone and I type frantically. I go back in the morning, or after a few days, and read what I’ve written. I know the words are important, streaming from my head like water breaking through a dam. This poem came from one of these middle-of-the-night sessions.
Once or twice a week I awaken in the middle of the night with a poem in my head. I reach for my phone and I type frantically. I go back in the morning, or after a few days, and read what I’ve written. I know the words are important, streaming from my head like water breaking through a dam. This poem came from one of these middle-of-the-night sessions.
If you let me
If you let me
I’ll cry you a river
Scream at the moon
Hold your hand
Kiss your mouth
Feel your heartbeat
Dream of more
Fear the end
Wish it were different
Pound my fists
Swear a blue streak.
If you let me
I’ll give you strength
Find a reason
Deliver some hope
Take a needle
Feel the pain.
If you let me
I’ll be grateful
Feign bravery
Take a stand
Do my best.
In the end
I’ll whimper softly
Try again
Give a last kiss
Take a last breath
Slip away.
March 2nd, 2013 §
 By now many of you have heard the news that my blog was chosen to be included in the New York Times Motherlode Blogroll. I’m so thrilled that editor KJ Dell’Antonia chose to share my writing with a wider audience. The original web announcement appears here, and the text appears below.
By now many of you have heard the news that my blog was chosen to be included in the New York Times Motherlode Blogroll. I’m so thrilled that editor KJ Dell’Antonia chose to share my writing with a wider audience. The original web announcement appears here, and the text appears below.
It’s exciting to see the readership grow. I’ve been busy reading the emails, tweets, and comments from readers who connect with what I’ve written. The notes of suppport and appeals to “keep doing what I’m doing” cheer me. When someone writes, “you’ve expressed what I’m feeling” or “I’m learning from you” I know that what I’m doing is right. I try to answer emails, even if it’s just a sentence or two, but sometimes I just cannot. Please know I read EVERY word you write to me, if I can’t respond individually all the time, I ask your forgiveness.
If you haven’t read my essay The mentor I never met about my own introduction to a blogger with cancer, please do. It’s one of the most important things I’ve written. It explores the connection between a reader and a blogger. I know there are thousands of you reading these words that don’t know me personally. But that doesn’t matter. I understand how reading a diary of the innermost thoughts of someone facing stage 4 cancer brings us together. My readers here and followers on Twitter understand me in a way that even my close friends cannot. It’s one reason I love social media. There is a connection that can be made (at least the way that I use social media).
I welcome new readers who’ve come here after seeing KJ’s announcement. I treasure the readers who have been with me, encouraging me from the start.
A bit of housekeeping before I turn you over to the Times profile: my bloodwork this week showed stable tumor marker (CA 15-3) numbers. This is good. Side effects from the chemo have varied from annoying/challenging/painful to quite tolerable. This is as much as I can hope for.  I was able to spend a lot of time with my family this week and enjoyed being at school for conferences and a reading celebration of Dr. Seuss’s birthday.
I was able to spend a lot of time with my family this week and enjoyed being at school for conferences and a reading celebration of Dr. Seuss’s birthday.
I will continue with the dosing that I have done for the last two rounds (I’m on round 11). I take 27,000 mg (54 pills) of Xeloda over the course of a week and then have one week off. Before starting the next round I do bloodwork, make any adjustments to the dose based on tolerability of side effects, and repeat the process. I will do this as long as the cancer responds to the drug and does not spread further. I will be on some form of chemotherapy for the rest of my life. 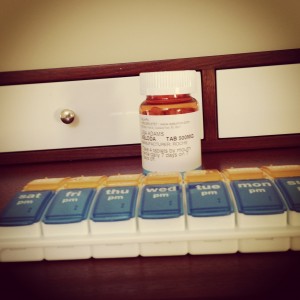
I received my monthly Xgeva injection for my bones which I’ve tolerated much better this month than the Zometa intravenous infusions I was getting since October. Those treatments were giving me difficult side effects.
Thanks to you all for reading. I appreciate all of the warm greetings I’ve had so far.
……………………………………..
Blogging Her Life With Cancer
by KJ Dell/Antonia
When I called on readers to submit the blogs they loved for the Motherlode blogroll, one name came up more than any other: Lisa B. Adams. And I can understand why. The best personal blogs come from people on a journey through something that is as intense as anything they’ve ever experienced, and Lisa is on a journey none of us want to be on. She has breast cancer, and last fall she learned that the cancer had metastasized to her bones, becoming Stage 4 breast cancer.
It’s hard for me not to resort to clichés in talking about Lisa’s blog — to say things like “she’s taking it one day at a time” and “she’s playing the hand she was dealt.” I suspect that those clichés are an excellent way to distance myself from her experience. But it is Lisa’s gift that she does not allow that distance between herself and the reader. She has a directness that draws you in, and she tells her story in a way that is never maudlin. It’s just … her story. It could be anyone’s, but it’s hers, and she’s willing to simply tell us how it is to be her.
I wrote Lisa, and asked her to tell us how her blog began and what it means to her, and to describe a few of her favorite posts.
From Lisa:
I probably started blogging in the reverse order many people do. Rather than it mattering intensely to me and then later realizing it mattered to others, I started by doing it for others and then realized how much it was part of me.
I’ll explain a bit. When you have had cancer and are one of the first ones to have it, you become the reference point as others are diagnosed. “Oh, Lisa had breast cancer… you should talk to her. Do you know her?” This is a natural branching out of social circles based on disease.
As a person who gets asked for advice all the time (most frequently about medical information), I was asked repeatedly for advice about cancer and how to help people who had friends or relatives who were diagnosed. Once I started writing informative pieces to share with them and saw their reactions, I realized I filled a void in the cancer blogging community at that time. As a result, my interactions with readers and the writing process itself became fulfilling in a way that my prior academic work never had.
I strive in my writing not to always focus on cancer per se. A few of my posts are, in fact, technical updates on my condition. These are the posts I like writing the least. I focus on the emotions of cancer … the disease itself is not usually what’s important. Instead, what I try to focus on are the emotions that accompany these hardships: fear, anger, despair, hope, grief, love.
A few of my favorite posts:
“These Things Are Not Tied With a Pink Ribbon” is an emotional reaction to Breast Cancer Awareness Month and details why I think those campaigns don’t relate to me.
“If You Knew Suzy, If You Knew Me” is a reaction piece to the Wall Street Journal reporter Katie Rosman’s book about her mother’s life, “If You Knew Suzy.” This piece is special because it really explores the very reasons why I write. If you want to know why I do what I do, you need only read this piece. I write to be known. I write to be understood. I fear others won’t be able to do that for me, I must do it for myself. In the process, I’ve found that others can learn and grow. I am glad that we all can do that together, even if the circumstances are not the ones I want.
“The Hardest Conversation” (published in The Huffington Post) details a long talk I had with my oldest child (age 14) shortly after I received the news that my cancer had metastasized. I think one of the reasons people like to read my blog is that they want a window into a family where difficult topics are discussed openly and honestly. We are a society which often does not treat children as if they can handle illness, death and tragedy. I believe teaching children coping skills is one of the most important things I can do as a parent. This piece has been one of the most personal and important ones I’ve written.
Some parents feel their job is to protect their children. I believe protection should not equate with hiding information. To me, protecting means educating them how to deal with what the difficult things life hands them.
“To My Dearest Children” talks about some of the joys of parenting and explains to them that being their mom is the best thing I’ve ever done. It’s the one job I haven’t quit, and the role I think I do best.
You can find Lisa’s blog here, and soon on the Motherlode blogroll, which will appear in the sidebar just as soon as I’ve welcomed a few more blogs. That main blogroll will be short, strong and as broad as I can make it. We’ll also be adding a page of resources — blogs and other sites you can look to for specific topics or to find some new reads. I’ll keep that as current as possible — so if you ever click through to a dead or abandoned blog, let me know.
February 27th, 2013 §
There are always eyebrow-raising things people say to those with cancer and/or their families. Maybe not everyone would find each of the comments listed below to be offensive but they’ve been submitted by readers as ones they wish they hadn’t heard. I like to revisit this topic every so often to allow people to post comments and add to the list. Some of these come from the comments the last time I discussed this topic (
here).
At the bottom you will find a link to the post I did on suggestions about what TO say and how to help a friend with cancer or other illness.
I’m not going to respond to each of the statements below. I’m just going to list them for your consideration. Some are just strange. Some miss the mark. Some are downright rude.
They weren’t all said to me, but they were said. Gee, that almost makes me want to have an award for the most offensive one listed below…
**please make sure to see the link in red at the bottom of the page for a post of things that are recommendations of what to say
……………………………………………………………
“It will all be okay, I just know it.”
“Someday you will put this all behind you” (to a stage IV patient)
“Don’t worry, things will get better.” (to a stage IV patient)
“So when will you be all better?” (to a stage IV patient)
“When will your cancer be gone?” (to a stage IV)
“But you don’t look sick.”
“Lance Armstrong cured his stage IV cancer. You can too.”
“But I thought you had chemo and surgery last time. How could it be back? This is why people shouldn’t do chemo.”
“Do you think it was a waste to do chemo last time?”
“Live in the moment.” “Be strong.” “Fight hard.” “Keep your chin up.” “Don’t give up.” “Attitude is everything.”
“We just need a miracle for you.”
“If anyone can beat this, you can.”
After telling someone I had stage IV: “Wow. I’m going to miss you.”
“Is it terminal?”
“What’s your prognosis?”
“It could be worse, you know.”
“Everything happens for a reason.”
“It’s all part of a larger plan.”
“You’re only given what you can handle.”
“All you need to do is think positive.”
“Half the battle is the mindset. Be determined to beat cancer and you will.”
“Now that you’ve been through this you’re due for some good things to happen.”
“I’m sure it’s fine/I’m sure it’s nothing.”
“Well, you’ve been needing a vacation for a while and now [during chemo] you get to lie around and read books all day. What could be better?”
“Well, do they think [the chemo] is going to do any good?”
“At least it’s not on your face where everyone could see the scars, besides you don’t really need your breasts anyway.”
“A new-agey friend asked me if I had been really angry about anything 7 years before my diagnosis that I had repressed. (What had I done to cause my DCIS?)”
“I was advised to write a letter to my husband detailing how much I loved him so he could have something when I died. [My husband] was standing next to me as I was being given this little chestnut.”
“One said to me the day after my malignant melanoma diagnosis: ‘Maybe this will help you evaluate all the things you need to change in your life.’ ”
“Last year I had part of my cervix removed surgically for PRE-cancerous cell growth. I was at home recovering from surgery and still had days to await the results of whether or not I had clear margins, etc. Those days that drag on and you just wonder and hope. My mother in law came over with dinner (nice) and then proceeded to stand there and tell me about every person she knew with cancer, how they died, and how their families went on.”
“When my mother was diagnosed with breast cancer, I was a wreck. My (now ex) husband got tired of it really fast and made a rule to confine my sadness to one day per week: “you are only allowed to cry about this on Fridays.” If I felt like I absolutely had to cry Sat-Thur, I had to do it in private.”
“The worst thing said to me was right before I was to have a new lump checked out. I was a 7 yr breast cancer survivor at the time, with 3 children ranging from 14-8 yrs old. When I told a pastor’s wife I was worried about the lump, but was most worried about my children if I got bad news, she responded, ‘Oh, they will get over it. You’d be surprised how quickly. I know I got over my dad dying in a year, and I was about their age.’ ”
“Gosh, I thought chemo was supposed to make you lose weight”
“Nearly every person I told about my mother’s death felt the need to tell me about some relative of theirs that had passed away and how awful their death was.”
“The very stupidest thing was said to me recently, a few months after treatment ended for a recurrrence. I was out to eat with my youngest son, now 16, and ran into an acquaintance. She said she’d given it a lot of thought, and wanted me to know that there were “perks” to dying at early age, in case I did. I’m 47. (and feeling fine by the way, and had just told her so.) But she proceeded to tell me 3 of “the perks” if I were to die early. One “perk” was that I wouldn’t be the grieving spouse, another was that I had already parented “through the fun years” and wouldn’t have to see my kids make bad life choices, and the other one….oh, I wouldn’t have the aches n pains that came with old age like she was experiencing. She was “sincere” and had “thought about it,” and is a nurse!! Just blew my mind.”
1. Random stranger on the street: Do you have cancer? Me: Yes. RS: How long do you have? Me: –
2. On telling peripheral people (e.g. hairdresser, or friend of a friend) of my diagnosis, they proceed to tell you that their uncle/cousin/friend’s mother had cancer and then that they died. I guess they are trying to make a connection and it’s the first thing that pops into their head, but I really did not want to hear about death at that time.
3. An email from a friend of a friend (a homeopath) telling me that breast cancer is caused my a negative relationship with your own mother. This is definitely not the case!
4. People asking me if I knew how I got my cancer (and then offering me something to read about some “natural” therapy they have heard about or are selling).
5. I fully got sick of hearing the words “positive” and “strong”; so much so that I banned my family and friends from saying them.
“People choose their sicknesses. He chose to have cancer by not managing his negative energy and he chose to die by not fighting.”
“Someone I know has pancreatic cancer. She didn’t suffer too many adverse effects throughout chemo which was fortunate for her. Her daughter, who knows I went through chemo all a year earlier, made a comment that her mother must have a particularly strong constitution because she didn’t have trouble with side effects. Ya, unlike like the rest of us weak wussies who who were knocked out by chemo! I knew that she was grasping at any tiny sign that her mom might experience a full recovery so I kept my mouth shut.”
………………………………………………….
So what DO you say? A post with suggestions for what to say/do appears here: “What to say to someone with cancer/how to be a friend to someone with a serious illness.”
February 26th, 2013 §
The months and years go by. Like all of you, I mourn the quick passage of time. “Where did the school year go?” I hear my friends asking.
Projects we hoped would be accomplished — tasks we hoped would be done — sit unfinished. Organizing photos, cleaning out a closet or a room, reading that book a friend recommended— many things went undone in the dark and cold months of winter.
Maybe there were emergencies, maybe there were health issues, maybe you just couldn’t get the energy together to accomplish everything you wanted.
Regardless the reason, there can be a bit of disappointment when a season ends.
Growth happens in fits and spurts, not with smooth, sliding grace.
With each phase comes
pain,
discomfort,
unease,
restlessness,
sleeplessness,
yearning.
At the time of my mastectomies my reconstructive surgeon placed tissue expanders in my chest. These were temporary bags of saline that would be slowly filled to stretch out my skin to make room for the silicone implants that would eventually take their place. Each week, like clockwork, I returned to my surgeon’s office. He accessed a port in each expander with a needle, and added saline to each side to make it bigger.
Each time after a “fill” my chest would feel tight. The skin wasn’t big enough for the volume inside, and it would react to the increased pressure by stretching. Until the skin could replicate there was achiness, tightness, a slight ripping or tearing feeling.
A similar sensation happened to me during my pregnancies; the growth happened fast, I got stretch marks. I had visible proof my skin just couldn’t keep up: the growth was too rapid, too harsh, too vigorous.
I often wonder if mothers and fathers get psychological stretch marks when we are asked to accommodate changes we’re not quite ready for.
What can we do? What options do we have? None. We must “go with the flow” and do the best we can. Our children grow and change whether we like it or not.
We do them no favors by trying to protect them, coddle them, and keep them young.
We give them wings to fly when we give them tools to be
confident
and caring
and inquisitive
and trusting
individuals.
I am often moved to tears as I watch my children grow.
I sit in wonder at the succession of infancy, childhood, and adolescence.
I know that as a mother I lack many skills, but I also know that the words I have written in my blogs and essays will one day be a gift to them tooNot a gift to the children that they are, but instead a gift to the adults that I am raising them to be.
Each June as the school year ends I marvel that another academic year has passed.
The growth happens too fast.
The growing pains hurt.
The stretch marks might be invisible, but they are surely there.
February 21st, 2013 §
 “I look so old in that picture.”
“I look so old in that picture.”
I hear this one a lot now that my friends and I are what they term “middle-aged.” They want to see and choose pictures before they get saved or shared; the confidence and carefree attitude in photos from our youth has slipped away.
It’s not just people my age, though. For example, my father in his 70s comments on how old he appears in photos I take, too. With a full head of white-gray hair, he doesn’t look old, I think… but even if he does? What’s wrong with looking his age? With plastic surgery and Hollywood showing altered appearances all the time it’s almost shocking when we see people who haven’t adjusted their appearance. Maggie Smith (most recently of Downton Abbey fame) has a face as wrinkled as a Shar-Pei, and we love her for it.
Aging isn’t easy. There are cruel sides: bodies that hurt, diseases like Alzheimer’s that strike mercilessly, loss of independence and body control. For sure, I don’t mean to imply that getting old is pleasant.
Aging is, however, the price one pays for living.
I look at getting old as a positive now. To age means to be alive. For some of us getting old is now a pipe dream. I will miss an entire generation of my life. That is the truth about my stage IV breast cancer.
I face the reality that I am not middle aged. I am living my own old age now, in my 40s.
February 15th, 2013 §
 When I was diagnosed with Stage 4 breast cancer last October I could not envision the future. I wasn’t sure if I even had one. Or if I did, for how long.
When I was diagnosed with Stage 4 breast cancer last October I could not envision the future. I wasn’t sure if I even had one. Or if I did, for how long.
It has been four months now. Some people don’t even get four months after a Stage 4 diagnosis. But I am here. And my cancer is responding.
Last October I wouldn’t let myself think about Spring. Or Summer. Or a three year renewal on a magazine. I’d wonder if I would outlive the expiration date on the can of food I’d put in my grocery cart. I renewed my son’s USTA membership for 10 years and hoped fervently it would be my job to renew it in a decade, not Clarke’s. I wondered if I’d see out the rest of my car lease. I just didn’t know what to expect.
In some ways I still don’t. My future is unknown. But that is good, I’m coming to think.
When I go to an appointment with my oncologist and he isn’t changing anything, telling me it’s time to try a different treatment, or handing me a piece of paper with a list of scans, I am happy.
On Thursday I had my usual 2 week appointment with my local oncologist. My tumor markers were down 7 points, erasing the blips up I’ve had lately. The tests are not precise. 7 points doesn’t correlate to a particular reduction, but it’s good news. It means I can continue with my current chemo. I did increase my dose this round and will repeat that again this time. We are hoping to find the “sweet spot” where I get therapeutic efficacy but still have manageable side effects. That’s the goal.
My oncologist talked about another goal for me today. We both know for now these two week intervals are needed. But one goal he would love to achieve is even more stability with my body’s response so that I can have longer stretches of time between appointments. Having bloodwork, checkups and my monthly bone drug (Xgeva) all at once would be grand.
When he told me my results I said, “that’s a two week reprieve.” He said he wants me to be able to think in longer increments. I’d love that too. I’m thinking about seasons now.
Spring.
Summer.
Autumn.
Next winter.
Beyond.
Let’s go for it. Let’s make plans. Let’s see what happens. Together.
February 11th, 2013 §
The finish line is the goal.
Runners strap on shoes, push their bodies, train for months.
Do it well. Do it faster. Faster than the others.
Laps around the track, tires squealing, pit stops along the way.
Checkerboad flags, shake the champagne.
Biking stages, climb the hills, pass the others, wear the gold jersey.
You got there first.
You won.
But I do not want the finish line.
I do not want to get there first.
I am dragging my feet.
Digging in my heels.
Fingertips grasping,
Losing touch,
Don’t make me go.
I’m fighting, crawling, resisting, doing everything I can.
Make the time slow down,
Make the days longer,
Make the end out of my sight.
I don’t want to be the first to the finish line.
I want to be last.
This time, losing would be winning.
February 5th, 2013 §
Today’s brand new post is over at Huffington Post. You can click here to read it: The Hardest Conversation.
This piece is about the conversation I had with Paige after my diagnosis in October of Stage 4 breast cancer. As the oldest of my three children, she has many questions that the younger children don’t. I wrote the piece back in October but kept it to myself.
I waited until I felt she was ready to read it and give her approval before I published it. I would not publish a piece like this without her permission. She said, “You should publish that, Mama.” I think she knows it might help someone else. We both hope it will.
I’ll be back with an update in a day or two. I’m back on an increased dose of chemo this week and did try switching to the new bone=strengthening drug.
Thanks for all of your comments, emails, and support!
February 4th, 2013 §
I awaken to the sound of the snowplow scraping,
Metal on asphalt, grotesque.
I didn’t move last night.
Soft bedding, peaceful house, drained body.
I lay in bed not wanting to start the day.
Friends will gather,
We will share and learn and grow.
But before we do,
when we eat,
I know I must dive headlong into the abyss.
My breakfast will come with a side dish of chemo,
A higher dose than last time.
It’s time to begin again.
Back to reality some will say when we part.
I never left it behind.
February 1st, 2013 §
I’m re-posting this piece quite simply because I find that when I re-read my pieces I find something new in them each time. Maybe readers will, too. Even though it was only written in November, I find it interesting to look back on what my mindset was then, only weeks of learning about my cancer metastases. The idea for the post below came from re-reading A bookmarked life. The idea that there are consistency, permanence, and predictability in the world is a mantra we simultaneously embrace and need while also knowing it’s patently a falsehood… everything is always changing, it just depends by how much.
……………………………………….
Each day is different. Each moment, too.
It still seems surreal, this diagnosis of metastatic breast cancer.
It’s strange how quickly the horrific can become regular: the chemo, the side effects, the new routines.
Oncology appointments, I.V. infusions, medication refills all start to fill my calendar.
I start making lists of things I need to do. I prioritize them.
It’s not always about what’s actually the most important, it’s also about finding things that bring me small moments of joy.
The small moments are the ones that bring tears to my eyes. Tristan’s little voice saying, “I love you, Mama. You’re the best Mama in the whole wide world” is enough to make me misty.
I still lose my temper. I still yell sometimes. Often it’s misplaced anger, a manifestation of my frustration with my situation.
I haven’t suddenly turned into the world’s most patient person. Sometimes cancer makes me the most impatient one, in fact. I feel the clock is ticking. I don’t have time for nonsense. But that’s not a way to be. I will still try to be better.
I try to be the one to do things with my children as much as I can. Even if there is a babysitter in the house Tristan always reads to me at night for his homework: that is sacred. I still save artwork and photographs and remind them to brush their teeth and clean their rooms.
I try to do the little things: helping Colin with a school project, keeping Paige company while she does homework, watching a sports practice if I can. I go to the grocery store and I work on the holiday card. I still take pleasure in getting the stubborn stain out of Clarke’s dress shirt that the dry cleaner couldn’t.
My motto is that I will do as much as I can for as long as I can.
I don’t ever have a moment that I forget about my cancer. I think that’s the part about it being new. Even when I was diagnosed the first time — even after I finished chemo and surgery and all of it– it still took at least a year for me to be able to push the daily fear down. Of course now the fear has been realized. I am living it. I am living my nightmare, one many people share.
And yet, the morning comes.
I see the light of day and I get out of bed. I see the faces of my children. I kiss my husband goodbye when he leaves for work. Each day I have is a day that matters. Each day is one to make a memory with my family and friends.
Each day is one more than I had the day before.
But let’s be clear: there is no joy in this disease.
My appreciation for my days should not be interpreted as supporting the nonsensical idea that “cancer is a gift.” There is nothing positive about this disease; I would give it back if I could. I did not need cancer to show me the value of things. I always knew these things were true. I never took them for granted. I knew what demons could be lurking.
I did all I could. It was not enough to keep it at bay. But maybe, just maybe, I can keep it at bay for a while.
I still haven’t fully come to terms with what this diagnosis means, but that’s because there’s no real way to know. We don’t know enough yet. It is the uncertainty that is the most difficult part for me. Will this chemo be the one that lasts for a while? Will it fail? When? What next? How long with that one last? My body holds the answers, but it’s not showing its hand yet.
I have to learn to ride this roller coaster. I’m just not there yet. And I don’t really know how long that is going to take.
I walk past people on the street and know they have no idea what is going on inside my body.
People in front of me in line at the gas station don’t know there’s chemo in my purse.
I look like everyone else. I have hair on my head. I ask the checkout person to pack the bags light because I can’t carry anything with my left arm now (the cancer has fractured two ribs on my left side).
Sometimes I want special treatment. I want a Get Out of Jail Free card. Most of the time, however, I want to stay home. Hide out. Be invisible.
I’m still processing. Reeling. But while I’m doing that I’m living.
January 31st, 2013 §
I always think these updates must be boring to read. I know they’re necessary, and important. I know this is how most of you get the nitty gritty details on my treatment. Somehow, though, I always wonder if they are actually educational or if they are too technical. So, that’s why I try to limit them to about once a week or when there are changes. My goal is to show you how these decisions get made (in my case only). Some cancers have very specific and formulaic treatment schedules. Metastatic disease often does not. It’s unclear which drug(s) will work and for how long. It’s never known how a patient will tolerate the drug initially and cumulatively as time goes on. The patient has a lot of leeway in many of these cases. There is no blueprint. A good team has communication about options and constantly revises their strategy.
I had this week “off” from chemo. The last few days I’ve felt very good. I have been spending lots of time with our new dog, Lucy, who has brought joy into our home in so many ways. We just adore her.
I was at Sloan Kettering last week and today I met with my local oncologist. Fortunately everyone in agreement after a review of all of the options. One of the things that’s always a concern is quality of life. My doctors are very keen on making sure I am comfortable and able to do things I enjoy. The balancing act of aggressive treatment to extend life without sacrificing too much quality of life is an integral part of treating metastatic cancer. There is no cure. But the goal is holding off the inevitable as long as possible.
I’ve had lingering trouble with the monthly IV bone drug Zometa. Some readers suggested I ask about the other available drug Xgeva, a subcutaneous injection also given once a month. They anecdotally reported fewer side effects. Both of my doctors do not believe Xgeva actually is better for my needs cancer-wise than Zometa, but also agree it’s not worse. One option was to try an IV steroid infusion of Decadron immediately prior to the Zometa to see if it helped with side effects. The other option was to try to the Xgeva and see if I had any side effects from that (most people report fewer to no problems with it, though most also do not have problems with Zometa after the first one or two times). I’ve opted to try the Xgeva. I would usually have gotten it today (28 day interval) but I have plans this weekend that are very important to me. I don’t want to risk being ill and having to cancel. It will not be a problem to get the injection on Monday, so I will postpone it for a few days. We’ll see how I tolerate the Xgeva shot and go from there.
My tumor marker number stayed relatively constant after that small increase two weeks ago. This is good, but leaves us in a bit of a quandary. We aren’t yet at the point of doing a repeat PET scan. The rise is not enough to warrant that, though we will do it soon. Neither is the increase enough to assume the chemo has stopped working after initially being responsive. We don’t know, as I said in the last update, if it’s an anomaly or a trend. The only things that can show us are more data points. I happen to like data points. I like seeing what happens every 2 weeks even if it means more of an emotional rollercoaster. We are only 4 months into this and I don’t feel that we have a handle on how I’m responding yet. Only time can shed light on that. I did have a good initial reaction to the drug which was encouraging.
So… since we’ve achieved a good decrease in the last 4 months with the Xeloda but now that is slowing down and I seem to have “bottomed out” on its efficacy, what now? We want to keep everything where it is. If we can get more of a decrease, that’s the best. If not, we need it to hold steady. We all agree it’s time to try again to increase the chemotherapy dose and see if I can both tolerate it and get a stronger marker response. I started at 8 pills a day in the beginning (for about 2 months) and had to decrease about two months ago to 7 pills a day when side effects became intolerable.
It’s time to walk into the fire again. There is no manual for how to do this. We all brainstorm, we talk about what my goals are, we talk about what makes scientific sense. The idea this time is to increase, but not go back to the 8 pills for the whole round. Instead, to try to get more chemo in my system, I will alternate 7 and 8 pills for the week. We’ll see how I do. Debilitating nausea, stomach pain, hand/foot syndrome, and migraines have been my issues with this drug in the last month.
Also, I will change my start day. Thursday night was my usual. Lately, however, I’ve felt rotten on the weekends (both weekends this time around, as effects often last into day 10 or 11 which technically are “off” days for me). I will now start chemo on Saturday night or Sunday morning and see if we can shift my “rotten days” to weekdays instead. I want more quality days with my family on weekends if I can get it.
This is all educated guesswork, a constant dance of drugs and schedules and side effects and efficacy.
There is no manual.
There is no “must.”
There is only me, floating away, trying to grasp the fingertips of treatment and hope.
January 29th, 2013 §
I wish I had been more accepting of help in the early days when I was first diagnosed with breast cancer in 2006. I wish I had not seen it as a personal “weakness” the way that I express in this piece. I don’t want to change what I wrote then, but I do want to say that I don’t think I was right to push myself so hard. If I had it to do over again I would accept help more often– maybe not for the hair-washing, but definitely for other tasks that I should have outsourced. I have learned from my experience and I now try to graciously accept help when it is needed.
………………………………….
One of my favorite romantic movie moments occurs between Denys (Robert Redford) and Karen (Meryl Streep) in the movie Out of Africa. The two lovers are out in the African desert at a fireside camp. Karen leans her head back into Denys’s hands. He washes her hair gently, then cradles her head in one hand and pours water from a pitcher, slowly and gently rinsing the soap from her hair after he’s done washing it. It’s a tender moment, to me utterly soft and sensual.
Before I left the hospital after I had a double mastectomy, the staff told me I might not be able to lift my arms over my head. With both sides affected, they said, I’d likely be unable to wash my own hair.
Recovery is slow in the week after surgery. A clear thin tube (like aquarium tubing) is literally sewn into a small hole in the skin under each arm. It carries excess fluid away from the mastectomy site as it heals. Fluid is collected into a small “bulb” and measured every few hours. After certain medical criteria are met, the drains are removed, the incisions sewn up, and then you can finally take that longed-for shower. Eight days after the surgery I received the all-clear. As any mastectomy patient will tell you, the day you get your drain(s) out is a great day.
Only then did I try to lift my arms. And hurt it did. I tried to shrink down into my body. I tried to be a tortoise withdrawing my head back inside my shell, shortening my height so I wouldn’t have to lift my hands so high to reach my hair. It was a painful challenge. I worked up a sweat trying to get my fingers to touch my scalp. I knew it was a questionable proposition. But I thought I could do it.
I thought about that scene— that romantic tender scene from Out of Africa. And I started laughing. I laughed and I laughed and tears came down my face. That cry hurt. It was one of those “I’m laughing and I’m crying and I’m not sure if it’s funny or sad or both and I don’t want to think about it so I’ll just go with it and I hope I’m not on Candid Camera right now…”
I was laughing at the absurdity of it. Here I was. It was my chance to get Clarke to wash my hair. My big fantasy moment. I was going to be Meryl Streep and he was going to be Robert Redford and he was going to wash my hair. Except I couldn’t move without pain. And I certainly wasn’t feeling romantic. I had just had my breasts removed. And I had these weird temporary breasts (tissue expanders) in their place. And my chest was numb. And my underarms hurt from having tubes in them for a week.
Because I hadn’t properly showered I still had purple Sharpie hieroglyphics all over my chest. And I had no nipples. And I had big scars and stitches in place of each breast. And a small angry scar with stitches under each armpit where the drain had just been removed. Let me tell you… this was clearly not how I envisioned beckoning my loving husband to come make my little movie scene a reality.
Now, don’t get me wrong. Had I called him from the other room, he would have done it in a second. He would have been there for me, washed my hair, and not made me feel the bizarre, odiferous (!) freak I felt at that moment. And I would have loved him for it. But I did not want him to see me like that.
In that moment I had a dilemma. What kind of woman was I going to be?
What kind of person was I going to be with this disease from that moment going forward?
I was going to push myself. Do it myself.
I wasn’t going to be taken care of if I could help it. I knew I was going to have trouble asking for help, have trouble accepting help. I knew these things were going to be necessary. But I also knew they were going to cause me problems. That’s the kind of person I am.
I knew asking for and accepting help were actually going to make me feel weaker than I was already feeling. And it was only the beginning. I knew these actions were going to make me feel weaker than I knew I was going to get. I wanted to do everything myself for as long as I could.
That was what was going to make me feel alive: doing it myself.
I am not sure I did the best job washing my hair. I probably missed a spot or two. But I did it. And I didn’t ask for help.
Granted, it was something small.
But in that particular moment, on that particular day, that particular act gave me a feeling of pride as big as anything else I could have possibly accomplished.
January 28th, 2013 §
I wrote this only a few months ago, but I am reposting it because it strikes at the core of what I feel so often. So many people responded to this piece saying that whether because of cancer or some other medical/life experience they could relate. Sometimes feelings like loneliness can be the hardest to describe.
…………………………..
I can see how isolating metastatic cancer can be already.
It has become hard for me to be around other people.
I find myself hiding as much as possible.
When I am in the company of others my mind wanders.
I can’t focus. I feel the need to retreat.
For the time being I just can’t relate to others’ lives which only weeks ago were so similar to my own. Now… we are a world apart.
It’s not their fault. It’s just that circumstances make it so that I am selfish. I try to conserve my energy as much as I can.
Already I can see relationships suffering. There is a fine line between giving space and putting distance. Some are already dropping away, and we’ve only just begun. Others have risen to the occasion and helped more than I could have dreamed. Only true friendships are going to make it under these circumstances. Sometimes the isolation comes from being shut out. Sometimes it comes from locking yourself away.
Phone calls go unanswered, emails often do too. Thank you notes don’t always get written, social commitments get canceled or never scheduled in the first place.
I know that people cannot truly understand.
I don’t want a support group right now because metastatic cancer has a wide range of outcomes. I don’t know if I will be in a rapidly progressing group or not. I don’t know whom to look to that is “like me.” There is no way to know which group I will be in, who my peers are.
Right now I am very sensitive to death, to pain, to suffering. It’s very hard for me to see right now. I’m too raw. I just don’t think I’m ready for a group. But I won’t say I never will be.
It’s difficult to listen to people complain about trivial things, normal things, things I was complaining about just months ago.
Now those complaints just annoy me, or make me sad.
I want to scream, “I want your problems!” And I do. I want that life back. I want to turn back the clock. I just don’t want it to be this right now.
One of the things that bothers me the most about this disease is the knowledge that the way I feel right now is the best I will ever feel for the rest of my life. It’s only going to stay the same or get worse. That thought terrifies me.
When you feel crappy you want the time to go faster. You just want to get through it.
The problem is that what you may not have is time.
It’s a conundrum. You want the time to pass, but this is the only time you have.
I know so many people say, “No one ever knows how much time they have. You have to make the most of every day, of every moment.” I know that’s true. But the knowledge that there is something identifiable in your body that is a threat, is most likely to be that which kills you, bears a different weight. Of course the doctors don’t know exactly how much time it will be. There is no crystal ball.
Everyone tells me the stories of friends and relatives who were told they only had months and years later they are still alive and doing okay. I am told these stories every single day. I get it. I do. And I love them, they give me hope. But often those people’s diagnoses and particulars bear no relation to mine.
Additionally, there are also stories of the people in the other group, the ones who thought they had years and didn’t. People probably have the good sense not to tell me those stories. But they are out there. It’s not that I focus on the negative. It’s not that I necessarily think I will be in that group. But anything is possible. On both sides.
The part that scares me: I’m only at the beginning. I hope that I will get stronger, gain acceptance as I get used to this diagnosis. But I’m not sure about that. I truly believe I could handle this better if I didn’t have so much worry about my children and what effect this will have on them. I wish I could protect them, shield them from this agony.
There are good days and bad days. I must do my best. But being the one everyone is watching takes a toll. Everyone will take their cues from me. I will set the stage for how my friends and family will deal with this: how I handle metastatic cancer matters. I am laying groundwork. I feel I must do it right.
Some days that is an overwhelming task.
“Doing it right” doesn’t mean I have to be positive all the time. Doing it right means I have to be honest. It means I get up each day and do the best I can. For myself, for my husband, for my children, for others who may have cancer and those who will get it. It’s okay to be scared, and angry, and sad, and everything else.
It’s all part of this.
And for me, so is sharing.
January 27th, 2013 §
My brother Mark has kindly edited out all of the lead-ins and station breaks and created a permanent link to the show. It’s about 40 minutes long. I really enjoyed talking to the hosts and hope they will keep their word and have me back; there were so many subjects we didn’t even touch on.
Click here to download the podcast.
January 27th, 2013 §
I almost stole it: the tape measure with the purple finger prints.
After all, my surgeon had left it in my room by accident. After he had marked me with his purple pen and left my room on his way to get ready for my surgery, he left it sitting on the counter by the sink. In my nervousness and tranquilized haze I didn’t see it until after he’d left. I figured I shouldn’t hold onto it as I was wheeled in (“Who knows what germs lurk in tape measures!” I thought), and that if I gave it to a nurse it might get misplaced. So I shoved it in my bag of personal belongings knowing I’d be in for an office visit shortly after surgery.
I actually forgot about it during the days I was home after my two-day hospital stay. The drugs, the pain, the shock of my breasts gone and numb chest filled with temporary tissue expanders were all I could think about.
I forgot all about it as I was shuttled around for weeks unable to drive. I wasn’t living my normal life, my normal routine. I wasn’t carrying my purse and keys daily. I was living in pajamas and constantly trying to adjust to a new body once the drains were removed.
Then while I was looking for my keys a few weeks after my operation I saw it: the tape measure.
The yellow fabric one with the purple fingerprints up and down its sides.
The one.
The one that had measured and determined where my body was to be cut.
It was there in my bag.
There wasn’t anything particularly special about its practicality; it was just a tape measure.
Just like the ones I have sitting around with all of the odds and ends that inhabit kitchen drawers.
But that doesn’t capture the social meaning of it.
It wasn’t just any tape measure. It was mine.
But it wasn’t just mine, I argued with myself—it wasn’t a personal momento for me.
For a moment or two I wanted it.
I needed it,
as if to remind myself what had been,
of what I had been.
It wasn’t mine, I thought– it was his.
But more than that, it was theirs; it was ours… the other women who had needed it.
Now I was one of them. It was a shared history we had: strangers who had endured the same surgery, whose faces and names I would not know.
We were bound together by this object which had literally touched all of us.
And then I realized it was my responsibility to give it back.
Not for the obvious reason that it didn’t belong to me.
But as usual, I thought of the other women: the ones who didn’t even know they had cancer,
the ones who were going about their normal lives that day, and in the days ahead, only days or weeks or months from learning the life-altering news that would change their lives.
I felt giving back the tape measure would be my way of being bound to them, of saying “I know what you have ahead of you. I have come from there, and we are in it together.”
And so when I went to one of my office visits, I took it out of my bag and casually handed it to my surgeon.
“You forgot this in my room when I had my surgery,” I said.
He thanked me and said “I wondered where it had gone.”
January 23rd, 2013 §
 Perhaps the most common question I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a wonderful gift for someone who has just been diagnosed and is a necessity if you are the patient.
Perhaps the most common question I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a wonderful gift for someone who has just been diagnosed and is a necessity if you are the patient.
Being organized is one of the best ways to help yourself once you’ve been diagnosed. When you first hear the words, “You have cancer” your head starts to swim. Everything gets foggy, you have to keep convincing yourself it’s true.
But almost immediately decisions need to be made — decisions about doctors, treatments, and surgeries. Often these choices must be made under time constraints. You may be seeing many different doctors for consultations. Medical oncologists, surgical oncologists, radiation oncologists, recontructive surgeons, internists— there are many different voices that you may hear, and they may be conflicting. It’s hard to keep it all straight in the midst of the emotional news. Not only are you likely to be scared, but also you are suddenly thrust into a world with a whole new vocabulary. By the time you are done with it, you will feel you have mastered a second language.
You can help your care and treatment by being organized. Especially if you are juggling different specialists and different medical facilities, you must remember that the common factor in all of this is you. It’s your health. It’s your life. I believe it’s important to travel with a binder of information about your medical history and treatment, as well as notes and questions.
This binder will mean that all of your information about your cancer will be in one place. This will be your resource guide. I cannot tell you how many times physicians have asked about my binder and said when I was able to produce test results, pathology reports, or other information they needed, “I wish every patient had one of those.”
I suggest the following:
A heavy 3-ring binder
I think a 1.5″ binder is a good size to start. This size will allow you to easily access reports and pages and have room for the calendar. It will look big at first but you won’t believe how quickly you will fill it up.
Colored tab dividers
I like these to be erasable. I think 8 is the minimum number you will need. If you have a lot of specialists you will need more. The categories you think you will need at the outset may change. It’s easy to erase and reorganize them. Put the categories you will be accessing the most in the front so you aren’t always having to flip to the back. Once the binder is full it will make a difference.
Some starting categories:
- schedules (dates of appointments you have had, when the next ones are due, and how often you need certain tests done)
- test results/pathology (it’s very important to keep copies of MRI, CT, and pathology reports so that you correctly tell other doctors what your diagnosis is. For example, new patients often confuse “grade” with “stage” of cancer.)
- insurance (keep copies of all correspondence, denial of claims, appeal letters, explanations of benefits)
- articles and research (handouts, post-surgical information. Ask if there are any websites your doctor does approve of. My own oncologist said, “Do not read anything about cancer on the internet unless it comes from a source I’ve told you is okay. There’s a lot of misinformation out there.”) Keep your post-surgical instructions, any info given to you about aftercare.
- radiation/chemo (keep records of exactly what you had done, number of sessions, dates, drug names, etc. I also asked how my dose was calculated so I knew exactly how much of each drug I received in total)
- medications (drug names, dates you took them, dosage, side effects). I also keep a list of all of my current medications as a “note” in my iPhone. That way I can just copy it down and won’t forget anything on the list. You should always include any vitamins or supplements you take.
- medical history (write out your own medical history and keep it handy so that when you fill out forms asking for the information you won’t forget anything. As part of it, include any relatives that had cancer. Write out what type it was, how old they were at death, and their cause of death. Also in this section include genetic test results, if relevant)
Loose leaf paper
Perfect for note-taking at appointments, jotting down questions you have for each doctor. You can file them in the approporiate category so when you arrive at a doctor your questions are all in one place.
Business card pages
These are one of my best ideas. At every doctor’s office, ask for a business card.Keep a card from every doctor you visit even if you ultimately decide not to return to them. If you have had any consultation or bloodwork there, you should have a card. That way, you will always have contact information when filling out forms at each doctor’s office. For hospitals, get cards from the radiology department and medical records department so if you need to contact them you will have it. Also, you want contact information for all pathology departments that have seen slides from any biopsy you have had. You may need to contact them to have your slides sent out for a second opinion.
This is also a good place to keep your appointment reminder cards.
CD holders
At CT, MRI or other imaging tests, ask them to burn a CD for your records. Hospitals are used to making copies for patients these days and often don’t charge for it. Keep one copy for yourself of each test that you do not give away. If you need a copy to bring to a physician, get an extra made, don’t give yours up. If you need to get it from medical records from the hospital, do that. You want to know you always have a copy of these images.
Keep a copy of most recent bloodwork (especially during chemo), operative notes from your surgeries (you usually have to ask for these), pathology reports, and radiology reports of interpretations of any test (MRI, CT, mammogram, etc.) you may have had. Pathology reports are vital.
Calendar
I suggest a 3-hole calendar to keep in your binder. This will serve not only to keep all of your appointments in one place but also allow you to put reminders of when you need to have follow-up visits. Sometimes doctor’s offices do not have their schedules set 3, 6, or 12 months in advance. You can put a reminder notice to yourself in the appropriate month to call ahead to check/schedule the appointment.
Similarly you can document when you had certain tests (mammograms, bone density, bloodwork) so you will have the date available. I usually keep a piece of lined paper in the “scheduling” section of my binder that lists by month and year every test/appointment that is due and also every test I’ve had and when I had it.
Sticky note tabs
These can be used to easily identify important papers that you will refer to often, including diagnosis and pathology. These stick on the side of the page and can be removed easily. As your binder fills up, they can be very helpful to identify your most recent bloodwork, for example.
Plastic folder sleeves
These are clear plastic sleeves that you access from the top. They can be useful for storing prescriptions or small notes that your doctor may give you. The sleeves make them easy to see/find and you won’t lose the small slips of paper. Also a good place to store any lab orders that might be given to you ahead of time.
The above suggestions are a good working start to being organized during your cancer treatment. If you want to do something for a friend who is newly diagnosed, go out and buy the supplies, organize the binder and give it to your friend. He or she will most likely appreciate being given a ready-made tool to use in the difficult days ahead.
I also believe a modified version is equally useful for diagnoses other than cancer. When our youngest son was born with defects in his spine and hands it took many specialists and lots of tests to get a correct diagnosis. Having all of his tests and papers in a binder like this was instrumental in keeping his care coordinated. In fact, at his first surgery at The Children’s Hospital of Pennsylvania they gave us a binder to assist in this process. I know some hospitals do this for newly diagnosed patients already. Maybe my tips will help you or a friend know how to better use the one you already have. You may not need all of these elements depending on the complexity of your case, but I hope you will find some of these suggestions useful.
January 23rd, 2013 §
First order of business is a late reminder that today (Wednesday) I will be on Doctor Radio on SiriusXM 81 from 1:00-1:30 EST on the Oncology show.
I’ll be talking about my first diagnosis of stage II cancer and then my recent diagnosis of stage IV metastatic cancer, my blog, and how to improve the doctor-patient relationship. You can call 877-NYU-DOCS if you want to ask questions! We will be live for that time period. You can even email questions in during that time (or even before, just send them to docs@siriusxm.com and say it’s for me on today’s oncology show). The half hour will go fast I’m sure. The taped show will then repeat tonight at 11 pm. I think you can go here to listen for free for a week if you want to listen in today: http://www.siriusxm.com/freetrial
……………………….
I had intended to be posting each day this month but this weekend caught up with me. In the negative column, side effects from chemo this weekend were worse than usual. The nausea was the most debilitating one. Two out of the three weekend days were pretty much lost. As a result I could not get posts up. I am sorry about that.
However, these negatives were overshadowed a million times over by the other reason I was too busy to be writing. The photos you see are of the new addition to our family. Lucy is a two year old Pembroke Welsh Corgi that came to live with us on Sunday. She is a sweet and loving dog, and has made the adjustment to her new home seamlessly. My children (14, 11, 6) have fallen head over heels in love. Paige knew we were getting her but the boys were unaware… I loved having a surprise for them. I’ll write more about that soon.
We thank Gaye and John Georges at Calista Corgis for raising this beautiful dog who is a treasured part of our home now.
I’ll include a few photos and then be back this week finish out my month of revisiting some of the most-requested old posts. Yesterday I was at Sloan Kettering talking about side effects, PET scans, and tumor markers. As always, my doctors are very thorough and I always leave with more information about options and perspective. I was also able to share with Dr. Dang that with your generosity we’ve raised over $15,000 in 3 weeks for metastatic breast cancer research on my Sloan Kettering Giving page.
Thanks to all for your support this week.



January 19th, 2013 §
I wrote this back in 2010. Just like in this week’s “I think so too” I decided to think about the history of an object.
………………………………..
I took my friend Brenda out to lunch for her birthday today. While we were sharing an appetizer, a group of four people entered the restaurant: three men dressed in business attire accompanied a woman with a knit cap on. I realized in an instant she was bald underneath that covering and postulated that the hat would not be coming off.
They took off their coats and sat down at the table. I watched them for a while, from a distance, across the restaurant. Indeed, the hat did not come off. She was bald, most certainly, and likely undergoing chemotherapy. My mind started to wander, and I started to wonder. Was she at a business lunch and able to keep working during this crisis? Was she done with treatment and waiting for her hair to grow back in or was she on an “off week” of chemo when food might be somewhat appealing?
I kept looking at her hat. It was freezing cold out today, so it wasn’t particularly out of place. But I kept staring at it. It looked handknit. Had someone she knew made it for her? Had she gotten it from the basket at the cancer center where people knit and donate hats for patients?
I wonder what she’ll do with the hat when her hair grows back in: will she throw it away? Burn it? Give it to someone else who needs it? After wearing those head coverings day after day, you don’t want to lay eyes on them again. After my hair grew back, I saved my scarves for a friend’s sister who was set to start chemo shortly after I finished. I recently saw pictures of her wearing them. It’s odd to see them, associated with so many memories for me, on her head too. Now I have the scarves back, and some have already been lent to another member of the club.
My wig, worn twice, is packed away in the basement. I will soon donate it to a charity that provides wigs to women who can’t afford them. I hate that wig. I hate what it looks like. I hate how it feels. I hate how I looked in it. Twice I wore it, and I had to keep from tearing it off every second it was on my head. It wasn’t me; I felt like someone else in it. But I just can’t get rid of it yet. It’s like a trophy for walking through the fire.
I wonder if that woman I saw at lunch today feels like that. She and her group finished their meals and left before I did. I was really sorry I didn’t get to tell her that her hat looked great on her.
January 17th, 2013 §
** please note I updated this post in October 2013. I added the following information:
Once again Facebook games about breast cancer are making the rounds now that it is October. I posted this last year and got some flack from people who thought anything that “raised awareness” about breast cancer was good and couldn’t understand why I am critical of these messages.
My point is that this isn’t awareness.
There probably isn’t anyone on Facebook who doesn’t know that breast cancer exists. But there certainly is a lot of myth-busting to be done. This is not how to do it. Topics that do need attention include male breast cancer, the underfunding of metastatic research (30% of people with breast cancer will eventually have metastases yet less than 5% of breast cancer funding overall goes to metastatic research), the fact that for many breast cancers 5 years in remission does not mean you’re free from risk of recurrence, not all breast cancer presents with a lump so self exams and/or mammograms may not always find certain types of breast cancer (inflammatory breast cancer)… the list goes on and on.
There’s a lot of work to be done educating. Education is awareness, these Facebook posts are not.
A friend asked me, “What can I do to help? I can’t donate money to your research fund but would like some ideas on things I could do instead.” What a great question. Rather than post these messages on your Facebook page here are a few easy ideas:
1. Make sure you are properly vaccinated from vaccine-preventable illnesses. This includes your family (kids and your parents if applicable), friends, and anyone else you can get involved (nag). Boosters like those for pertussis are very important. Get your annual flu shot. People over the age of 65 and some others at high risk should also talk to doctors about the pneumonia vaccine.
2. If eligible, donate blood and platelets. These products are needed by cancer patients constantly.
3. If eligible, get tested to be a bone marrow donor. Go to BeTheMatch.com to see the requirements. The initial registry just requires a cheek swab. It’s easy as can be.
4. Read blogs/follow tweets by people living with cancer. I think understanding the day to day lives of those of us living with it is a great way to truly become more aware. It’s one of the reasons I spend so much time writing here. I try to bring you the science, the experience, the thoughts of a mother trying to cope with raising a family and managing an terminal diagnosis.
If you want to see the comments on the new post you can go here. The original post appears below:
………………………….
I don’t usually rant, but something has me steaming. Today the following exact message appeared in my Facebook inbox:
So here is the time of year again when we try to raise awareness for breast cancer through a game. It’s very easy and I would like all of you to participate. Two years ago we had to write the color of our underwear on our wall. Men wondered for days at what was going on with random colors on our walls. This year we make references to your love life status. Do not answer to this message just post the corresponding word on your wall AND send this message privately to all the girls in your contact list!!!!!! BLUEBERRY = single; PINEAPPLE = it’s complicated; RASPBERRY = I can’t / don’t want to commit; APPLE= engaged; CHERRY= in a relationship; BANANA=married; AVOCADO= I’m the better half; STRAWBERRY= can’t find Mr. Right; LEMON = want to be single RAISIN = want to get married to my partner. Last time the underwear game was mentioned on tv, let’s see if we get there with this one !!!!!Copy and paste this message into a new one and send to all your girly friends and update your status with your answer. DO NOT RESPOND TO THIS CONVO, just leave and participate.
I’m going to keep my reaction short. I’m hoping writing something down like this will allow people who are as infuriated as I am with these silly requests to have something to react with.
First, I give you permission to ignore this crap. Better yet, write back to the people who have shared it. Let’s do some real awareness here.
The above instructions are not awareness. This is offensive. Breast cancer is not a joke, awareness does not come from sharing the color of your underwear or your marital status (the whole “tee-hee, wink-wink” attitude adds to my disgust). Even if it ended up on TV, that still would not be educating people about breast cancer they didn’t know before. All it does is show the world that lots of people are willing to post silly things as their status updates.
Let’s do a piece of education right here. The status update says “only send this to your girly friends.” Um, hello… men get breast cancer too. Men are also the husbands, fathers, sons, brothers, and some of the friends, coworkers, nurses, and doctors who care for and are left grieving for people (men and women) who die of breast cancer. We should not exclude them from ANY discussion of cancer.
Just because it says it’s about “breast cancer awareness” doesn’t mean you have to agree. Go ahead. Ignore it. Or write back and tell them why you don’t want to be included in these things anymore. Another blogger, Susan Niebur, wrote about her take here. She was an astrophysicist, by the way. She died of metastatic breast cancer.
Anyone who has breast cancer and uses your FB status update as an indicator of whether you support their cause is not very enlightened. When I rank “how to help those of us with cancer,” sharing one of these paragraphs as a status update is the lowest possible method of showing support. There are endless ways to do that. I think it actually is the opposite; sharing these status updates makes people feel they are doing something real for breast cancer causes when they aren’t.
I’ve also had it with the “I’ll bet most of my friends won’t share this post” attempt to guilt me in to sharing something like “share this if you think domestic abuse is awful.” “Share this if you think autistic kids are special.” Well yes, actually, I believe both of those things. And just because I didn’t share them as my status update doesn’t mean I do NOT agree with the statements.
Education underlies awareness. To even call something a “game” and honestly believe it’s doing anything to help any aspect of this disease is delusional.
I also think that those of us who have had breast cancer have an obligation to speak out if we disagree with these posts. People look to us to see how we react. If we not only read these updates but share them, it does constitute endorsement. It says we agree. It says it’s okay to think of breast cancer awareness this way.
I say: count me out of these Facebook games.
I have stage 4 breast cancer and it is no game to me.
January 17th, 2013 §
There is comfort in routine. Some people are superstitious. Sometimes they want the same chemo nurse, the same appointment time, the same chair. “If it’s working don’t mess with it” applies to many things about treating cancer.
I’m always thinking about continuity and the stories that objects tell. I’ve written twice about the tape measure my plastic surgeon used to measure me before surgery. I’ll post those pieces again this month. Whenever I sit in a chair in a doctor’s office I think about all of the people who have sat in it before me.
Each person has a story. So, too, does each chair. Here is one from 2011.
……………………………
Back in 2011 my plastic/reconstructive surgeon asked, “Did you know it’s been four years since your reconstruction surgery?”
Immediately he chuckled, “Of course you know that,” he said, realizing my mental calendar was certainly more precise than his– of course I marked the days off in my head.
Whenever I sit in a waiting room I am instantly transported to that place and time. I sit and watch patients walking in and walking out. I can tell by hearing what the time interval until their next appointment what stage of treatment they are in.
I sit in the chair, the same one I did four years ago.
It’s the same chair, but I am not the same person.
My body is not the same.
There is continuity in that chair.
There is a story it tells me.
I wrote this piece to the next person who sits in that chair.
………………………….
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. PET scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments. Tears. Avoidance.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Asking the grocery line folks to “make the bags light, please.” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
Targeted treatments. Effective treatments.
Ultimately, someday, perhaps: a cure.
Don’t you think that would be amazing?
I think so too.
January 15th, 2013 §
When you have cancer you become an expert in reading cues.
Actually, when you’re in any serious situation I think that’s the case.
So when the nurse showed me into my oncologist’s office this morning, instead of to the usual exam room, I didn’t even make it through the doorway before forcing him to look at me while I said, “Uh-oh. This is not good.”
The door closed and he turned the computer screen to me. “Well, it’s not awful. It’s not terrible, but it’s a change.”
We looked at the trend of my tumor marker tests since October when I was diagnosed with metastatic (stage IV) cancer. Since that time my markers have declined quite consistently (with one exception which I’ll explain in a bit).
I get my blood drawn every two weeks. Some oncologists might think it should only be done monthly at this point. But my doctors and I are data people. Hey, when the news is good, who doesn’t want to hear/see it as often as possible? When it’s bad news, I could use it less frequently, thank you very much.
This week’s tumor marker was elevated slightly over the one from two weeks ago. It’s almost exactly what it was one month ago. The fact of the matter is had we drawn it monthly we’d be saying it’s stable.
But seeing this one blip now causes conjecture and concern. Now, it could be a natural variation in this test. After all, this test is not precise and does vary. No one tests patients daily to see how much it actually changes over the course of a month or a week. Going back to my earlier caveat about having had one previous rise in the marker: I had it drawn twice in four days when I was diagnosed back in October. Those results showed a rise of almost 5 points in four days — but were considered within similar range. Now I’m showing a seven point rise in two weeks. I’m not going to go into the standard devation and all of that stuff right now. It just doesn’t matter for these purposes.
For now, it’s just a blip. We don’t know if it’s an anomaly or part of a trend. There’s nothing to do but stay the course and wait. I’ll be starting chemo again this Thursday at the same dose as I have for the past few rounds (total of 3500 mg/Xeloda a day, split into two doses, 7 days on/7 days off).
My hands have been worse this round. My oncologist warns me that most people can’t tolerate long term use of this drug. I am not thinking about that. I’m thinking about bearing whatever I can for as long as I can if it’s working. The question is now: is it still working?
My feet are doing well actually (strange to be posting a “foot update” but…). They are very sensitive to shoes so I wear furry slippers at home and at least now that it’s winter I can wear soft lined shoes during the day. I do not have significant pain while walking. That is great in terms of quality of life.
My fingertips are simultaneously numb and very sensitive at the very tips. They are peeling and any pressure hurts. The finger wrinkles where the actual fingers bend (to grip) are white and cracked and sore. But I am able to drive which is a real help.
My shoulder (from the fracture in the collarbone area) is feeling much better. I still don’t lift anything on that side but day-to-day it doens’t cause me discomfort like it did. This is good; it means the bone is healing as the cancer shrinks it and the bone strengthener that I take by IV is helping. I am in discussion with my two oncologists to potentially try a different bone drug next time because I still am having side effects after each round of the IV one (normally only happen the first one or two times). This would be a switch from monthly intravenous Zometa to monthly injection of Xgeva.
After we see what the bloodwork shows in 2 weeks we’ll re-evaluate everything. It might be time for the PET scan, might be time to try a higher dose again of this chemo, might be time to watch and wait a bit more (it would be too soon to abandon ship on this chemo with just two data points).
I’ll discuss all of these issues with my other oncologist next week and I’ll count the days, minutes, and seconds until I get my next results back.
January 13th, 2013 §
Originally written on January 30, 2009 (the two year anniversary of my surgery).
……………………………..
I had two surgeons that day:
one just wasn’t enough for the job.
The surgical oncologist would take away,
the reconstructive surgeon would begin to put back.
Before I headed off into my slumber,
I stood as one marked me with purple marker.
He drew,
he checked,
he measured.
And then a laugh,
always a laugh to break the tension:
Surgeons must initial the body part to be removed to ensure
they remove the correct one.
But what if you are removing both?
How silly to sign twice,
we agreed.
And yet he did,
initialing my breasts with his unwelcome autograph.
The edges of the yellow fabric measuring tape he used
had purple fingerprints up and down their sides;
use after use had changed their hue.
And now it was my turn to go under the knife –
a few more purple prints on the tape.
I got marked many a time by him that year.
Endless rounds of
purple dots,
dashes,
and lines
punctuating my body
with their strange, secret blueprint
only those wearing blue understood.
We stood in front of mirrors
making decisions in tandem
as to how my body should and would take new shape.
Two years today and counting.
Moving forward.
Sometimes crawling,
sometimes marching,
and sometimes just stopping to rest
and take note of my location.
Numb inside and out,
but determined.
Grateful,
hopeful,
often melancholy.
Here comes another year
to put more distance
between
it and me.
Let’s go.
January 12th, 2013 §
Now that my cancer is stage IV many things that once seemed important are now at the bottom of my list. I distinctly remember during and after my breast reconstruction that I was very obsessed with every tiny detail about my implants. What size should they be? Were they healing well? Were they even? How did they compare to other women’s reconstructed breasts?
I think after I finished chemo I needed something to focus on. It seemed that this was something positive. Something for me. Something that would make me feel better (after all, those tissue expanders before the implants were the pits).
The time between when I was diagnosed and when I had my double mastectomy was about one month. Those were anxiety-filled weeks. Though I consoled myself with the news that my cancer was confined and surgery would most likely be enough to treat it, later I learned after the mastectomies that my cancer was actually stage II.
I look now at this piece I wrote and I can still connect to it. I still remember what it felt like. But now that I’ve got metastatic cancer I don’t give a damn about how my implants look. None of that matters to me. One of my first phone calls after the new stage IV diagnosis was to my plastic surgeon to ask if there was any reason to consider removing them if it would help any of my treatments that are to come (there isn’t).
This piece was written about my first diagnosis and surgery… when it was all very new. It seems so long ago. A lifetime. It’s been six years.
……………………………………
In the weeks before my surgery, I looked at pictures of double mastectomy patients on the Internet. I Googled “bilateral mastectomy images before and after” thinking I was doing research. I thought I was preparing myself for what was coming.
In reality I was trying to scare myself. I wanted to see if I could handle the worst; if I could, I would be ready. My reaction to those images would be my litmus test.
Some of the pictures were horrific. I sat transfixed. I looked. I sobbed. I saw scarred, bizarre, transformed bodies and couldn’t believe that was going to be my body.
Days later, when I met my surgeon for my pre-op appointment for the first time he said, “From now on, don’t look at pictures on the Internet. If you want to see before and after pictures, ask me: look at ones in my office. You can’t look at random pictures and think that’s necessarily what you are going to look like.”
All I could do was duck my head in an admission of guilt. How did he know what I’d done?
I realized how he knew: other women must do this. Other women must have made this mistake.
The aftermath is terrible to me though not in the ways I’d anticipated. I have no sensation in my chest. I never will.
A major erogenous zone has been completely taken away from me. Yes, I have new nipples constructed, but they have no feeling in them; they are completely cosmetic. The entire reconstruction looks great but I can’t feel any of it. It does help me psychologically beyond measure to have had these procedures though.
Here I sit, two gel-filled silicone shells inside my body simulating the biologically feminine body parts I should have. And sometimes that thought is disturbing.
To be clear: I don’t regret having them put in. I’ve never regretted that. It was a decision I made, and made deliberately. I knew that reconstructing my breasts was the right decision for me. I am overwhelmingly happy with the cosmetic appearance and the wonderful job my talented surgeon did. I will always be grateful to him for what he’s done.
I definitely don’t remember what my breasts looked like before. I only remember these.
I once asked my plastic surgeon to see my “before” pictures a year or two after my reconstruction was over. You know what? My “before” breasts didn’t look so great.
In my mind they did though.
In my mind, everything about my life before cancer was better.
But that’s not the truth.
Don’t take that as an endorsement of the “cancer is a gift” nonsense though.
My mind distorts the memory of my body before cancer. Then forgets it.
My mind distorts the memory of my life before cancer. Then forgets it.
With time, I can get used to a new self.
It’s like catching my reflection in the mirror: only lately do I recognize the person staring back at me.
For over a year the new hair threw me. It’s darker than I remember it being before it fell out. It’s shorter than it was before, too.
And the look in my eyes? That’s different also.
I just don’t recognize myself some days.
Sounds like a cliché if you haven’t lived it.
But it’s true.
January 11th, 2013 §
One of the ways you can be a good friend to someone going through a difficult time is to use open-ended questions. In this way, you are not projecting your own feelings onto them; neither are you assuming what feelings they are having. Trust me: they’ll appreciate it.
…………………………………..
There are ways in which I will never make you as readers understand what it’s like to have cancer if you haven’t. However, part of the reason I write this blog is to try to explain some of the cancer patient “mentality” (if you’ll accept such a generalization) to those of you who haven’t had cancer. To that end, you can hopefully be better friends, partners, spouses, sons, and daughters. There are things I didn’t know before I had cancer that I wish I had understood.
It’s not that I am special.
It’s not that I am so smart.
It’s that I have been there.
Hopefully sooner than you have.
And so I am reporting back from the field. To try to help you. Prepare you. Because if there is one thing I know, one thing I know for sure: you will know someone. It might be your friend. Your parent. Your child. Or even yourself. Maybe you already know someone. But one thing is for sure: you will know someone who gets cancer. And you know what? You already know me.
One of the ways your life changes when you have had cancer is that you begin to understand the phrase “It’s never over” in a whole new way.
As soon as you hear the three words, “You have cancer” your life changes. From the time you hear those words everything is different. You now have a history of cancer — even if it’s a cancer that can be removed and you don’t need any other treatment. It is now a history that puts you at risk. Now every medical problem, every medical history you give, every question mark, every medical mystery must be filtered through the lens of a history of cancer.
A woman I know from college was writing a brief note to me by email to thank me for something nice I’d done. The last part said, “You must be on top of the world (or close to it).”
My reaction? First I burst out in laughter.
Ah, the naiveté of the healthy!
On top of the world! Ha!
Then it actually got me riled up.
Angry.
How dare she think it was over.
Then I got angry at myself for lashing out.
I became contrite.
Why should she know better?
How could she know better?
It isn’t fair to expect people to know better.
Only once you know better can you do better.
If she only knew.
What was I going to do?
Write back and explain to her the error in her thinking?
Should I write back and say:
I counted every day, every hour, every minute, every second to be “done.” But when each thing was “done” there was always something else I was counting toward. Always something else looming. I’m never “done.” It’s never “done.” It’s never “over.”
The language we use reveals a lot.
When someone says,
“You must be on top of the world,”
that means:
“You should be”
“You ought to be”
or
“I expect you to be.”
For someone like me, if I don’t feel like that it’s hard.
I get angry. I want to say all of the reasons why that’s not realistic– why that’s wrong. Why that’s precisely what I’m not feeling.
But then, when my anger cools, I take that and turn it inward. And all I feel is disappointment. Disappointment in myself. Maybe I should feel like that. Maybe I really should feel on top of the world. The fact that I don’t means I’m not as far through this thing as I thought. It reminds me I’ve still got a lot of work to do.
But I think the point remains: just surviving cancer isn’t necessarily enough. It’s not enough to make you feel on top of the world.
You can help those who have had cancer by not making the leap that just because they have lived through this round that they have “won”; don’t assume that they will necessarily be ecstatic, “done,” and ready to move on.
Rather than telling people what they “must” feel, we all can be better friends and listeners by asking questions rather than making statements.
Rather than saying “you must feel on top of the world” think of the difference it would have made if my friend had said, “Now that your treatment and surgeries are over, how do you feel?”
An open-ended question is always a safe conversation starter. I’m going to try it more often in my everyday life; I hope you will too. My wish is that it begins some good conversations between you and someone you care about.
January 10th, 2013 §
My current chemotherapy is oral. Oral chemos are common with metastatic cancer. My veins are happy to hear this; after my original surgeries and chemo the only usable veins I have are in the top of my right hand. All bloodwork and IVs for surgeries and drug infusions must be placed there. It’s not easy and takes planning at each visit what vein should be used for what purpose. When the time comes to start an IV chemo in the future I’ll need a port.
Oral chemo is more convenient, of course. The one I’m on now used to be an IV that needed to be administered over the course of days, so patients would need to be on an IV pump during that time. Obviously, swallowing pills and getting the same drug is better for the patient’s quality of life. I’m glad I am able to use the oral version.
For most people, the prospect of losing all of their hair is disturbing. Not just on your head, but eyebrows, eyelashes, all of it. I wrote this for a friend a few years ago. Now I have another friend about to start chemo this week and I wanted to share it again. Thinking of you, Amy.
……………………………….
originally published September 12, 2009
My friend Andrea found out she needs to have chemo. I cried a lot the day I found that out. Last night she emailed me that she was thinking about the whole “losing her hair” thing. She has gorgeous hair. Thick. Straight. Reddish-brown, in the sun I’d say it has a honey shine in it. She usually wears it back in a ponytail, as she says, “taking it for granted.”
I started writing her back to tell her that focusing on her hair wasn’t silly. There are many things about cancer that are real worries. One of them is going bald. Especially for a woman. And as I typed to her I realized the words were flowing fast and furious.
I realized all the things people had said to me when I was worried about losing my hair and all of the things people had said to me after it eventually happened.
Everyone wants to reassure you that it isn’t as bad as you think it is.
Some days you convince yourself it isn’t that bad.
Some days you are sure they are all lying to you.
Either way, you get through the days.
The day you take that hat or wig or scarf off and wear your newly-grown stubble or “mouse fur” out in public is a great day (My first hair was so fine and soft and thin that it didn’t resemble hair at all… I called it mouse fur because while it blissfully covered my head and was dark, it couldn’t be cut or styled).
So, for my friend, and for other women who are getting ready to start chemo (and those who bravely walk through the world every day without hair because of alopecia and other conditions), no matter what, it matters.
No matter what anyone says…
all the things they will say:
“It’s only hair.
It’ll grow back.
You’ll look so pretty anyway.”
“With a face like yours it won’t matter.
We’ll get you a cute wig.
We’ll get great scarves.
It’ll grow back in no time.
Maybe it’ll be better after it grows in.”
“It might be curly.
It might be straight.
I know someone whose hair came in gray.
I know someone whose hair came in red.
I know someone whose hair came in black.
I know someone whose hair came in white.”
“Hers came in curly.
Hers came in straight.
Did you see hers?
It looks great.
Did you see hers?
It looks awful.”
“I like her better with short hair.
I liked her better with long hair.
You’re gonna look great.
I don’t know what I’d do.
I don’t know how you do it.
I don’t know how you’re gonna do it.”
“You are so brave.
You are so strong.
You can do it.
You can beat this.”
No matter what anyone says–
It is just going to suck.
Bigtime.
You may shed many tears over this one.
It may be harder than you thought.
I’ve heard some women say it was harder for them than the actual chemo.
Reports show women actually turn down the chemotherapy they need because they don’t want to go bald.
It’s real.
It’s hard.
But hair matters.
To us,
To our kids,
To our husbands,
To our friends.
My hair has never been the same since chemo.
I’m not alone in that.
In fact,
My hair now grows “the other way”…
My part is on the opposite side of my head than it used to be.
I think that’s kind of neat.
There’s the way my hair was B.C. (before cancer)
And the way it is now.
It is a big deal.
Don’t let anyone minimize it.
If they do, make them go shave their heads.
Not just clipper cut.
Straight razor shave it until there’s nothing left.
Then the eyebrows.
Then the eyelashes.
And then the stuff they might not think about.
Every piece of body hair.
Of course there are jokes.
And giggles.
The Brazilian wax done for you.
It’s funny.
But not so funny.
Then when your nose hairs fall out you suddenly realize how
Much you needed them.
Your nose runs constantly.
And it’s embarrassing.
Mine dripped clear liquid constantly.
I was so embarrassed.
No one had told me about that part.
I had a tissue stuffed in every pocket.
Because there were no hairs to stop the drip.
Chemo drip.
You try to imagine what it will be like.
You try to picture what you will look like bald.
You pull your hair back,
Slick it back,
Try a wig on to see what it might look like.
But nothing can prepare you.
For that crappy day,
Two weeks in.
When you scratch an itch
Or touch your head
And take away a handful of hair
Or find it on your pillow.
And the sight of it is so sad,
But so disgusting
So repulsive,
That you need it gone.
And then if you need me
You will call me.
And I will come.
And I will cut it.
Or maybe I will just come and cry with you.
And remember what it felt like.
No matter what anyone says,
It isn’t nothing.
It is something.
And even in the scheme of all of the things to be afraid of with cancer,
How you feel about losing your hair is real.
It matters.
And I remember.
January 9th, 2013 §
Elizabeth Edwards reached many people because she was in the public eye, but inspirational people also live quiet lives. We can be inspired by Edwards’s grace and courage as she dealt with the challenging parts of her life in the same way we can find inspirational people around us each and every day. These are all people we can connect with and learn from. In doing so, we better ourselves.
When she was diagnosed with metastatic cancer people told me not to worry: it wouldn’t happen to me just because it happened to her. That’s true. It wouldn’t happen just because it happened to her. But it did happen. And now I look back on everything I’ve said for the past 5.5 years and I am glad I expressed those thoughts as they were happening. Because my fear came true.
…………………………………..
(from December 7, 2010).
I didn’t know Elizabeth Edwards. In fact, I wrote a piece critical of her when she initially stood by John after his affair. I was disappointed when she gave an interview on CNN in May of 2009 and spoke only of John’s “imperfection” rather than calling him the cheater he was and kicking him to the curb. I was angry she hadn’t used her interview time to talk about herself, her cancer, her life: the topics I wanted to hear about. I was angry at her for not claiming her remaining years of life as her own.
So why am I sitting with tears in my eyes because she has died?
I cry because it makes me feel vulnerable and scared of what this disease can do to me: what it did to her.
Yes, I know… there are plenty of men and women who get cancer, have treatment, and stay in remission for the rest of their lives. And, in essence, isn’t that what every cancer patient hopes for, as Betty Rollins wrote, “to die of something else”?
I don’t think it makes me pessimistic, depressing, or negative to think that I am vulnerable.
It’s the truth. It’s my truth.
Anyone who hasn’t been to the oncologist with me to see my risk-of-recurrence charts, my mortality charts, my decision-making discussions along the way can’t say to me “Oh, don’t worry, that won’t be you.” No one, including me, knows how it will go.
People tell me: stay strong, just think positive, you can’t generalize from her situation.
I respond: I am strong, I hope for the best. I don’t think positive thinking is going to save me if there are remaining cancer cells still in me.
I hope that people won’t say to someone who has been diagnosed with cancer, “Don’t worry, what happened to Elizabeth Edwards won’t happen to you.” Because while we do everything we can to ensure we die of something else, it just isn’t always the case. In 2006 her oncologist told her that there were many things going on in her life, “but cancer was not one of them.” Things change quickly, cancer can recur when you least expect it.
I have sympathy for her family. I cry for her children. I am saddened about the years she spent with a man who didn’t deserve her. I am angry about the time she wasted on him. I hoped she would be an example of someone who would keep cancer at bay.
I grieve for that hope, now gone.
January 8th, 2013 §
“Two Cents” was one of the first things I wrote for the blog. I don’t know if it’s poetry or a rant or what. I distinctly remember writing it: I scribbled it down on the back of a brown paper sleeve from a Starbucks donut as I waited for Paige to finish her piano lesson one sunny day several years ago. I’m quite sure the impetus was being told that “things happen for a reason.” I still find this one simple, but true. Many readers still have a soft spot for this early piece in which I provide my own two cents’ worth.
…………………………………….
Don’t tell me things happen for a reason.
Don’t tell me there is a plan.
Don’t tell me I’m supposed to learn a lesson from this.
Don’t tell me I’m a better person for it.
Tell me I’m strong.
Tell me I’m tough.
Tell me I did it well.
Tell me you care.
I don’t believe I was given cancer for a reason.
I don’t believe there is a master plan.
I don’t believe this is a test.
I don’t believe you only are given what you can handle.
I know I will learn lessons.
I know I will be stronger.
I know sometimes it is too much to handle.
I know sometimes I want to give up.
I know sometimes I thought dying would be easier.
I believe the power is in me.
I believe the power is in my doctors.
I believe in the power of medical science.
I believe unless you have experienced this, you cannot know.
I believe unless you’ve been there, you cannot give advice.
I believe unless you’ve felt it, you cannot judge.
I believe in the power of friendship and love to make the journey bearable.
I believe suffering is a process.
I believe in picking myself up and pressing forward.
Again.
And again.
And again.
I believe persistence pays off.
I believe in enjoying the gifts I’ve been given.
I believe many people will never understand.
It might sadden me, anger me, and frustrate me.
But in the end that does not matter.
I can only be true to myself.
I must be true to myself.
January 7th, 2013 §

Revisiting old blogposts is taking me on an emotional rollercoaster. Being on the other side — having things I was most afraid of actually coming true — gives the pieces a whole new meaning. Of course one of my main fears was that my cancer would return. Of course, it has, and worse. The metastases I have now are exactly what I feared most after my treatment was complete the first time around.
Again, I’d like to say that even when I feared it, as I would think most people who have had cancer do have fear of cancer returning/metastasizing, hearing the words “You have Stage IV cancer” bears no relationship whatsoever to the fear you have when it’s a hypothetical. The anxiety, the panic, the worry… all of those were only a fraction of what it felt like to be told it was actually true. This is what my life will be.
As I re-read the post below I got emotional. The words I wrote here over two years ago are still so true for me. This post captures my fervent wish to document my thoughts and feelings for my children. I still feel a strong desire to be understood. Perhaps some of this is because I think in many cases people with cancer do not feel understood.
Katie and I became friends after I read her book. Great friends. We talk about Suzy. We talk about french fries and silly socks and Pilates. We talk about her work and we talk about our kids. We talk about cancer. We talk about the most frivolous parts of life and the most serious. As I write below, “Even after her death, Suzy has the lovely ability to inspire, to entertain, to be present.” In life, so does her daughter, Katie.
………………………………….
There comes a point in your life when you realize that your parents are people too. Not just chaffeurs, laundresses, baseball-catchers, etc.– but people. And when that happens, it is a lightbulb moment, a moment in which a parent’s humanity, flaws, and individuality come into focus.
If you are lucky, like I am, you get a window into that world via an adult relationship with your parents. In this domain you start to learn more about them; you see them through the eyes of their friends, their employer, their spouse, and their other children.
Yesterday I sat transfixed reading Katherine Rosman’s book If You Knew Suzy: A Mother, A Daughter, A Reporter’s Notebook cover to cover. The book arrived at noon and at 11:00 last night I shut the back cover and went to sleep. But by the middle of the night I was up again, thinking about it.
I had read an excerpt of the book in a magazine and had already been following Katie on Twitter. I knew this was going to be a powerful book for me, and I was right. Katie is a columnist for The Wall Street Journal and went on a mission to learn about her mother after her mother died in June, 2005 from lung cancer. In an attempt to assemble a completed puzzle of who her mother was, Katie travels around the country to talk with those who knew her mother: a golf caddy, some of her Pilates students, her doctors, and even people who interacted with Suzy via Ebay when she started buying up decorative glass after her diagnosis.
Katie learns a lot about her mother; she is able to round out the picture of who her mother was as a friend, a wife, a mother, a strong and humorous woman with an intense, fighting spirit. These revelations sit amidst the narrative of Katie’s experience watching her mother going through treatment in both Arizona and New York, ultimately dying at home one night while Katie and some family members are asleep in another room.
I teared up many times during my afternoon getting to know not only Suzy, but also Katie and her sister Lizzie. There were so many parts of the book that affected me. The main themes that really had the mental gears going were those of fear, regret, control, and wonder.
I fear that what happened to Suzy will happen to me:
My cancer will return.
I will have to leave the ones I love.
I will go “unknown.”
My children and my spouse will have to care for me.
My needs will impinge on their worlds.
The day-to-day caretaking will overshadow my life, and who I was.
I will die before I have done all that I want to do, see all that I want to see.
As I read the book I realized the tribute Katie has created to her mother. As a mother of three children myself, I am so sad that Suzy did not live to see this accomplishment (of course, it was Suzy’s death that spurred the project, so it is an inherent Catch-22). Suzy loved to brag about Katie’s accomplishments; I can only imagine if she could have walked around her daily life bragging that her daughter had written a book about her… and a loving one at that.
Rosman has not been without critics as she went on this fact-finding mission in true reporter-style. One dinner party guest she talked with said, ” … you really have no way of knowing what, if anything, any of your discoveries signify.” True: I wondered as others have, where Suzy’s dearest friends were… but where is the mystery in that? To me, Rosman’s book is “significant” (in the words of the guest) because it shows how it is often those with whom we are only tangentially connected, those with whom we may have a unidimensional relationship (a golf caddy, an Ebay seller, a Pilates student) may be the ones we confide in the most. For example, while Katie was researching, she found that her mother had talked with relative strangers about her fear of dying, but rarely (if ever) had extended conversations about the topic with her own children.
It’s precisely the fact that some people find it easier to tell the stranger next to them on the airplane things that they conceal from their own family that makes Katie’s story so accessible. What do her discoveries signify? For me it was less about the details Katie learned about her mother. For me, the story of her mother’s death, the process of dying, the resilient spirit that refuses to give in, the ways in which our health care system and doctors think about and react to patients’ physical and emotional needs– all of these are significant. The things left unsaid as a woman dies of cancer, the people she leaves behind who mourn her loss, the way one person can affect the lives of others in a unique way… these are things that are “significant.”
I woke up in the middle of the night thinking about the book. My head spun with all of the emotions it raised in me. I think that part of the reason writing has become so important to me is precisely because I do realize that cancer can return at any moment. And if you don’t have an author in the family who might undertake an enormous project as Katie did, where will that explanation of who you were — what you thought — come from?
Is my writing an extension of my desire to control things when cancer has taken away so much of this ability?
Is part of the reason I write an attempt to document my thoughts, my perspective for after I am gone… am I, in a smaller way, trying to do for myself what Katie did for her mother?
If I don’t do it, who will do it for me?
And in my odd way of thinking, am I trying to save anyone the considerable effort of having to work to figure out who I was– deep down?
My blog originally had the title “You’d Never Know”: I am telling you things about myself, my worldview, and my life, that you would otherwise have no knowledge of. One of the things people say to me all the time is, “You’d never know to look at you that you had cancer.” After hearing this comment repeatedly I realized that much of our lives are like that:
If we don’t tell someone — share our feelings and experiences — are our lives the proverbial trees falling (unheard) in the forest?
What if you die without being truly understood?
Would that be a life wasted?
If you don’t say things for yourself can you count on others to express them for you?
Further, can anyone really know anyone else in her entirety?
After a loved one dies, there always seems to be at least one mystery person: an individual contacts the family by email, phone, or in person to say, “I knew your loved one: this is how I knew her, this is what I remember about her, and this is what she meant to me.” I know that this happened when Barbara (my beloved mother-in-law) died suddenly in a 2009 car crash. There are stories to be told, memories to be shared. The living gain knowledge about their loved one. Most often, I think families find these insights comforting and informative.
Katie did the work: she’s made a tribute to her mother that will endure not only in its documentation of the person her mother was (and she was quite a character!) but also in sharing her with all of us.
Even after her death, Suzy has the lovely ability to inspire, to entertain, to be present.
I could talk more about the book, Katie’s wonderful writing, and cancer, but I would rather you read it for yourself. I’m still processing it all, making sense of this disease and how it affects families, and being sad that Katie’s children didn’t get to know their grandmother. Katie did have the joy of telling her mother she was pregnant with her first child, but Suzy did not live long enough to see her grandson born. In a heartwarming gesture, Katie names her son Ariel, derived from Suzy’s Hebrew name Ariella Chaya.
I thank Katie for sharing her mother with me, with us. As a writer I learned a lot from reading this book. I’ve said many times recently that “we don’t need another memoir.” I was so wrong. That’s like saying, “I don’t need to meet anyone new. I don’t need another friend.” Truth is, there are many special people. Katie and Suzy Rosman are two of them.
January 5th, 2013 §
From June, 2009. I’ve been thinking about writing a new post about the word “inspirational” for a few weeks now. I am sure I will someday soon. For now, I want to share this post from a few years ago that a few people mentioned as one of their favorites. Of course some things have changed since then. I need to think about some of the things I’ve said here.
But I do still believe in setting an example.
I still believe in doing my best.
I still believe in doing as much as I can for as long as I can.
………………………………..
What does it mean to “be an inspiration”? A few people have said that to me recently: I am an inspiration. At first I laugh. I guess I’m an inspiration because I’m still alive. Maybe that’s enough.
What’s inspirational about me? Trust me, I’m not searching for platitudes here. I’m trying to get at “what makes someone an inspiration” and why do people think I and so many other breast cancer survivors qualify? There’s definitely more than one day’s blog in this question.
Is it being a mother and worrying about your children more than yourself? No. That’s what every mother does.
Is it summoning strength to confront chemo when it’s your greatest fear?
Is it putting a smile on your face when you are crumbling inside?
Is it speaking the words, “I have cancer” to your children, your friends, your husband, your parents, your in-laws, your brother, and all of the people in your life enough times that eventually it starts to sound normal?
Is “inspirational” when you offer to show your post-mastectomy body to women so that they will know the results just aren’t as scary as they are thinking they will be?
Is it answering everything and anything people want to know?
Is it putting words and feelings in black on a white page?
The essence of inspiration is being strong.
When you least want to be.
When you are faking it.
Strength.
When you lack it.
When you have to dig deep for it.
When your kids need dinner and you want to vomit from the chemo.
When you are too weak to climb the stairs.
And you don’t think you can get through another day.
Or hour.
Or minute.
Or second.
And you just want the pain to end.
Somehow.
Some way.
Any way.
Just have it go away.
When your pride is gone.
Dignity is gone.
All of it.
Being inspirational means being tough.
It means feeling rotten but not wanting others to.
It means wanting to put others at ease with how you are doing.
It means being a lightning rod for everything bad.
A catalyst for everything good.
A spark.
A resource.
A friend.
A wife.
A lover.
A mother.
A daughter.
It means telling your parents you feel okay when you don’t.
A little fib so they will go home and get some rest for the week.
Take some time off for themselves before they come back in 8 days and do it all over again.
A break so they don’t have to see their little girl suffer anymore.
Because 6 days in a row is enough.
For anyone.
Because looking good makes others feel better about how you are doing.
So you put makeup on.
And dress well.
And put a big smile on your face.
So they will think you are feeling good.
And when you switch the topic of conversation, they will go along with it–
They will believe you when you say you are feeling better.
Okay, so maybe I am inspirational. I don’t call it inspirational. I can only admit to the smaller things. The micro things. Inspirational sounds big. Important. It’s hard to accept that one.
But I think I’m convinced.
The reason I’m going to finally concede is that I just realized something:
That was my goal.
Except I wasn’t calling it inspiration.
I was just calling it doing it right.
I was calling it setting an example.
I was trying to show my family, especially my daughter, how you can tackle an obstacle– a big one.
I was just doing my job.
January 4th, 2013 §
 It’s 4 A.M. and I’m up with side effects from yesterday’s Zometa infusion. The monthly IVs to help strengthen my bones are doing their job but I always have one night of flu-like symptoms. Tonight I’ve got numb feet, a splitting headache, and the sweats with a fever. I know it will only last a day. I started round 7 of chemo last night as well. Again I will continue with my regimen of 3500 mg a day of Xeloda split into two doses: 3 pills in the morning and 4 at night. The good news is that even at this slightly decreased dose the chemo is working. My bloodwork yesterday showed my tumor markers again decreasing in the last two weeks.
It’s 4 A.M. and I’m up with side effects from yesterday’s Zometa infusion. The monthly IVs to help strengthen my bones are doing their job but I always have one night of flu-like symptoms. Tonight I’ve got numb feet, a splitting headache, and the sweats with a fever. I know it will only last a day. I started round 7 of chemo last night as well. Again I will continue with my regimen of 3500 mg a day of Xeloda split into two doses: 3 pills in the morning and 4 at night. The good news is that even at this slightly decreased dose the chemo is working. My bloodwork yesterday showed my tumor markers again decreasing in the last two weeks.
Still no appointment to have a repeat PET scan. That will come when the numbers plateau. I am expecting that to happen pretty soon as the numbers have declined a lot, but just can’t keep going down. I’m thinking it will be February for that.
Yesterday was my first time at my local oncologist’s office since they moved back into their fully renovated location. The space is beautiful, there are many changes including the way the chemo room is set up. The social aspect of chemotherapy and its administration is an interesting one. Some people like talking during chemo. Some like watching TV. Some like total quiet. The new setup is more conducive to privacy. While most of the chairs are out in the open, they have curtains, dividers, and positioning that make it difficult to see into the next space and/or talk to any other patients. I will confess I am usually a privacy person. I go to my infusions alone because they piggyback on my doctor’s visit and these particular ones are very quick (actual chemo infusions can take any amount of time. Some are pretty fast, others can take all day. The advent of the iPad and smartphones has made passing the time a whole lot easier).
 The Zometa is not a chemo treatment, it’s just an IV-administered drug. The drips only last 15 minutes once the IV is set and we get started. I have had many occasions to sit with other patients and chat during chemo and Zometa infusions. While initially one who thinks I would rather be sitting alone, I always have ended up happy I had the opportunity to get to know someone else going through this. I always learn something. Of course people are there for every kind of cancer, so frequently I am learning about other cancers and how they are treated. I am (almost!) always interested.
The Zometa is not a chemo treatment, it’s just an IV-administered drug. The drips only last 15 minutes once the IV is set and we get started. I have had many occasions to sit with other patients and chat during chemo and Zometa infusions. While initially one who thinks I would rather be sitting alone, I always have ended up happy I had the opportunity to get to know someone else going through this. I always learn something. Of course people are there for every kind of cancer, so frequently I am learning about other cancers and how they are treated. I am (almost!) always interested.
The new exam rooms have curtains which are woven with the phrase “Speak your truth.” I liked that.I also liked the new chairs. These have a massage button and heating ability! I snapped a photo and captioned it “Love the new chairs: heat and massage. Too bad about the cancer!”
I had long talks yesterday with both of my oncologists (local and at Sloan Kettering). I will share some of those discussions in the weeks ahead.
While the description of some of the chemo experience will be nothing new to those readers with cancer, I will continue to share descriptions of some of the daily routines for those who have had the good fortune to have no idea what goes on inside cancer centers. What I can say is that the doctors and nurses are filled with love. I have a team– from the phlebotomist who has taken my blood for the past 6 years to the doctors to the nurses whose smiles and hugs and concern warm my heart every single visit– I am well cared for and I know it.
 While I was in the chair yesterday I put the final touches on my Sloan Kettering donation page. I will be making a separate post about this experience soon. I am flabbergasted: in the first 12 hours the page has gotten $6500 in donations. This money is earmarked: it goes to metastatic breast cancer research at Sloan Kettering.
While I was in the chair yesterday I put the final touches on my Sloan Kettering donation page. I will be making a separate post about this experience soon. I am flabbergasted: in the first 12 hours the page has gotten $6500 in donations. This money is earmarked: it goes to metastatic breast cancer research at Sloan Kettering.
I thank each person who has donated so far. I am truly astounded at the outpouring of support. Thank you on behalf of patients like me. Thank you to friends and family who donated and total strangers who have too. I know that this is a difficult time of year for many, and making charitable donations may not be in your budget right now. That is just fine. Support comes in many different ways and “free” words I get daily via comments, email, and tweets are appreciated too.
January 3rd, 2013 §
I return to this image again and again: a bookmarked life. This brief post is from May, 2011.
……………………..
One of the defining features of childhood is innocence.
As children we don’t realize that things change. We think the way that things are when we go to bed at night is the way they will be in the morning. We put the bookmark in our lives and expect everything to be the same when we return to it.
Of course, as we grow we realize that’s not true.
That it can’t be true.
That’s not how things happen.
That’s not the way the world works.
And what do we say when someone still believes it? We say he is being childish.
Often times I wish I could retreat to childhood. Not because of how my childhood was, but because I want to recapture that mindset, the one that says that everything is going to be all right. When people tell me “everything is going to be fine” I snort. I recoil. I don’t believe them.
It’s not always going to be all right.
Sometimes it is. Sometimes it isn’t.
But the road you must take to figure it out might break you before you ever find out for sure.
January 3rd, 2013 §
I’m constantly haunted and angered by the language we use with cancer. I woke up in the middle of the night last night and this is what was in my head. I feel the need to caution: please don’t over-interpret this post: my health status has not changed. I’m not stopping chemo or any such thing. I’ve had a few acquaintances die of cancer this month and that’s where this is coming from.
…………………….
People die of cancer every day.
Do you think they didn’t try hard?
Keep their chins up?
Think positive?
Stay strong?
Do their best?
They did.
But it wasn’t enough.
There is no consolation.
Sometimes there is no “getting better” or
“Kicking cancer’s ass.”
Sometimes there isn’t anything else to do but accept the finality.
That’s not giving up,
That’s accepting what is.
January 2nd, 2013 §
When I originally wrote this I tried to think about awareness and what it means to me. I wanted to explain why pink ribbons didn’t mean awareness; I wanted to capture the emotional side of this disease. Readers consistently cite this as one of their favorite pieces. It’s one of mine, too.
Of course some of the things I say here are a bit outdated now that my cancer is Stage IV. But I will leave the words as they are. I still think we are a long way from true awareness. It’s one of the reasons I continue to write.
…………………………………………………..
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
January 1st, 2013 §
I’ve decided rather than just post a top 10 list of readers’ favorite posts, the ones they want to read again, I will be posting the most-requested pieces each day in January. I will still be writing new material; on those days two posts may go out. There is so much material here that most new readers haven’t seen, and I’d love to start the new year off by sharing some of it with them. Readers who’ve been here from the beginning tell me they welcome the opportunity to re-read some of the old work, so I’ll trust them on that since most of my pieces are short. I’ll make a list of the top pieces with hyperlinks so you will be able to easily find them in the future from the website home page.
I do say that it’s very interesting for me to go back and read these knowing that my life has taken a turn since many were written. I wrote them during/after my initial treatment for cancer. Recurrence and/or metastasis was “just” a fear. That fear was real. It motivated me to act a certain way about my health and my life. Those acts obviously weren’t enough because here I am with Stage IV. But make no mistake, the fear of metastasis bears no earthly relationship to the fear that you have when you are told you actually have it, are living with it, are dying with it. No relation at all.
I’ve thought about revising some of the pieces to reflect my new health status but decided not to. They were my truth at the time. My reality now is different, and I document it accordingly.
I’d love to hear your comments as always… It’s been truly gratifying to see how much more response there is now and your willingness to comment and share your reactions to the pieces. Thank you for supporting me in 2012 and let’s see what 2013 brings. I’ll be writing my way through it.
This is one of the most requested pieces. Yes, I really do know people who utter the words, “Cancer is a gift.” And I still am baffled by that statement. The following post, “Cancer is not a gift” was originally written in 2009 and is a response to one such person.
………………………………..
I have a friend who says that “cancer has been her gift.”
She says that it’s been the best thing that’s ever happened to her.
That perspective doesn’t suit me. Despite being optimistic and determined, I am a realist. I see the ugly warts.
I don’t think it’s the best thing that’s ever happened to me; in fact, I wouldn’t wish it on anyone.
A gift is something you want to share.
Something you want to give to someone else.
Something you say “Next time I need to give a special gift to show someone I care, this is what I want to give.”
Cancer is not that thing.
Language matters.
The words we use to describe illness, death, and emotion are important– we should choose them carefully.
Cancer is not a gift:
It’s what you get.
It’s what I got.
It’s a twist of fate.
A happenstance.
A piece of bad luck.
But once you’ve got it, you have to decide what you’re going to do with it.
You can’t give it away, so you might as well make the best of it.
Fortunately, some good comes with it too.
And one of the best parts is the people you will meet.
Just because you don’t think it’s the best thing,
or a good thing,
doesn’t mean you are a negative person
or a bad person
or any particular kind of person.
In fact, it may mean you are a realistic person.
It may mean you are having a bad day.
Or a good day.
Or just a day.
And you will have those days:
Good
Bad
High
Low
Carefree
Despondent
Manic
Depressed
Terrified
Numb
Grateful
Spiteful
Bewildering
Confused
Overwhelmed
Sleepwalking
Drained
Energized
Proud
Embarrassed
And everything in between.
The days are gifts.
You can celebrate the days.
You should celebrate the days.
But don’t celebrate the disease.
Don’t treat it like a prize.
You are the prize.
You are doing the work.
You get the credit.
December 30th, 2012 §

It’s true:
you’d never know.
I look great. I look healthy. I’m not gaunt or drawn or pale.
I wear makeup most days, and some days I ever wear boots with a heel on them.
I smile, I laugh.
I take a slight jog up the front hall steps when I feel like it.
I crack jokes, I roll my eyes when standing in a long line, I gossip with my friends.
I wear gloves a lot, I have to moisturize my feet and hands at least a dozen times a day.
I buff my feet, I examine them for cracks and bleeding. I stick ice packs on them when they burn from the chemo.
I can’t feel my fingertips, yet portions of them crack and peel and are painful and raw.
I can’t hold a pen or twist off a bottle cap.
I take pills all day long.
I’m swollen, I’m tired, my mind can’t stop racing.
I tell time by “on” weeks and “off” ones.
Of course the doctors understand my situation.
They know what this diagnosis means.
Even ones that have nothing to do with cancer call to check on me.
When I go to my sons’ school some of the teachers and moms cry when they see me.
“You look good,” they say. This a compliment. Sometimes they say, “You don’t look sick at all. You’d never know.”
That is shorthand for, “You don’t look like you’re dying but we know you are.”
I hear people in line to buy holiday gifts complain about the sniffly cold they have or the poor night’s sleep their child had.
They might be complaining about something more serious, but still something that can be fixed.
Time will heal what ails them.
I am not so lucky.
I am jealous.
I am jealous that this is their only medical concern.
I’m not jealous of what they wear or the car they drive or the house they live in.
I’m jealous of their health status.
I’m not in denial. This diagnosis is a nightmare.
My life will always be full of chemo and side effects and worry and monitoring and drug refills and hospital visits.
But my life will also be full of great memories, of laughter, of smiles.
There will be tears. There will be pain. There will be heartache.
But there will also be joy, and grace, and friendship.
I don’t know for how long. I don’t know if they will be in equal measure.
They say I look good. They say, “You’d never know.”
For now I know it’s true.
There will come a day when it’s not true.
And they will lie.
And I will know it.
And someday, then, I will know the end is near.
But that day is not today.
December 27th, 2012 §
Sometimes doing everything you can is not enough.
Sometimes your best isn’t good enough.
Sometimes things don’t work out the way you want.
Sometimes it just isn’t fair.
Sometimes the end comes too fast.
Sometimes time won’t slow down.
Sometimes your plans won’t happen.
Sometimes those dreams won’t come true.
Sometimes your life feels like a nightmare.
Sometimes nightmares happen in the day.
Sometimes uncertainty is a needy child that won’t leave your side.
Sometimes there isn’t enough strength.
Sometimes it’s more than you can handle.
Sometimes the end is near.
Sometimes there isn’t anything you can do.
Sometimes staying strong isn’t an option.
Sometimes a word or gesture or deed can bring you to tears.
Sometimes strangers show the kindness that should be shown by friends.
Sometimes you can’t see which way the road will go.
Sometimes all you can do is research, then close your eyes and guess.
Sometimes strength may look like denial;
Sometimes you must trick yourself to get through the day, or hour, or minute.
Sometimes the reality is so unfathomable you must push it aside.
Sometimes the pain is too great.
Sometimes people don’t understand.
Sometimes they make what’s hard even harder.
Sometimes the kindness of friends makes things bearable though,
Somehow the strength of love can keep you going for a while.
Sometimes you get lucky.
Sometimes you don’t.
Sometimes what happens has nothing to do with you.
But somewhere, deep in the darkness, you must hold out hope.
December 22nd, 2012 §
I’ve decided to compile some lists here for readers new and old but I need your help.
I thought it might help new readers if they had a landing point when they first get to the site. Old readers might find posts they’d missed or forgotten, or ones they liked that have earned a second read. That idea blossomed into thinking about posting a list of my own favorites, but realize you as readers might have your own.
As I spend the next few days working on this job, please comment below with nominations you have for which post was your favorite. You don’t have to limit it to one. You can list as many as you like. I’d love to know what “hit home” with you, which ones affected you, or educated you the most. I’ll take those and work them into my lists.
It also is a gift to me to see which ones resonated so much that weeks, months, years later you still remember them. I’d love to know. If there are suggestions for topics you’d like to see me write more about, I’ll take those too. Even if someone else has suggested it, please add your vote… I am trying to see which ones are the favorites.
I think this is a great end of year activity.
I appreciate your readership and input as always and can’t wait to see what you have to say. I’ll be back to you with lists (in some form or another as I see what comes in) by the end of the year.
I wish you all a healthy, happy 2013.
Lisa
December 20th, 2012 §
Today marks the six year anniversary of the day I was first told I had breast cancer. When the radiologist told me the news, she also said she didn’t know exactly what it was or how bad it was.
This is why you do not schedule mammograms or biopsies right before a holiday. Especially Christmas. You’ll be going on vacation… and if you aren’t going on vacation, the doctors, nurses, and pathologists will.
I was told on December 20, 2006 that I almost certainly had cancer based on the mammogram and ultrasound images. I’d need a biopsy to confirm it. But they couldn’t do the biopsy until after the new year. It’s hard to hear, “We think you have cancer. Now go on your vacation and when you come back we’ll figure it all out.” Weeks later I was told I had extensive DCIS and would need to have my left breast removed. I opted to have a double mastectomy. A few weeks later a second look at the slides revealed I had some breast cancer in one of the lymph nodes that had been removed (I am now a big advocate for a second opinion on pathology). I was reclassified as having stage II breast cancer. I had chemotherapy; later, a salpingo-oophorectomy.
Almost six years later, I have now found out that I have stage IV (metastatic) breast cancer (details here).
Yesterday I went to an appointment with my local oncologist. I go to see him every two weeks right now to review bloodwork and to discuss dosing for the next round of chemotherapy which starts tonight.
The concept of “good news” has been completely redefined since my new diagnosis. There is no cure, so I can’t hope for that. There is never going to be a day I am not aware of running out of time. Now “good news” gets defined as stable disease. If you’re lucky, and the chemo is working, good news can even mean reduced disease. Now I hope for that.
I look at my oncologist’s face when he walks in the room. I scan it for signs of what kind of news day this will be. The day he told me about my metastasis I read his face. When he walked in that day I asked him how he was and he said, “Not good.” I assumed it was something about him, his family. I immediately starting worrying about the bad news he was going to tell me about someone else. But it was my bad news. It was my nightmare.
I never used the word cured. I never said it. And I don’t like when others do with my kind of cancer. I always prefer the technical terms NED (no evidence of disease) which means it may be there, but we can’t detect it with the tests we have done. I don’t even like the term “cancer-free” for my particular cancer… again, there might be cancer there, but just not enough to be detected or can’t be with the tools used.
Five years had come and came and gone. Even nurses in other specialties would say at my checkups, “Oh! Five years! That means you’re cured!” and when I’d explain to them that it actually didn’t mean that at all with my kind of breast cancer they would look at me quizzically.
“SEE?! I told you!” I want to go back to say to all of them. I was vigilant for a reason. It “shouldn’t” have happened based on the statistics, the predictions. But it did. And now the only life I’ve got is spent dealing with it.
……………..
I watched my oncologist’s face yesterday. We’ve had some bloodwork results in the last two months that have been a good first step but he hasn’t been willing to budge much on declaring that this chemo is working. One or two data points are not enough for either of us to feel confident, actually. But yesterday we got our fifth data point.
I still have metastatic cancer. That isn’t going to change.
But I have some news I can finally share: my bloodwork is showing “indisputably” (in the words of my doctor) that my cancer is shrinking. The chemo is working. The pills I’ve been swallowing, seven or eight a day for seven straight days at a time, in alternate weeks, are doing what we’d hoped. The cancer is still there. But it’s smaller. But it’s responding. It’s been consistently trending down since I started on Xeloda. Now, with more than a few data points, we can finally characterize the effect and I can share it publicly.
……………………….
So what does that mean? I know that’s the question most will ask. It simply means this is the chemo I stay on for now. It means that I just keep doing what I am doing. I’m not “cured” or “feeling better” or “cancer-free.”
It means that modern science and pharmaceuticals are giving me some time. For today, the cancer is responding, shrinking. And in the land of stage IV cancer, that’s unmitigated good news. Make no mistake, it’s no Christmas miracle. It’s not happening for any other reason than the fact that I am aggressively taking as strong a dose of this drug as I can tolerate, and it’s doing its thing.
Six years ago I went on Christmas vacation and feared for my life. I was scared and confused and miserable. Now, six years later I’m in a much worse place vis-a-vis cancer but my mindset is different.
I’m coming to terms with accepting the life I have — the one I thought I’d have is gone. I have created a new one. The best one I can.
For today, I celebrate the good news. I will go to my children’s school holiday parties. I will smile. I will make memories. I will not focus on side effects. I will find beauty in something small.
I will savor the things I can do today.
December 15th, 2012 §
I’m re-posting this piece today in light of the school shootings nearby in Newtown, Connecticut. I know there is a lot of material out there this weekend on children and grief, but I’d like to add mine as well. This post was originally written a few days after my mother-in-law, Barbara, was killed suddenly in a car crash in 2009. I think these observations apply now, too.
I will honor childhood today.
………………………………………………….
Children are different.
From adults.
From each other.
I had to give two of my children different directives this morning:
One I told, “It’s okay to be sad.”
One I told, “It’s okay to be happy.”
I needed to tell my 7 year-old son that it was okay to cry, to be sad, to miss his grandmother.
I miss her too.
And it’s okay to let your emotions show.
It doesn’t make you a sissy or a wimp.
What it does make you is a loving grandson.
A grieving boy.
A bereaved family member.
But my ten year-old daughter needed a different kind of permission slip today.
I sensed she needed permission to smile.
To laugh.
To be happy.
I needed to tell her that it was okay to forget for a moment.
Or two.
To forget for a few moments that Grandma died.
It’s okay to still enjoy life.
The life we have.
Grandma would want that.
I told her that Grandma loved her so much.
And was so proud of the person that she is.
I reminded her how Grandma’s last phone call here last Sunday was specifically to tell Paige how proud she was of her for walking in a breast cancer fundraiser with me.
It’s okay to still feel happiness.
And joy.
It’s okay to let that break through the sadness.
Children are different.
But they take their cues from us.
I know my children.
I know that this morning what they needed from me was a sign that it was okay for them to feel a range of emotions.
It’s healthy.
Because what we are living right now is tragic.
And confusing.
And sad.
And infuriating.
If it is all of those things for me,
It can only be all of those things and more
To my children.
December 14th, 2012 §
It has been ten weeks since I was diagnosed with stage IV breast cancer. After I was diagnosed the first time with cancer in 2006 I began to mark time in a new way.
The parent of a newborn starts with days, then weeks, then months and fractions thereof. “How old is the baby?” a parent is asked. “He’s 5 days old” or “11 and a half weeks old” or “16 months,” the reply will come. But when that child is a teenager no one will mark his age in days and half weeks and months. The importance of those fractions will fade. Once he’s got years under his belt their significance is muted.
Time now gets marked in rounds of chemo, time elapsed since diagnosis, months without disease progression. There’s always a mental countdown, a cognitive calculation going on.
I find myself obsessed with time in a new way, but also rapidly losing track of it. Granted, some may be chemobrain. I wonder now that I am on chemo for the rest of my life what it will mean to my brain. It’s a necessary evil, but concerning. The chemo that kills cancer cells is also killing brain cells. New evidence shows the reality of this condition, no longer a punchline or mere excuse for forgetfulness.
I always encourage people with cancer (and any illness) to keep a calendar of their treatment. There is so much to keep track of that having an easy reference point is good. When did you change doses of medications? when did you see certain side effect symptoms? Jotting them down in a calendar or noting them in a smartphone calendar can be helpful. Sometimes on paper, patterns will emerge.
Grief is such a wily companion. Like smoke it creeps into places when offered only the tiniest access point. Grieving the life we thought we’d have is important. It’s easy to say, “lives don’t always go the way we plan” but that undermines the emotional complexities of dealing with serious illness. Just because things don’t go as planned for many of us (most of us?!) doesn’t mean there isn’t a serious adjustment to make.
“Roll with the punches” and “live in the moment” are deceptively simple phrases of advice that are not only absurdly emotion-free but also easier said than done. More than once in the past few weeks I’ve challenged people whose best words of support have been to live in the moment. While I understand the ideology, and agree with the premise that we must enjoy the time we have, I defy anyone without a stage IV diagnosis to tell me that it’s the quality of your years, not the quantity of them. These are things that healthy people say. Yes, quality matters. None of us want to suffer. I don’t. But years count, too. “Living in the moment” can imply that the grief process should be squelched or has an expiration date. Anyone who has experienced grief knows there is no expiration date.
Of course none of us knows our future. Some people try to tell me they don’t know their future either; they could get hit by a bus tomorrow. I love the response that Jen Smith suggested, “Would you like to trade odds?”
Acceptance of reality must come. Dwelling on the dark side of diagnosis won’t lead anywhere productive if dwelling is the only thing one does. I think that is the real meaning behind the idea of focusing on today. The acceptance of reality does come. Of course, that’s complicated when what the reality of what one’s prognosis is unknown. I have quickly built up tolerance for discussing the most serious and unpleasant ramifications of my condition. I occasionally sleep through the night. But I don’t know how long it will take to wave goodbye to my children in the morning, or tuck them all in at night, or talk about the future without feeling pain with the joy.
I mark the time. I’m back to being someone who counts the months and weeks and days. Counting them, appreciating them, grieving them. All at once.
December 12th, 2012 §
Tuesday’s visit with my oncologist at Sloan Kettering was informative, as always. However, the big question can’t be answered: what is the trajectory of my stage IV cancer?
There will be no answer to that for now.
We start with a chemo. We see (through bloodwork and PET scans) how the cancer responds. If it responds, I stay the course until the treatment stops working or the side effects become untenable or dangerous. There is no way to know how long that will be. Any particular chemo could be ineffective from the get-go. It could fail after months. It could fail after years. Then you go to the list of options and decide on a next chemo regimen. This decision is not always easy; you can’t know which one will be best for you. It is often educated guesswork at best. There can be many chemotherapy options and in the end, I will probably try many/all as each one eventually fails. I’ve talked to women who have gone through more than eight different chemos in the treatment of their metastases. One thing I know is that chemotherapy in one form or another will be a part of my life for the rest of my life.
There is also no way to know if you will tolerate a chemo regimen well. Side effects can be dangerous and variable. Sometimes side effects are serious enough that you must discontinue using a particular drug even if it’s effective in reducing the cancer. As you can imagine, this can be a heartbreaking proposition: find something that works but you are unable to take.
As you know from my last post I have been struggling with HFS (Hand/Foot Syndrome) from the current chemo, Xeloda. I had done some research and found some studies indicating that the selective COX-2 inhibitor and anti-inflammatory drug Celebrex has been used with some success in helping reduce the severity of HFS in patients taking Xeloda (and a few other specific chemos). I had reduced my daily dose of chemo from 4000 mg to 3500 mg for this 5th round (7 days on, 7 days off) to see if the HFS improved with a slightly lower dose. Of course it’s scary to reduce the dose of your chemo but I’ve tolerated the maximum dose for a good number of rounds. It’s normal to need to reduce the dose as time goes on.
My oncologist agreed that the Celebrex was a good thought and definitely might help the HFS. There are risk factors associated with the use of the drug but we both agree that it’s worth the small risk. So I am starting with 200 mg once a day to see how I tolerate the Celebrex and if a low dose helps I will stay with that. If needed, it can be increased to 200 mg twice a day. My hope is that the Celebrex helps the HFS and allows me to go back to the higher 4000 mg (8 pills) a day chemo dosing for the next round.
In the meantime I continue with frequent moisturizing of my hands and feet (at least 10 times a day) with a variety of lotions including shea butter, Eucerin, Aquaphor, and more. I stay away from water, do not apply heat on hands/feet, wear socks and soft shoes/slippers, and wear gloves as much as possible. My feet have been doing very well, my hands holding steady and actually do seem improved today. Here’s hoping!
I know this was a technical discussion today but I want to share it for other people in treatment who might be able to ask their doctors about Celebrex if they suffer from HFS with Xeloda. I also hope that the explanation of chemo and prognosis will be informative.
I continue to do as much as I can everyday and when people see me and say, “You’d never know what you’re going through right now,” I take it as a compliment. I was busy today with routine dentist and endocrinology appointments… you can’t ignore the rest of your body when you are treating cancer. Many other body systems will be affected by the cancer and chemo. My thyroid has been holding steady but shows signs of needing another medication adjustment. Bone treatments like the Zometa infusion I take can cause problems with jaw bones. It’s important to keep a watchful eye on your whole body and not use cancer as an excuse for ignoring routine checkups. That’s my loving nag for the day… stay vigilant with your healthcare appointments and thanks for all of your support.
December 10th, 2012 §
I wake up in the middle of the night with a start:
Heart racing, breathing fast.
It was a dream, I soon realize. What I fear is not true.
The despair, the nightmare, the horror.
All of it was a creation of my mind.
In the dream I was searching for him.
He was gone.
He just disappeared.
My child jogged off into the woods, his identifiable gait
Seen from behind,
Tennis whites lit up the woods–
But where was his racquet?
I realize now in the dream he didn’t have it.
He ran off never to be seen again.
Did not get to his destination.
I searched. I could not find him.
I failed him.
I quickly erase the fiction from my mind,
It’s not true I tell myself:
It’s a dream.
Focus on something else.
It’s 12:56 AM.
My heart settles back to its rhythm
I hear the rain,
My children are safe in their beds.
I can relax now.
But ease does not come.
My fear is misplaced.
The nightmare still persists.
The reality is a different image.
There is a nightmare.
A waking one.
One that’s real and true, one I cannot shake off with time, or more sleep, or distraction.
My nightmare is loss, it is my children out of my grasp, it is separation.
I still fear all of those things.
But it is I who will wander off into the unknown
Leaving others behind
Waking in the middle of the night with only an image of me,
Fleeting,
As they search for me in vain.
I will be there, with them, but only in memories.
It will have to be enough.
But I know it won’t be.
After all,
This is what cancer nightmares are made of.
This is what grief does.
I cannot do more, be more, than I am right now.
But I can want more.
It is a parent’s prerogative.
I am greedy.
I make no apologies for wanting to see the things I want to see,
Wanting to share the things I want to share,
Wanting to live the life I want to live.
This is what I want.
This is what I hope.
This is what I dream.
 It’s been a wonderful but long few days. I was so run down yesterday that after our egg hunt I got into bed and pretty much didn’t get out for 9 hours. Tristan’s birthday was absolutely delightful. We held a birthday party, something he’s never had before. We’re not big on parties in our family; instead, we always have small family celebrations.
It’s been a wonderful but long few days. I was so run down yesterday that after our egg hunt I got into bed and pretty much didn’t get out for 9 hours. Tristan’s birthday was absolutely delightful. We held a birthday party, something he’s never had before. We’re not big on parties in our family; instead, we always have small family celebrations.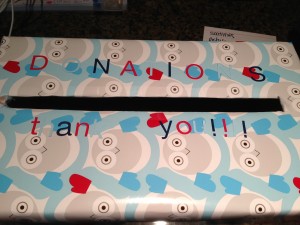 We put a donation box out at the party and everyone can stuff the box. This year Paige wrapped and decorated the shoebox. The children who are bringing the donations also get a lesson in the joy of giving to others. Often the parents tell me that their children don’t understand why they can’t bring a present. That’s okay with me, I think it’s fine to force a discussion about giving to those in need. My children take pride in doing something good, and even when they are young and want to know why guests can’t bring gifts, I feel no guilt in explaining that not all children can afford to pay for the operations they need. When parents say to me, “Oh, I would love to do that but I don’t know how my child would respond,” I never quite understand that. It’s our jobs as parents to be role models, to show our children what’s important.
We put a donation box out at the party and everyone can stuff the box. This year Paige wrapped and decorated the shoebox. The children who are bringing the donations also get a lesson in the joy of giving to others. Often the parents tell me that their children don’t understand why they can’t bring a present. That’s okay with me, I think it’s fine to force a discussion about giving to those in need. My children take pride in doing something good, and even when they are young and want to know why guests can’t bring gifts, I feel no guilt in explaining that not all children can afford to pay for the operations they need. When parents say to me, “Oh, I would love to do that but I don’t know how my child would respond,” I never quite understand that. It’s our jobs as parents to be role models, to show our children what’s important. Invitations and stickers from Easton Place Designs and the most adorable cookies from One Tough Cookie helped to make the day special. Tristan loved his karate party, and I love that I’ll be sending a big envelope to Shriners Hospital in Philadelphia from Tristan. I am so grateful to the families who helped to make this birthday so special for Tristan. I thank them on behalf of the children who will benefit from their generosity. Everyone does what’s right for them. This type of birthday celebration is what feels right to me.
Invitations and stickers from Easton Place Designs and the most adorable cookies from One Tough Cookie helped to make the day special. Tristan loved his karate party, and I love that I’ll be sending a big envelope to Shriners Hospital in Philadelphia from Tristan. I am so grateful to the families who helped to make this birthday so special for Tristan. I thank them on behalf of the children who will benefit from their generosity. Everyone does what’s right for them. This type of birthday celebration is what feels right to me.






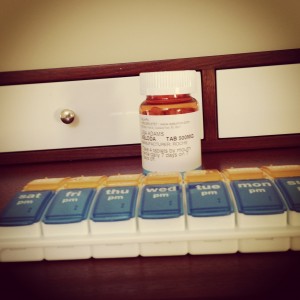










 Link to Twitter
Link to Twitter