November 24th, 2012 §
I can see how isolating metastatic cancer can be already.
It has become hard for me to be around other people.
I find myself hiding as much as possible.
When I am in the company of others my mind wanders.
I can’t focus. I feel the need to retreat.
For the time being I just can’t relate to others’ lives which only 6 weeks ago were so similar to my own. Now… we are a world apart.
It’s not their fault. It’s just that circumstances make it so that I am selfish. I try to conserve my energy as much as I can.
Already I can see relationships suffering. There is a fine line between giving space and putting distance. Some are already dropping away, and we’ve only just begun. Others have risen to the occasion and helped more than I could have dreamed. Only true friendships are going to make it under these circumstances. Sometimes the isolation comes from being shut out. Sometimes it comes from locking yourself away.
Phone calls go unanswered, emails often do too. Thank you notes don’t always get written, social commitments get canceled or never scheduled in the first place.
I know that people cannot truly understand.
I don’t want a support group right now because metastatic cancer has a wide range of outcomes. I don’t know if I will be in a rapidly progressing group or not. I don’t know whom to look to that is “like me.” There is no way to know which group I will be in, who my peers are.
Right now I am very sensitive to death, to pain, to suffering. It’s very hard for me to see right now. I’m too raw. I just don’t think I’m ready for a group. But I won’t say I never will be. I need to talk to my oncologists about whether they have patients like me.
It’s difficult to listen to people complain about trivial things, normal things, things I was complaining about two months ago.
Now those complaints just annoy me, or make me sad.
I want to scream, “I want your problems!” And I do. I want that life back. I want to turn back the clock. I just don’t want it to be this right now.
One of the things that bothers me the most about this disease is the knowledge that the way I feel right now is the best I will ever feel for the rest of my life. It’s only going to get worse. That thought terrifies me.
When you feel crappy you want the time to go faster. You just want to get through it.
The problem is that what you may not have is time.
It’s a conundrum. You want the time to pass, but this is the only time you have.
I know so many people say, “No one ever knows how much time they have. You have to make the most of every day, of every moment.” I know that’s true. But the knowledge that there is something identifiable in your body that is a threat, is most likely to be that which kills you, bears a different weight. Of course the doctors don’t know exactly how much time it will be. There is no crystal ball.
Everyone tells me the stories of friends and relatives who were told they only had months and years later they are still alive and doing okay. I am told these stories every single day. I get it. I do. And I love them, they give me hope. But often those people’s diagnoses and particulars bear no relation to mine. Additionally, there are also stories of the people in the other group, the ones who thought they had years and didn’t. People probably have the good sense not to tell me those stories. But they are out there. It’s not that I focus on the negative. It’s not that I necessarily think I will be in that group. But anything is possible. On both sides.
The part that scares me: I’m only at the beginning. I hope that I will get stronger, gain acceptance as I get used to this diagnosis. But I’m not sure about that. I truly believe I could handle this better if I didn’t have so much worry about my children and what effect this will have on them. I wish I could protect them, shield them from this agony.
There are good days and bad days. I must do my best. But being the one everyone is watching takes a toll. Everyone will take their cues from me. I will set the stage for how my friends and family will deal with this: how I handle metastatic cancer matters. I am laying groundwork. I must do it right.
Some days that is an overwhelming task.
“Doing it right” doesn’t mean I have to be positive all the time. Doing it right means I have to be honest. It means I get up each day and do the best I can. For myself, for my husband, for my children, for others who may have cancer and those who will get it. It’s okay to be scared, and angry, and sad, and everything else.
It’s all part of this.
And for me, so is sharing.
November 21st, 2012 §
I load the dishwasher, put in a load of laundry and buy Colin a new white dress shirt
Because I can.
I walk the two blocks between the doctor’s office and the drugstore on a crisp autumn day
Because I can.
I give my children an extra hug, just one more kiss, an additional “I love you” before the bus
Because I can.
But still I worry about today, tomorrow, and the next day.
How can I not?
I put makeup on yesterday.
I can tell it puts people at ease.
If I look “healthy” then they can relax.
If I don’t look sick they won’t have to worry how to act or what to say.
They tell me “You’d never know to look at you. You’d never know you have cancer. You’d never know you’re sick.”
Some moments that’s true. Some moments I feel good. Some days, in fact. And I treasure those.
Some days it’s a lie. It’s not how I feel.
I know it’s a compliment. I take it as such.
The phlebotomist asked me at my oncology appointment yesterday if I’m ready for Thanksgiving.
I wasn’t sure whether to cry or laugh.
Ready?
I don’t know.
Giving thanks. That’s a loaded phrase.
I am grateful I have some time. I am thankful for the kindness that gets shown to me every day by my family and friends.
I appreciate every person who tells me they are lifted by my words, learn from them, say they express something they have felt or even just wondered about.
For every email I get of support,
Every offer of help,
Every playdate,
Every Facebook post, photo, comment
I give thanks.
But cancer sucks. This diagnosis is my nightmare.
But I also know that tragedies happen to people every single day. A life can be lost without warning. I have learned of two sudden deaths of friends’ loved ones this week and I see the pain those losses have caused. I learned it for myself when my mother-in-law died. She did not have time to say her goodbyes.
I don’t like that my life revolves around this disease right now. I try to keep my life focused on others as much as I can. I try to check in on friends who have their own troubles. I try to keep up with the kids. I try to be a good wife and keep the house running. I wish I could be a better wife right now. I try to be strong. I try to suffer on my own time. I try at these things but don’t always accomplish them.
It’s an isolating predicament. Few can know the anguish, the daily trials, all of the parts of my life which don’t get shared with anyone. I share some here, of course, and with friends, but much of it is my own. For now, this is how it needs to be while I continue to process and try to make sense of this new chapter.
Thanks to you all.
…………………….
I was honored to be featured in this blogpost from the American Cancer Society titled “Cancer survivors are truly remarkable people” which focused on the post I wrote in the days after my diagnosis giving tips on how to talk to children about stage IV cancer.
……………………..
Many have asked about the fractures on my left side. The one that is painful is the one in a rib up near my collarbone. That will probably take two months to heal. It is a fracture caused by cancer in that bone. The cancer must shrink first. Only then can the bone heal. So it will be a slow process.
I start round 4 of chemo tomorrow, on Thanksgiving night. Same full strength dose because I was able to tolerate the last round again. Same regimen: 7 days on, 7 days off.
November 15th, 2012 §
Each day is different. Each moment, too.
It still seems surreal, this diagnosis of metastatic breast cancer.
It’s strange how quickly the horrific can become regular: the chemo, the side effects, the new routines.
Oncology appointments, IV infusions, medication refills all start to fill my calendar.
I start making lists of things I need to do. I prioritize them.
It’s not always about what’s actually the most important, it’s also about finding things that bring me small moments of joy.
The small moments are the ones that bring tears to my eyes. Tristan’s little voice saying, “I love you, Mama. You’re the best Mama in the whole wide world” is enough to make me misty.
I still lose my temper. I still yell sometimes. Often it’s misplaced anger, a manifestation of my frustration with my situation.
I haven’t suddenly turned into the world’s most patient person. Sometimes cancer makes me the most impatient one, in fact. I feel the clock is ticking. I don’t have time for nonsense. But that’s not a way to be. I will still try to be better.
I try to be the one to do things with my children as much as I can. Even if there is a babysitter in the house Tristan always reads to me at night for his homework: that is sacred. I still save artwork and photographs and remind them to brush their teeth and clean their rooms.
I try to do the little things: helping Colin with a school project, keeping Paige company while she does homework, watching a sports practice if I can. I go to the grocery store and I work on the holiday card. I still take pleasure in getting the stubborn stain out of Clarke’s dress shirt that the dry cleaner couldn’t.
My motto is that I will do as much as I can for as long as I can.
I don’t ever have a moment that I forget about my cancer. I think that’s the part about it being new. Even when I was diagnosed the first time — even after I finished chemo and surgery and all of it– it still took at least a year for me to be able to push the daily fear down. Of course now the fear has been realized. I am living it. I am living my nightmare, one many people share.
And yet, the morning comes.
I see the light of day and I get out of bed. I see the faces of my children. I kiss my husband goodbye when he leaves for work. Each day I have is a day that matters. Each day is one to make a memory with my family and friends.
Each day is one more than I had the day before.
But let’s be clear: there is no joy in this disease.
My appreciation for my days should not be interpreted as supporting the nonsensical idea that “cancer is a gift.” There is nothing positive about this disease; I would give it back if I could. I did not need cancer to show me the value of things. I always knew these things were true. I never took them for granted. I knew what demons could be lurking.
I did all I could. It was not enough to keep it at bay. But maybe, just maybe, I can keep it at bay for a while.
I still haven’t fully come to terms with what this diagnosis means, but that’s because there’s no real way to know. We don’t know enough yet. It is the uncertainty that is the most difficult part for me. Will this chemo be the one that lasts for a while? Will it fail? When? What next? How long with that one last? My body holds the answers, but it’s not showing its hand yet.
I have to learn to ride this roller coaster. I’m just not there yet. And I don’t really know how long that is going to take.
I walk past people on the street and know they have no idea what is going on inside my body.
People in front of me in line at the gas station don’t know there’s chemo in my purse.
I look like everyone else. I have hair on my head. I ask the checkout person to pack the bags light because I can’t carry anything with my left arm now (the cancer has fractured two ribs on my left side).
Sometimes I want special treatment. I want a Get Out of Jail Free card. Most of the time, however, I want to stay home. Hide out. Be invisible.
I’m still processing. Reeling. But while I’m doing that I’m living.
November 12th, 2012 §
I had the honor of being interviewed by Julie Klam, Ann Leary, and Laura Zigman today on their radio show “Hash Hags.” I’m such a fan of the show and of these three authors; I always save the podcast to listen to while I fold laundry because it makes mundane tasks more fun. The truth of the matter is that I have a lot to say, which I guess is how I have written over 120,000 tweets. I think I will always be talking, sharing, asking, listening.
I really enjoyed being interviewed but of course I’m now kicking myself thinking of all of the things I wanted to say and didn’t. And of course, I love to talk about non-cancer things too.
Unfortunately, subjects like friendship during illness (especially relevant given Julie’s new book Friendkeeping) and how to help children deal with a parent’s illness just were too big to get to today. I also plan to write about these subjects more in the weeks ahead. Also, I will be writing about friendship and hope to get Julie here for a Q&A too.
If you’d like to listen to Hash Hags, click here.
………..
Tuesday I’ll be at Sloan Kettering to meet with my oncologist there to talk about how I’m doing on chemo, side effects, and the plan for the next month. I’m midway through the third round and doing well. I felt really good today and am glad for that.
November 9th, 2012 §
Started chemo again last night, counts were good and side effects tolerable enough that we’re doing full strength again this time. 2000 mg Xeloda twice a day for 7 days, then 7 days off. The side effects are usually worst on days 4/5 through 9/10. Fatigue, stomach pain, GI upset, nausea, loss of appetite are the worst. Hand and foot syndrome is to come but haven’t had problems yet.
My potassium is low this week and my dad had a great suggestion for this (especially when eating is difficult). Low sodium V8 is packed with potassium. It has twice as much as regular V8. If anyone out there needs a good source, the low sodium stuff is it!
I’ve given up nailbiting and am shocked that this was the month I was able to do it.
I’ll be back at Sloan Kettering in a few days… and hopefully soon will be able to write more creatively again beyond these boring treatment updates. I know so many of you aren’t sure whether to contact me or leave me alone, but I hope these updates at least let you know the basics. It also always lets me thank everyone for the many ways you are helping me right now.
xo,
Lisa
November 5th, 2012 §
A very short update because I have not updated for a while. We were hit by Hurricane Sandy and are still without power after 8 days. We are waiting for a Nor’easter to arrive on Wednesday which may cause further damage. A tree hit the house, fortunately came to rest on the chimney which prevented us from having the tree through the roof. The kids were out of school all week which was challenging since it was my week on chemo. But we got through it. My parents came and rode out the storm with us and I am so grateful for their help. They aren’t married anymore but they really do come together to help me, which is just what the kids and I needed.
We’re waiting for power to return and tomorrow (Tuesday) I will be back at the oncologist’s office (temporarily relocated because a lot of Greenwich is still without power as well). I’ll do bloodwork, meet with my doctor, and then get an IV dose of Zometa to help strengthen my bones and hopefully reduce some of the pain I am still having in my left shoulder from the cancer-caused fracture. I should probably wear a sling to help with the pain but I refuse to do it because I know it will cause so many questions of “What did you do? How did you hurt yourself?” I just don’t want to talk about it.
So many have been affected by this storm. My heart goes out to them.
I have a hard time right now dealing with the fact that once we get through the immediate cleanup from this storm I will still have this blasted cancer. And be dealing with it. Forever. And right now that is something I am having a hard time dealing with.
I do as much as I can each day to be normal… I went to the laundromat during the power outage. I did the grocery shopping today. I play Yahtzee and give snuggles. I don’t have energy to do as much as I want. I still ask for help. I have friends who’ve offered so much assistance and I am grateful. I am loved and I know it… I just am working through the mental anguish of this diagnosis.
I long for problems that can be fixed. I long for problems that have solutions.
October 27th, 2012 §
Today is day 3 of the second round of chemo. My blood counts were good this week and I was able to go ahead with full-strength dosing of 2000 mg of Xeloda twice a day for 7 days. Side effects need to be monitored each round to see what dose I can take each time.
I’m tired after a very active week. Tomorrow (Sunday) is Paige’s 14th birthday. We have a giant Crumbs cupcake waiting for her birthday dinner tomorrow night. My friend Alex is bringing over a special meal of her favorite foods from The Rye Country Store so it will be ham and other assorted treats for everyone.
She likes when I tell her stories about her babyhood/childhood. I’ve decided to finally give her the scrapbook I kept for her during the first few years of her life (okay, fine, until Colin was born and I didn’t have time for that anymore!). It has photos, letters I wrote to her every few months about what she was doing and how we spent our days. I think she will love it. Tonight I will read each letter and page through the book.
We’re in Hurricane Sandy preparation mode. I’ve got two refrigerators stocked, generator propane tanks filled, case of oil for generator, porch furniture moved, flashlights galore, batteries, water, etc. I’ve done as much as I can to be ready and yet still I feel unprepared.
It’s all about control. Loss of control is a tough one. There’s been a lot of that around here lately. I try to give myself ten minutes a day where I cry and lash out at what is going on. I let it out, and then I move on. There’s no other way to be in my mind. To focus on the negative only ruins the days. I need to keep reminding myself of that.
I try to do as much as I can to be “normal”… to do the things I usually do like some laundry and grocery shopping and going to Tristan’s karate class. It helps the kids to feel that things are going okay and also keeps me distracted. My motto is “I’ll do as much as I can for as long as I can.” That is how it’s going to be.
I don’t know what the storm will bring to us and to so many of you in its path. I hope we will all be safe. My best to you all for minimal damage and disruption. As always, thank you for your kindness in all of its forms.
xoxo
October 24th, 2012 §
Back to the oncologist on Thursday to talk about round 2 of chemo which also starts Thursday night. I’ll have my blood counts checked and we’ll talk about how I tolerated the first round. Frequently people can’t tolerate “full” dosage of the chemo for more than 2-3 rounds and they have to reduce the dose by 25%. I tolerated the first round reasonably well so I’m interested to see if we will be going full strength into the next round. I assume so.
It’s too soon to have any tumor marker tests show whether the chemo is working or not, so don’t expect any news about that yet. That will take weeks, perhaps many.
I am so grateful to friends who have been helping with playdates, rides, groceries, errands. I cannot tell you what it’s meant to me, especially during this very atypical few weeks. Thank you to everyone who has sent a note, email, treat, etc. It’s been overwhelming. I just can’t acknowledge them all the way I’d like (long handwritten note on gorgeous stationery) but please imagine that in your mind, because it’s what I’d send each of you if I could.
October 24th, 2012 §
To my dearest children,
Someday you will understand the depth of my love for you. Perhaps it might take until you are adults, perhaps made more vivid if you are fortunate enough to have children of your own. No matter when, no matter how, I hope you will someday learn this powerful emotion I feel for you. You give me strength. You make me fight. You give me joy. You make my heart swell with pride.
I want to see it all. I want to see every day. I want to know every phase of your lives.
You see, I am a quitter.
I know, those of you who know me are probably chuckling and saying, “Yeah, right.”
It’s true.
There are very few things I’ve finished that I have started. I think I was always afraid of not doing something well. I would start and quit… or just not start at all.
But let that be a lesson: there is no such thing as perfect. Try. Fail. It’s okay. Take a chance. You have no idea where it might lead.
Hard work doesn’t always pay off. People don’t always get what they deserve. That’s just the way it goes.
I didn’t finish my Ph.D.
I never wrote a book.
But my darlings, let me tell you something I take pride in: you. Parenthood is a lifelong commitment. There is no backing out, changing your mind, saying “it’s too much.”
There is one job I’m good at and it’s being your mom (I’m a pretty good wife but I do tend to nag even though it’s for your dad’s own good). Your flaws and your talents make my heart soar in equal measure… they are what make you you. You are each so different, so unbelievably deliciously divine in your own way. Never doubt that my heart bursts every time I look at each of you. I’m pouring every ounce of love into you that I can. I’m going to just keep doing it every day.
Being your mom is the best thing there is.
October 19th, 2012 §
I’m doing quite well after first week of chemo. Today is my first full day off and I’ll start up again next Thursday night. I only have a few minutes to update you but I know I’ve been so quiet this week and usually that makes people worry!
I want to say that everywhere I’ve gone for medical appointments this week I have doctors telling me stories of patients of theirs who have been living with metastatic breast cancer in their bones for years (and in some cases, “years and years”). Until proven otherwise, that’s the group I’m putting myself in. Anyone who knows me knows I’m the biggest realist (and skeptic) there is. But right now I’m going full steam ahead and trying to recalibrate my life to this new normal. My body will be doing lots of work and I know I won’t be able to do everything I want to. I’m already accepting help so much more than I ever have. For now I am hoping that it helps others to be able to do something practical and useful for me instead of feeling helpless… since I know feeling helpless is a terrible feeling when watching a friend or loved one go through a difficult time.
I won’t talk about side effects today, I won’t talk about negative stories today. Today is about the stories of women with this disease who are living with cancer. That’s my story.
…………………………
And a few links for you non-Twitter folks who might not have seen:
Author Laura Zigman and her Xtrafrenemy videos make me laugh. She made one for me. You can watch the YouTube video here. I’ve heard of Lisa Adams! (Laura, I miss you… thank you for the gift of laughter).
Also, Media Bistro did a really nice piece this week on me. You can see that here.
October 17th, 2012 §
My Twitter friend @thatneilguy (Neil Shurley) put together this sweet and tear-jerking YouTube video for me with photos from friends. He even wrote me a song to go with it. Then he created a Facebook page for me so I could see all of the photos individually.
I appreciate the love and attention so much from everyone and will need it in the days ahead. I’m dealing with chemo round one at moment.
Today is Wednesday. I have 2 doses today, one tomorrow morning, and then a week off. Side effects may not really go away in between. I’m learning as I go.
Here is the video of We Love You, Lisa … take a look
and the FB page is here .
I hope to be back doing some “real” writing soon, but for now short updates will have to do.
Go out and find beauty in something small today: a leaf, the sky, a hug, a kind word or deed. Go do it. For me. Because you can.
(okay, and while I’m nagging, make that healthcare appointment you have been putting off. Stay as healthy as you can. Be vigilant. #mondaypleads)
xoxo
lisa
October 14th, 2012 §
Thanks to Annie at PixelCurrents, Inc., I now have a “Tweets” tab on my home page. If you don’t tweet and want to see what I’m saying throughout the day, you can always check that page. Hopefully this will also help reduce the number of updates needed.
I’m on day 4 of chemo, hanging in okay. Should start feeling more effects in next 48 hours. Awful fatigue, painful/sensitive/cracking hands and feet and some other things are to come.
Sold tickets at the school carnival for two hours yesterday which was fun and normal except for the part where some people looked at me oddly or started crying when they saw me. That’s hard to take. Things like “chin up!” aren’t particularly helpful nor is “Everything happens for a reason” or “You’re only given what you can handle.” Attitude isn’t always everything. Genetics can trump all. I fight with science. My old post where I asked people to tell me the strangest thing someone said to them about cancer is getting some new comments. You can read the post and add your comments here. Some of them are jaw-dropping.
Please don’t send me suggestions of things like ozone treatments or anything like that to cure my cancer. I’m not interested. Don’t tell me about your relative or friend who died a long, painful death from this particular disease. That’s not helpful, though I’m sorry they had that experience. It’s not that I’m insensitive, but when you’re scared, what you don’t need are people telling you how bad it’s gonna get. Hearing details of a death from the condition you have — I’m not ready for that yet. I know most of what’s ahead. Trust me. And if I don’t… just let me learn it for myself. Also, “Rah-rah! You’re going to beat this! Stay strong and chin up!” doesn’t do much.
I know that people don’t know what to say. In most cases I know their hearts are in the right place. I don’t share these quotes to shame people. I share them to educate, to help teach people comments that might be interpreted by people with cancer in a particular way.
Throughout the last five years everyone always asked me, “why don’t you just move ON?” When they said “You’re done with treatment, go live your life. We think you have a long and healthy life ahead of you” I could not. I was always vigilant with my health.
I was right. And so was my oncologist. Five years doesn’t mean cured. There is a reason why I never said I was cured and THIS IS IT. I’m told I had a single digit chance of recurrence. Statistics were not on my side. I’ve always been an outlier. In the negative.
This one time, though, I am doing what I can to be an outlier in the right kind of way. Let’s hope this works and gives me lots of time.
As always, I appreciate the concern and offers of help I receive every day. I am loved, and I know it. I don’t take it for granted.
October 11th, 2012 §
 Ten hours, 2 oncologists, 2 hospitals, 1 IV infusion of Zometa, one blood draw, one knock-down drag-out fight with insurance, and first 4 chemo pills taken. That was today.
Ten hours, 2 oncologists, 2 hospitals, 1 IV infusion of Zometa, one blood draw, one knock-down drag-out fight with insurance, and first 4 chemo pills taken. That was today.
I don’t feel well enough to write out everything, but I do want to do a quick update because I know so many are wondering and I can’t address all of the messages individually.
My brain MRI came back clear. I found out when I was in my meeting at Sloan Kettering. Tears of relief.
After a two hour chat with my oncologist there I made some treatment options.
I will do monthly infusions of Zometa to strengthen my bones. Side effects have started already from this and are worst on the first dose. Flu-like symptoms including bone pain, fever, joint pain, etc. should sideline me for the weekend.
My chemo regimen will start with Xeloda. It’s an oral chemo, in which I take 4 pills in the morning and 4 at night. I do this for 7 days. Then I get a week off. Usually days #5-10 are the worst for side effects. Fatigue will be bad. I will not lose my hair.
I will do these two things and we will do bloodwork at one month to check my tumor markers (CA 15-3 and CA 27.29). They may not go down right away even if the chemo is working. It may take another month or two to see that. Also, there is a mechanism by which when you start attacking cancer it may temporarily make the tumor markers go up. So, you can’t put stock in the first month’s blood levels. I happen to be one of the 2/3 of patients who actually show elevated tumor markers during a metastasis. In 1/3 of cases, patients with metastatic breast cancer will not have elevated levels. So bloodwork will be one tool I can use to monitor this process.
My ribs can’t heal until the cancer is reduced. But the Zometa may help with the pain.
I will have a repeat PET scan in 8-12 weeks, probably 8. We’ll see if the cancer seems to be holding steady or even shrinking. Again, holding steady would be enough to continue on the regimen I’m on.
It’s mindblowing that the rest of my life will be spent on some form of chemo. I’m coming to terms with that. It still scares the crap out of me.
But, I have a plan and I’m going to do what I can to be strong.
I’m tired and dizzy and worn out. But I do appreciate all of your messages and love. It matters.
I hope this gives everyone an overview. I’ll try to address questions at a later time.
xoxo
lisa
October 10th, 2012 §
Many friends and family are now following my Twitter feed. If you are, let me know. My username there is adamslisa. It’s nice to see more of you there. I do update a lot there in between big posts here. Daily life is there. I don’t always catch new followers.
My meeting with my local oncologist was about an hour. Some tests are back, (still waiting on a few and Sloan Kettering will run some other tests with their own pathologists) and they indicate that the cancer is “strongly estrogen receptor positive” (not a surprise). This means there are a variety of drug agents we can start with to try to keep this under control. The two-prong goal is to actually shrink the disease that’s there and also keep it from progressing for as long as possible. In most cases, older women are more likely to have slower growing disease and younger women to have more aggressive disease. We’ll have to see if the drug therapies (starting with anti hormonals) will work. Of course I’ve been on Tamoxifen or Armidex all along and also had my ovaries out, so I am already in an estrogen-deprived state. Not sure what that will mean for likelihood of working but the science of it is complex and I’m learning as I go. There are injectable agents and IV chemo to throw into the mix too. All will have side effects, of course.
We learned that the pain I have in my shoulder and chest is actually two fractured ribs from where bones are weakened by cancer. That will not heal until the disease is reduced. If the pain gets too much before we do that I will need 2-3 weeks of targeted radiation to kill those cancer cells and allow the bone to heal. I’ll start an infusion of Zometa to help strengthen my bones in the next week. That is an IV drug given monthly to help my bones.
The actual plan of what I will start with be decided Thursday, once I see what clinical trials are available. At this point most likely will be starting with the standard combo of Aromasin and Effexor. These are oral chemo, anti hormonals. They have side effects. Mostly bone pain, joint pain, mouth sores, dry mouth. I need to do reading on them soon. This is the first line of defense. I get to keep my hair during these. PET scans will be about every 2 months. Bloodwork in the form of tumor marker tests will be monitored monthly. I was one of the 2/3 of women who have elevated numbers at time of metastasis so at least there is something useful in looking at those. This is one reason some doctors don’t like these tests routinely: one third of the time there will be a metastasis without an elevation in these tests. They also can be elevated for a reason other than metastasis, so there are false positive results.
I have disease in the fractured areas, in T12 of my spine and in a spot on my upper femur near my hip. Today I will have a brain MRI to see if there is any in my brain. The PET does not have the ability to show that. Of course we hope with all of our hearts there is not.
How long has the cancer been there? Hard to say. I mean, the reason you do chemo is because you figure that once cells have left the breast you might be missing some. Any cells that are left can start growing at any time. That’s what the anti hormonals like Tamoxifen and Arimidex (an AI, or aromatase inhibitor) are designed to keep at bay to a greater extent than doing nothing. My doctor feels there are periods of exponential growth which eventually reach critical mass. This cancer has probably been there for about six months or less. In my spine and femur the cancer is confined to the soft part of the bone, the marrow.
I’m having trouble eating, pretty much confined to liquid and soft foods like yogurt. I’ve lost a lot of weight and know I need to get my strength up for the assault that is about to hit with treatment. I’m trying. Right now I am very weak, in body and spirit. But this will change. It must change. I’m adjusting and gaining knowledge and I had better get my head around this soon. But that is hard. I am angry and sad and scared and I go through every emotion multiple times a day. I cry at everything and nothing. I snuggle with my children as much as I can. I talk with Paige about what’s going on, she wants to know everything. We do not talk about prognosis and timing, only that it’s not curable and treatment won’t ever end. We talk about advances in treatment and how new things are coming along every day. We talk about the role Herceptin has played in giving life to those with the HER2Neu form of the disease. I do not have that form, but my mother did. The infusions she received of Herceptin (at that time not yet FDA approved but she got under ‘compassionate use’ exemption) saved her life we believe.
So, brain scan Wednesday afternoon, Sloan Kettering Thursday. Then we will have a plan and will start immediately. Until then, resting and trying to eat and control the pain in the fractured areas.
I won’t lie: every moment is a nightmare. There isn’t a second I am not thinking about cancer now. I hate that part, how it eats my life as it consumer my bones. I know this is normal for now but I hope someday soon I can think about other things. I don’t know if that’s a pipe dream.
My friend Andrea sent me the most magically colored flowers yesterday. The note said, simply, “Anything is possible.” I alternate between wanting, needing to believe that and thinking that might be giving myself false hope. But then I think of how much I believe in science, and drug advances, and I want to believe that’s true.
Thanks for all of the continued love and support. These posts take a lot of time and energy so they won’t always come immediately. I am using time to rest and do tasks around the house that need to be taken care of, doctors’ appointments, etc. Thank you notes have taken a back seat and for now an email of gratitude is all you might get from me. I wish I could do more, but please understand why this is the case. And as always, the disclaimer: I am presenting my interpretation of what I am being told by my doctors. It’s not medical advice. It is sometimes simplification of complicated medical scenarios. I’m doing my best to distill it down but I’m not a doctor.
Much love,
lisa
October 9th, 2012 §
I hate October now. I don’t even like the color pink anymore. I get cranky in the last days of September when I start seeing everything from toilet paper to staplers colored pink and sporting a pink ribbon. It’s not that I don’t want attention called to the disease that affects so many people including me; it’s more that I think the focus has gotten misplaced. I don’t support Susan G. Komen Foundation anymore; I think they have lost their way. There is good research going on in many places, but I have come to question the line between commerce and research with Komen’s support of everything from Kentucky Fried Chicken to alcoholic beverages to its own perfume while simultaneously trying to prevent anyone else from using the phrase “For the Cure” (see my post on why I divorced the Komen Foundation years ago here). What happened to thinking we are all in this together, trying to achieve the same goals?
When I originally wrote it I tried to think about awareness and what it means to me. I wanted to explain why pink ribbons didn’t mean awareness; I wanted to capture the emotional side of this disease. I re-post it every year. Now, with my new diagnosis of metastatic breast cancer, it’s time to share it again.
…………………………………………………..
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
October 8th, 2012 §
I just received a call from my oncologist: the pathology reports are not back yet so our meeting is postponed until tomorrow (Tuesday) morning.
October 7th, 2012 §
My Facebook page has bloomed into a virtual garden. Friends have posted photos of their favorite flowers in a digital display of love and support. I love this idea. Each person has posted a picture more lovely than the next and I can’t tell you how much I appreciate it.
Many readers have asked about how I found out my cancer had returned/metastasized. I will write that account soon: it’s important. However, I need some time to write that up completely. I’ve been spending the weekend with my two older children having long talks about what’s happening. Their love and concern is heartbreaking. These talks are among the hardest conversations a parent can have but are the most important. These days are setting the foundation for those to come.
Monday afternoon at 4:30 I will meet with my local hematologist/oncologist and find out the details of my pathology report and talk more about the diagnosis. Thursday I will meet with my breast oncologist at Sloan Kettering and discuss treatment options with her as well. I have used both of these physicians since my original diagnosis so I don’t have to start from scratch with my medical history over the past few years.
I expect immediately after these meetings I will begin my first phase of treatment– whatever that is. I won’t speculate at this point what it might be, there are a variety of forms it might take.
I’m healing from surgery, my neck is very sore, with a good sized incision at the base of my throat. I had a nice tracheotomy scar there already since the age of 5; unfortunately, this one is puffy and angry and red and makes me miss my old one a lot. I couldn’t talk yesterday, but today I’m back jabbering away. I alternate between strength and falling apart, but I don’t think that’s anything unusual. It’s still all mindboggling. A week ago I was readying for a trip to the same oncologist, with no clue what news awaited me.
My appointment is late in the day Monday, so the next update might not actually get written until Tuesday. I’ll be in touch.
October 5th, 2012 §
I loved the book The Age of Miracles by Karen Thompson Walker. I had the pleasure of meeting the author a few months ago. In the book, the earth’s rotation starts to slow. The days stretch longer with obvious consequences on daily life with some not-so-obvious effects on personal lives. I found the book immensely readable, creative, and thought-provoking (My teen daughter thoroughly enjoyed it too. It’s absolutely appropriate for that age group).
My own life has suddenly taken an opposite turn. It feels as if the world has sped up. The days are flying by. There just isn’t enough time.
It’s only been four days since we had an inkling from my oncologist that I had metastatic breast cancer, three days since I have known for sure. And now, in the middle of the night, it’s time I long for. The Earth is spinning so fast… how can it be I’ve been awake for two hours? Have I spent them wisely? What else could I be doing with those days, minutes, seconds?
I’ve done so much already.
I wanted to share a few ideas on things I’ve done already, many of them pertaining to my children. In the dizzying days after a metastatic cancer diagnosis there is so much emotion that it might be hard to think about what to do. You feel helpless. In some ways you are helpless until you get more information. But in the meantime here are some tips about what you can do.
I understand that not all of my readers have children. But for those of us who do, helping children adjust to this news is vital. It not only helps the children but can help relieve some associated stress for the parent.
- Don’t share your news until you know for sure what your particular diagnosis is. I don’t think you need to know your exact treatment; that takes time. But even knowing a general range of what might be used is helpful. If you have had cancer before, children will usually want to know if you will be doing the same thing (especially if it has to do with hair loss) or if it will be different.
- In my case I needed to have a mediastinoscopy with biopsy after my status was confirmed. It’s an outpatient surgery that inserts a camera through an incision in your neck to grab some lymph nodes for biopsy. I decided to focus on that concrete event mostly… it’s something children can wrap their heads around… Mom is going to the hospital (not uncommon in my household), having a small operation, will be back tomorrow night. I explained the cancer, the metastasis, and answered lots of questions, but I think the “one step at a time” was more easily tangible with the surgery as the immediate hurdle. If you will need an overnight stay for your particular surgery I think it’s best not to spring that news on children if possible. An overnight absence is best with a few days’ notice. Children, in my experience, are usually a bit clingy after bad news and that would provide the opportunity for follow-up questions and reassurance.
- Be sure you understand your diagnosis. Explain what words mean to children and to your friends. There are many misunderstandings about cancer and stage IV cancer. The word “terminal” might be scary. Stage IV cancer is not the same diagnosis in different diseases. Prognoses vary and some types of metastatic cancer can be slow-growing or respond well to treatment, allowing years of life.
- I think the phrase “it’s not curable but it is treatable” is important to teach and use.
- Wait to share your news publicly until after you have told your children (except with a few close friends you can trust to keep the information to themselves. This determination may not be as easy as it sounds). This also gives you a day or two to begin adjusting to the news so that when you do discuss it with your children you might have emotions a little more in check.
- As soon as you tell your children, be sure to tell adults who work with your children on a regular basis. If your children have learned the news, by the time they go to school, lessons, and sports, their teachers need to know. Email coaches, teachers, school administration, guidance counselors, school psychologists, and music teachers. Grief in children is complicated and it’s important that all of the adults know and can be on the lookout for odd behavior. Also, they need to be understanding if things don’t seem to be running as smoothly at home or a child seems tired or preoccupied. Two-way communication is key. Adults need to know they have the opportunity to bring any problems they see to your attention easily. Encourage them to do so, whether what they observe is positive or negative.
- Use counselors, especially school psychologists. My first call yesterday morning before I left for surgery was to reach the high school psychologist. Because Paige is in a new school (high school) I didn’t even know which person it would be. Even though it was only 9 in the morning when I called, the psychologist had already received my email (forwarded from the guidance department to the appropriate person) and had a plan in place to find my daughter during 2nd period study hall. She was able to introduce herself, talk to my daughter, and let her know how to get in touch with her as needed. They set up an appointment to meet to talk more in depth after their initial chat. Paige likes her, feels comfortable with her. This resource is invaluable. After my mother-in-law was killed in a car crash 3 years ago, the middle school guidance counselor became a refuge for Paige. When she was sad, distracted, needed a place to go have a good cry or talk, she had a safe place with an adult to help her. These individuals are part of my team. We are working together and it’s so important to use them.
- I have always felt that it’s important to be honest about a diagnosis; that is, open and public. I know this doesn’t work for everyone. The downsides of being public about a diagnosis are outweighed by the negative pressure for children if they have to keep a secret and bury feelings about such a serious topic. Children take their lead from you. If you are up front and comfortable discussing it, your children will learn to be that way, too.
- Call your other medical professionals and tell them of your diagnosis. Not only will they want to know because they care, but there may be instances where treatments may need to be examined or medications evaluated more often (for example, my endocrinologist wants to monitor my thyroid hormone levels more often than usual). They are all part of your team. They want to know. Many of the most touching and heartfelt phone calls I got were from my doctors this week. They cried with me, gave me information, offers of help, and caring. It also means if you have a situation when you need urgent medical care their office will already be aware of the situation and will likely respond more quickly to get you in to see the doctor.
- A carefully worded email is invaluable. Accurate information is documented so people don’t spread rumors. Friends can refer back to it if needed without asking you. They can forward it to other individuals easily, as can you. Choose your words carefully. The words you use will be repeated so make sure the email says what you want it to say to friends and relatives. The right explanation is much more helpful than a quick one sentence Facebook status update. People will have questions, and you can head many of them off by including that in your email (if you so desire).
I will be posting more tips about what I’m doing in the weeks and months ahead. Hopefully they will help you or someone you care about. There is so much you can’t control during this time, and that’s unnerving. Even taking steps like these can give you concrete tasks and a feeling of accomplishment that you are helping yourself and those you love.
October 3rd, 2012 §
Dear friends and family,
This is the last post I ever wanted to make but you all know that I am open and honest to a fault. Many of you noticed that I have not been online all week. Some of you checked in on me.
Some of you have heard the news by now: this week I received confirmation that my cancer has returned, now it has metastasized to my bones. It is not bone cancer. It is breast cancer that is in my bones. This means it’s stage IV breast cancer.
On Thursday I will have surgery to go in through my neck and retrieve some lymph nodes in my chest for testing. This will establish the hormone receptor status of the disease. My cancer was hormone receptor positive the first time around, we need to see if it still is or whether it’s converted. This is important in that it tells us what drugs to try first to contain the disease.
This is not curable. The goal is to keep it growing slowly and keep it at bay for as long as possible. At this point how long that is is pure speculation, we need to see how it responds to drugs I will take. These could range from oral anti- hormone treatments to daily injections to IV chemo again. There are many different types of things they can try to use on this. I have already had a double mastectomy, chemo, and my ovaries removed to try to keep this from happening. Unfortunately my efforts did not work.
I will be writing more in detail about how I found out the cancer was back (be your own health advocate!) and writing along the way about what’s happening and what treatment is like. I know not all of you are readers of my blog; that will be the best place to get updates for now. My goal has always been to de-mystify this disease and its treatment as much as possible and I will continue to do that to the end. For now I am focused not on the end result but on the potential for science to provide me with treatment that will give me years of happiness with my beautiful husband and children. I do not know how many those will be.
If you want to receive emails of the blogposts (no pressure!) you can go to lisabadams.com and enter your email address in the upper right. Be sure to look for the message in your inbox; you have to confirm that message to receive the updates. You can always just drop in to the website for an update if you don’t want to get them automatically. I will need to use the blog to do updates mostly because the updates will become time-consuming and I hope to do them in a public way to allow other people to read what this part of cancer is like. Those of you who follow me on Twitter, I will continue to be my prolific self as much as possible. My friends there are real friends in every way and have become some of my strongest in-real-life friends and were the first to pick up on the fact that something was wrong.
For now there isn’t anything we need. I’m hibernating and will need a few days to recover at home from the surgery tomorrow. You will see people around in the coming months who are helping me with the house and kids. My mom and dad will come at various times as well.
I ask that you not ask the children too many detailed questions right now. They will be getting used to this way of life again. They know my cancer is back. They know I will be treating it. We are leaving it at that for now to let them adjust to this while we gather the necessary information.
I know I have a great family and support system with all of my friends and I already am seeing the help and love they can give. I thank you for your concern, thoughts and wishes and you know I will be giving this everything I’ve got.
Please understand if I cannot respond to every message in a timely fashion. Your words mean so much to me but there are only so many hours in the day right now during this hectic time. I do read every single one though, and am buoyed by each.
Much love,
Lisa
July 20th, 2012 §
There is a natural tendency to turn our heads from things which are upsetting.
But as adults it is our responsibility to be aware of them.
Protecting is not always the right thing.
Jennifer Merendino was first diagnosed with breast cancer in 2008, shortly after her wedding. Her husband Angelo began taking photographs (www.mywifesfightwithbreastcancer.com). Angelo documented her surgeries and treatment all the way through her death in December of 2011 after she experienced metastases to her liver and brain.
The Gathering Place: A Caring Community for Those Touched by Cancer in Westlake, Ohio, said they wanted to exhibit some of Angelo’s photographs in their art gallery.
After a successful opening, The Gathering Place pulled the exhibit. In their own words:
Shortly after the exhibit was hung some of our volunteers (many of whom are cancer survivors) and our participants found it very difficult and emotionally upsetting to see the exhibition. Because our mission at The Gathering Place is to provide a peaceful, healing and nurturing environment where our participants feel supported and encouraged, we have chosen to remove the exhibit so as to not add to the emotional challenges a cancer journey creates.
It’s not that I can’t understand how someone might find the images disturbing. In fact, I think you are pretty hard-hearted if you don’t. But that is the point. It isn’t enough to say you want to be “a community for those touched by cancer.” It’s important to get the message out: breast cancer isn’t pretty. It isn’t a pink ribbon or a one-day walk to raise money. It isn’t about wearing a pink football cleats in October.
I do not agree with The Gathering Place’s decision to remove the photographs from their art gallery once they had seen the photos, chosen to display them in their gallery, and had a public opening. Despite their stated goals, in this instance they don’t “get it.” The proof of that to me is the web address name The Gathering Place used to announce the removal of the photos from the gallery. The web address for that post is http://www.touchedbycancer.org/2012/07/art-imitating-life/
Art imitating life? No way. Angelo’s art is no imitation. It’s the real deal. It captures the reality of his wife’s cancer treatment for all to see. And sometimes, even when it’s painful, we must look.
July 13th, 2012 §
When I die don’t think you’ve “lost” me.
I’ll be right there with you, living on in the memories we have made.
When I die don’t say I “fought a battle.” Or “lost a battle.” Or “succumbed.”
Don’t make it sound like I didn’t try hard enough, or have the right attitude, or that I simply gave up.
When I die don’t say I “passed.”
That sounds like I walked by you in the corridor at school.
When I die tell the world what happened.
Plain and simple.
No euphemisms, no flowery language, no metaphors.
Instead, remember me and let my words live on.
Tell stories of something good I did.
Give my children a kind word. Let them know what they meant to me. That I would have stayed forever if I could.
Don’t try to comfort my children by telling them I’m an angel watching over them from heaven or that I’m in a better place:
There is no better place to me than being here with them.
They have learned about grief and they will learn more.
That is part of it all.
When I die someday just tell the truth:
I lived, I died.
The end.
June 28th, 2012 §
I finished a new novel recently, one I enjoyed enough to share with all of you. It’s called The Good Father by Noah Hawley, and it’s an exploration of what might happen to a parent when his child is accused of doing something terrible. In this case, Dr. Paul Allen’s son is accused of shooting and killing a candidate for President (I’m not giving anything away by revealing that plotline). Paul eventually starts traveling around, talking to people who knew his son during the months leading up to the shooting. One man he talks to is named Carlos.
Carlos tells Paul a story about his brother who stepped on a land mine. His legs were saved but his intestines were crippled. He needed a colostomy, and doctors repeatedly told him it was temporary. They keep telling him that he will use the toilet in the normal fashion again. But their promises don’t come true. He continues to need the colostomy. After two years of false hope his brother couldn’t take it anymore, and he kills himself. Carlos says:
Acceptance is the key to happiness. If those doctors had told my brother he’d be crapping in a bag for the rest of his life, he would have accepted it. He could have found a way to be happy. But instead they gave him hope. They promised him a better life. And so he spent every day hating the life he had.
Though fictional dialogue, this scene really struck home. It immediately reminded me of Admiral Jim Stockdale and The Stockdale Paradox. Jim Stockdale was the highest-ranking naval officer held as a Prisoner of War during Vietnam. Captive for more than seven years, tortured more than 20 times, Stockdale is an expert in how to deal with hope. Stockdale talked about his experience to James C. Collins, eventually published in the book Good to Great:
I never doubted not only that I would get out, but also that I would prevail in the end and turn the experience into the defining event of my life, which, in retrospect, I would not trade.
Stockdale’s next observation floored me the first time I heard it. He was asked to talk about those who did not make it home, who died in Vietnam after being taken into custody:
They were the ones who said, ‘We’re going to be out by Christmas.’ And Christmas would come, and Christmas would go. Then they’d say, ‘We’re going to be out by Easter.’ And Easter would come, and Easter would go. And then Thanksgiving, and then it would be Christmas again. And they died of a broken heart.
This is a very important lesson. You must never confuse faith that you will prevail in the end—which you can never afford to lose—with the discipline to confront the most brutal facts of your current reality, whatever they might be.
Stockdale is telling us to forget the eternally positive attitude, the belief that hope is enough. He says, rather, that you must always believe you will succeed, but not place an expiration date on it. In fact, doing so (“I’ll be better by Christmas”) can, in his opinion, be a recipe for disaster and self-destruction. Stockdale had a failed political career, but that doesn’t matter to me. He made it through his confinement, and what he thinks about the reasons for it interest me.
I’ve never been a believer in the “a positive attitude is everything.” That doesn’t mean I don’t think you generally should have one. Like Stockdale, I believe you must fight as if you will win. But, and this is key to me, you must accept that you do not know the outcome. This is where I differ with Stockdale’s prescription. I believe you cannot confuse having hope with the reality that your hope may not be, and often will not be, enough.
A few weeks ago as my three children had their dental checkups, I picked up People magazine. I skimmed the letters to the editor. One letter, from a woman named Barbara, referred to a prior People story about Ryan O’Neal having cancer. “I know that he will overcome this because he has immense strength and courage,” she wrote. Barbara is not unique. I have heard this exact statement countless times.
First, I’m fascinated by Barbara’s knowledge over O’Neal’s outcome. To claim she knows what’s going to happen to him is pretty remarkable. She has no knowledge about anything except a few quotes in a pop culture magazine and yet she “knows” he will overcome it. Second, and this is the big one: strength and courage are not enough, I’m sorry to say. Don’t those who die from cancer have strength and courage? Is it their fault that they aren’t surviving? Strength and courage are needed, for sure. But just having them won’t do it. You can’t think the cancer away.
June 18th, 2012 §
The last month has been busy with good things.
Somehow I’ve wanted to tuck these things away, commit them to memory, etch them in my mind so that I might remember. I’ve been taking loads of pictures and rather than writing, photography has been my way of documenting these times. I find myself taking photographs more and more each week, and getting a lot of joy from doing so. I post many of them on Instagram for those of you who might be interested (username: adamslisa).
Paige graduated from eighth grade this week. The fact that my firstborn is starting high school in the fall is mindblowing.


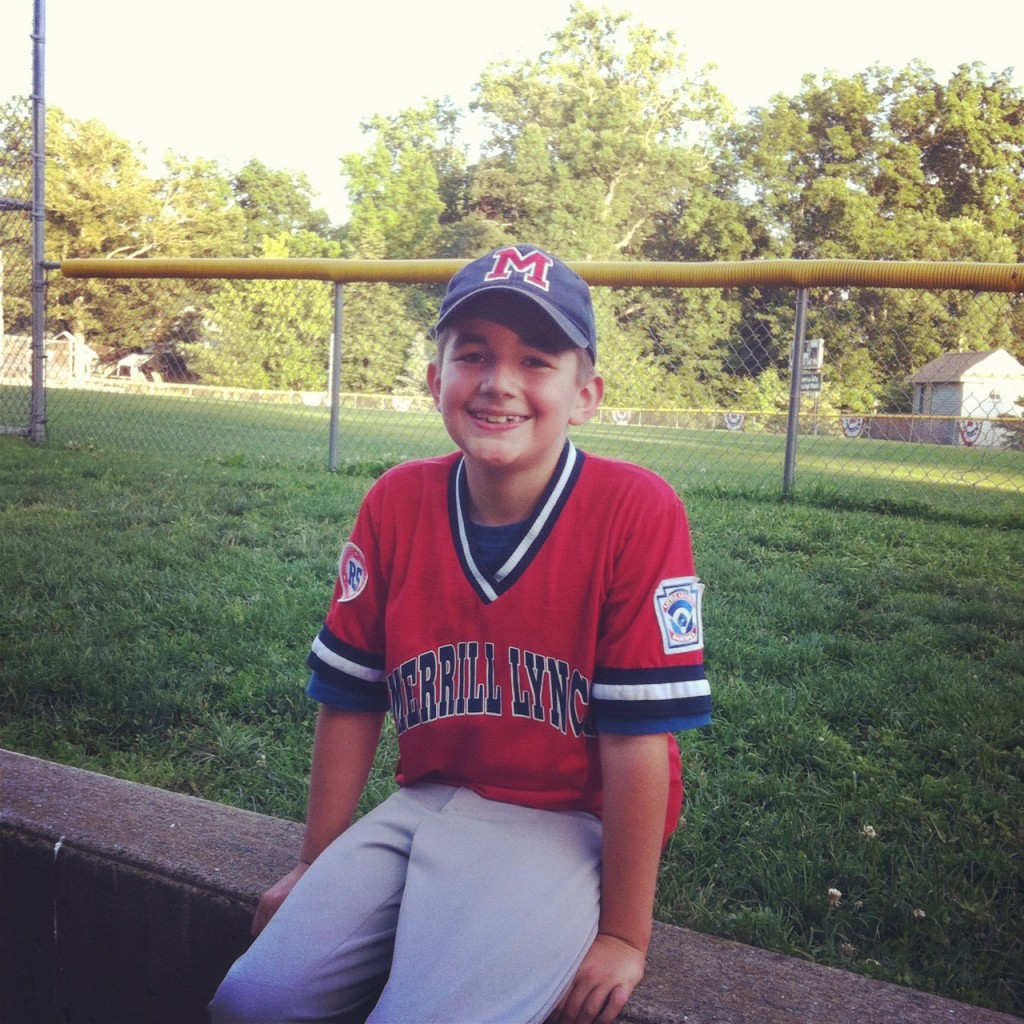
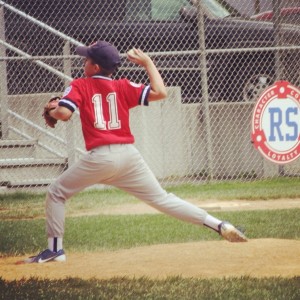
Colin finished 4th grade, made the All-Star baseball team (they lost the game) and then had his Little League Minors team win the Championship today (a happier boy could not be found). He pitched the first 3 innings of the game today and I’ve enjoyed this season immensely. What a great group of boys and coaches on the team this year. I love that he still waves to me when he is playing right field and still will yell, “Hi Mom!” as he runs by. I love that he still hugs me at the bus stop and tells me he loves me many times each and every day, without hesitation.
These things matter. They may change. They probably will. But for now, I treasure them.

Tristan and Paige had a piano recital yesterday and Tristan got his first trophy. On Tuesday we will take him to Philadelphia to see his orthopedic team at Shriners Hospital for a checkup. He is bubbling with excitement at being a first grader now…

June 18 is a significant date. It was 5 years ago today that I had my last chemo treatment.
Five years isn’t meaningful in terms of my disease. It doesn’t mean I’m “cured.” My kind of breast cancer can return after seven years, or twelve, or fifteen. But it’s still five years so far that I have had no evidence of a recurrence. Five years of memories. Five years that matter.
These last few weeks have been magical to me.
These were the days I fought for.
These were the days I wanted.
These are the days I longed to share with my husband and my children. And I am doing just that.
I’ve been overwhelmed with emotions in these weeks, seeing my children change and being so proud of not only what they do, but also who they are.
I think when it comes down to it I haven’t been writing this month because I needed to hold all of this inside. I needed to let it sink in. I needed to steep in the glory that these simple days hold.
Being alive to share these days with my friends and family.
Helping others who are undergoing treatment and surgery.
My days are full and I do not take them for granted.

May 4th, 2012 §
Regrets are most often over things we have not done, rather than things we have.
Inaction, it seems, is harder to tolerate than action.
Doing something, even if it’s ultimately a mistake, is better than doing nothing.
I’m constantly torn between taking chances and staying nestled in the warm comfort of habit. I am a lover of routine, constancy, predictability. One of the many reasons I fell in love with my husband is his admirable and enduring sense of calm. I am more hot-headed, far quicker to be annoyed, get frustrated, to yell. I strive to be more like him in his ability to go with the flow, but most often I fail miserably.
I’m not a risk-taker. I tend to over-think things. If there is something unpleasant that needs to be done, I do it immediately so I can move on. If I were still a child I would eat the green vegetables first so I could enjoy the rest of the meal.
Making drastic changes often doesn’t work. I’ve been trying to branch out in a few ways over the past few months and I’m happier for it. I’ve started doing Pilates weekly, sometimes twice a week, and I’m loving it. I am physically stronger, have a teacher I adore, and many weeks get to take the lesson as a duet (semi-private) with a dear friend.
I’ve been taking lots of photos and enjoying not only the images I’m capturing, but also the social element of sharing them on Instagram. I enjoy seeing the slivers of beauty that are around us every day and am taking time to appreciate them more.
I’m taking more chances with my writing. I’ve been privately writing about a wider variety of topics, and trying out longer-form work. I recently read a story I wrote out loud to a group for the first time.
I curse middle age a few times a day, mostly about my body and how things just don’t work like they used to. But the perspective I have through my life experiences, the wisdom that I have after 42 years of ups and downs, the confidence to say, “I am flawed, I will try to be better, but I also know who I am” are all valuable.
I enjoy having others in my life but also know that when it comes time to take a chance, I can wrap my arms around myself and jump.
April 20th, 2012 §
The other night, in 140 character tweets, I made some comments about my past few days on vacation in Jamaica. I noticed that two tweets especially received lots of replies and lots of “favorited” status.
Two simple sentences that captured so much of what I’ve been thinking about this week.
The tweets read:
Folks, these were the days I fought for during chemo. This time is my reward. These days with my family are priceless.
It doesn’t mean I don’t complain, or have bad days, or get frustrated with my kids. Life isn’t perfect. But I try to appreciate all I can.

breakfast

the simple geometry of a beach umbrella

open door policy

pool steps
I took many photos this week which you can see now on Instagram (my username there is AdamsLisa). I’ll be posting my favorites here occasionally in the weeks ahead, and probably next winter when we all are craving some views of sunshine and palm trees.
I am grateful to Clarke for working hard each day to pay for the trip, to my children for being the individuals they are who make me smile, laugh, and go to the computer to Google answers to endless questions. I always appreciate their hugs and kisses and sense of wonder and enthusiasm for life. I know these days with them are fleeting.
Life is fragile. I know it.
I am treasuring these last hours here in Paradise.
April 19th, 2012 §
This blogpost came up in conversation recently so I’ve decided to re-post it. While there may be exceptions, in general I firmly believe it’s important to be open and honest with children about serious illness (in my case it was cancer). Not only is it important to explain it to them to de-mystify illness, it can also be crucial that children be aware of the condition in case of emergency. For example, if a child is alone with a parent who has a medical condition and the parent loses consciousness or injures herself, the child can call 911 and provide important information about what might be the cause for the problem. Similarly, people with metastatic cancer may have daily medical issues that are ongoing. Chemotherapy that is chronic, repeat surgeries, severe side effects, and more frequent tests and appointments may mean hiding a diagnosis is probably not even an option. Metastatic cancer patients may view withholding information as a luxury they do not have.
Using the real words to name our diseases/conditions can also be important for children’s knowledge of their family medical history. I have heard stories of women diagnosed with breast cancer who only learned of a family history of the disease after their own cancer was diagnosed. Only then did information come to light that relatives had also had the disease. Perhaps knowledge of a familial history of the disease would have been useful at an earlier time and monitoring could have begun sooner.
…………………………….
I met a woman who told me something shocking.
It wasn’t that she’d had breast cancer.
Or had a double mastectomy with the TRAM flap procedure for reconstruction.
Or that she’d had chemotherapy.
What made my jaw literally drop open was her statement that she has never told the younger two of her four children that she’s had cancer.
Ever.
Not when she was diagnosed.
Or recovering from any of her surgeries.
Or undergoing chemotherapy.
She never told them.
To this day– five years later– they do not know.
I like to think I’m pretty open-minded. But I confess, it took a lot of self-control not to blurt out, “I think that is a big mistake.”
I’m a big believer in being open and honest with your children about having cancer. My caveat, using common sense, is that you should only give them age-appropriate information.
When I was diagnosed with breast cancer Tristan was six months old. Of course he didn’t understand what cancer was. Colin, age 5 at the time, understood some of what was happening. I explained to him what cancer meant, that I was going to need surgery to take the cancer out, where the cancer was, what chemo was, what it would do to my appearance and energy level. Using words like “I will be more tired than I usually am. I might feel sick to my stomach and need to rest more” explained things in words he could understand.
Age 8 and the oldest at the time, Paige understood the most when I was diagnosed. She had bigger questions and well as concerns about me (“Will I get it too? Who is going to take care of us? Are you going to be okay?”).
It’s not that I think small children always understand everything. But they are certainly able to sense that things are not “normal.” They can tell when people are acting strange. I think it’s important that they know there is a reason for that change. Children have a tendency to be egocentric; they think that everything is their fault. They may think they have done something wrong if everything at home feels different.
The woman told me she didn’t want to worry her children. She thought it “unnecessary” to tell them. She said when they got older she would explain it. I argue that by keeping her cancer a secret, she runs the risk of doing the opposite: making cancer seem scarier and more worrisome. If children hear words like “cancer” casually in conversation as they grow up they will be comfortable with them; in that way, they won’t be frightened of them. If they understand the truth of the diagnosis and treatment they are dealing with reality. By hiding the truth, the unintended consequence is to make it seem worse than it is. By not telling children, and waiting until they are older, it reinforces the idea that cancer IS something “big and scary.” After all, if it weren’t, you would have told them already.
I think being secretive is a step backward to the days when cancer was only talked about in hushed tones: the “C” word or “a long illness.” These concepts might seem primitive to us now, but it wasn’t long ago that these vague labels were the norm. By showing our children, our friends, our neighbors, that we can live with cancer, live after cancer, we put cancer in its rightful place.
To me, the deception that goes on to lie to children about where you are going, what you are doing is lying about a fundamental part of your life. Cancer isn’t all I am — but it is a part. And it’s an important part of my medical history. If for the past 3 years I’d covered up where I was going and what I was doing, the web of deceit would have been extensive. I can’t (and won’t) live a life like that.
Further, I think it’s a poor example to set for my children.
Lying,
covering up information,
and omitting important information are all wrong.
With rare exception, the truth is always best.
Presented in the proper way,
commensurate with a child’s age,
a difficult situation can be not only tolerable but surmountable.
It takes work. It takes parents who can manage not only their own emotions about having cancer but also be involved with helping their children cope with it. It’s more work, but it’s worth it.
I think that woman made a mistake. I think her decision was harmful. I am sure she thinks she was doing her children a favor. I totally disagree. I think keeping this type of information from children “in their own best interest” is rarely– if ever– the right thing to do.
April 13th, 2012 §
In the past few weeks a flurry of news articles discussed the topic of overtreatment in medicine. From both sides, suddenly, we are hearing physicians (“Doctor Panels Recommend Fewer Tests for Patients”) and patients (“Do Patients Want More Care or Less?”) proposing what seem as a controversial idea: less care may be, and often is, better.
My thoughts on this topic stem from a variety of influences: my father spent his career as a cardiothoracic surgeon and now is editor of the Journal of Lancaster General Hospital. My mother spent her career as a psychologist. I have a graduate degree in sociology. Five years ago I was diagnosed with stage II breast cancer. I have a son with congenital defects in his spine and hands.
I list some of these influences because they are important sociological variables and have surely affected the way that I think about this subject. It is often the case that anecdotal evidence supplants cumulative scientific data when people make decisions; that is, if you or someone you know has had a certain experience, that information will weigh more heavily into your thought process than knowing what “the statistics show.”
When I underwent a double mastectomy and completed chemotherapy for my breast cancer, my two oncologists and I sat down in separate meetings to discuss the always stressful: “What now?” I had hormone-receptor positive cancer (breast cancer that is “fueled” by estrogen and/or progesterone) so I was able to take adjuvant therapy. I opted to have my ovaries removed even though I am BRCA-1 and 2 negative.
But what about screenings? After my double mastectomy they told me I wouldn’t get mammograms anymore. I would, however, do “tumor marker tests” that measure levels of antibodies in the blood. They are not very reliable, and therefore are not good screening devices. This is why they are not yet used for the general public and some oncologists don’t even use them. The tumor marker tests can sometimes show if cancer has returned before other symptoms show. Because the tumor marker tests are done via routine bloodwork, the tradeoff seems acceptable to us. The tests are relatively benign. When it comes to other testing, however, the bigger discussion started with my oncologists.
What about PET scans? Chest x-rays?
Discussions about screenings and testing are negotiations of sorts. As the new research and guidelines indicate, doctors and patients are often at odds on how much monitoring is “just right.” I propose that one of the most important variables in this discussion has been overlooked: the psychological ability of the patient to tolerate ambiguity. That is, I believe there are some people who can live with uncertainty better than others, and the amount of uncertainty a patient can accept in his/her treatment should be an important consideration in current discussions about overtreatment of patients.
The decision to have a prophylactic mastectomy on my right side, for example, was in part made because I didn’t want to worry about getting a new primary breast cancer on my other side. Some consider this decision controversial and I’ve spoken about my thought process here in USA Today with a followup to critics here.
Screenings are not always benign. While blood tests may be considered simple, they still cost money. Mammograms, x-rays, CT scans, and PET scans all expose the patient to radiation in varying amounts. Many patients are not aware of the relative radiation exposure that screening/diagnostic tests pose. For example, a chest CT provides nearly 200 times the amount of radiation as a two-view x-ray of the chest. A helical abdominal/pelvic CT provides the same amount of radiation as twenty 4-view mammograms (full article here).
My oncologists were quite clear five years ago: there would be no PET scans for me. I worried: after all, shouldn’t I be monitoring my body for any residual cancer? In my particular case, they were adamant: no (of course there are many cases where this risk-to-benefit ratio is different and PET scans are necessary. There are many factors used to make this decision). These decisions are not solely about radiation exposure; they also take into account how likely tests are to yield false positive results on a PET scan. There are many reasons why areas may “light up” in a scan, arousing suspicion. If any areas do light up, this could provide more anxiety and opportunity for additional testing, most often unnecessarily. Not every suspicious area can be biopsied, and you can’t biopsy every time something lights up. Instead, watchful waiting with a keen eye to symptoms of potential recurrence is what we’ve determined is best. I do get a chest x-ray each year. I do tumor marker tests. I follow up with my physicans if there is pain that doesn’t resolve (which can sometimes be a symptom of a cancer recurrence).
I’ve taken a different approach in the past few years with tests not only for myself but also for my children. I always ask “Is this really necessary? Is it important? Does it need to be done this often?” This is not to say that the test won’t happen. I’m not arguing with the providers. But discussing these topics is important. Frequently, tests or screenings are suggested with a time range and now, with with some tests, if screenings have been clear in the past, longer intervals may be used in the future (Pap smears, dental x-rays, etc.). It is worth reading about some of these options and talking to your doctor/dentist about them.
Research shows that antibiotics are not needed (and no more effective than placebo) for many common illnesses like bronchitis, sinus infections, and ear infections. Yet, patients often clamor for them.
As I talked about in the USA Today interview/response piece, there are many factors which come into play when deciding what surgery one wants to have and what level of follow-up care is right for patients. This determination is one that a doctor and patient must come to together. Each must rely on the other to help navigate the murky waters of staying healthy. That said, our healthcare system does not often allow for such conversations to occur and does not reward doctors for the time needed to have in-depth conversations with their patients. Further, physicians are still concerned with liability if they opt to reduce testing on a patient and they miss a problem.
One variable that I think will help doctors and patients come to a more mutually satisfying relationship is a determination of the patient’s tolerance for uncertainty. With this information, physicians can identify more pointedly which levels of acute treatment and long-term follow up care are both psychologically acceptable to the patient and medically reasonable.
April 2nd, 2012 §
We gather friends like seashells throughout our lives, tucking the treasures away to take with us as we walk. At different times, we appreciate different qualities of those friends; characteristics that initially attract us to someone may later be a source of discomfort. Some friendships last entire lifetimes, others are brief but intense. Friendship is an art form, one we must learn and practice daily.
I recently read Lindsey Mead’s post about friendships made during life transitions. She writes, in part: “It strikes me that it is not an accident that our truest and most lasting friendships are forged during times of life transition; we are closest to those who have shared experiences that changed who we are. Whether it was childhood, college, or becoming mothers, this is true for me.”
I’ve thought about this for weeks because while I absolutely understand what she is talking about (and do have some friends like this), I’ve also seen many of those friendships fall by the wayside. I have written before about the ways cancer and friendship sometimes don’t mix. There are friends who just can’t deal with a friend’s illness and/or death of a family member and they just disappear. In contrast, there are friends who seem to thrive on helping when there is a crisis underway.
When I was diagnosed with breast cancer at 37 I did not have any friends who had already had the disease. One of my closest friends has a son who had experienced leukemia twice and received a bone marrow transplant from his sister that saved his life. I talked with her a lot, not only because she had some sense of the fears I had but also just because she is my friend and a great listener. While I treasured that connection, though, I didn’t know anyone who had recently had a double mastectomy, chemotherapy, or needed to figure out how to balance those treatments with caring for three young children. My diagnosis preceded my involvement with Facebook and Twitter; social media would have greatly changed my experience with cancer.
I didn’t like support groups; they just weren’t right for me. Instead, I found myself talking to and finding support from a few women who used some of the same surgeons I did. We’d see each other in the waiting room at the plastic surgeon’s office when we went for weekly “fills” to add saline to the tissue expanders in our chest that were stretching the skin and making space for the implants some of us chose to receive. During chemo, nurses would often try to put younger patients in the same semi-private chemo room so they could meet and pass along wisdom and support.
Not every interaction I had led me to a friendship, of course. Sometimes in stressful situations we just need someone to help get us through. Like the stranger in the seat next to you during a turbulent airplane ride who chats with you and passes the nervous minutes, we rely on strangers to steady us when we wobble. We look for cues that everything is okay, that our experience is in the range of what might be expected.
But as my chemo and surgeries and constant doctor appointments waned, there was more room for “the rest of our lives” in the conversations I was having. One woman and I became quite close; we’d meet for coffee and spend hours talking about cancer, its effect on us, our children, our spouses. We were different kinds of people, though, in dealing with our similar cancer diagnoses. As time went on, it became more and more apparent. For example, she didn’t want to share as much information with her children about her cancer as I did. She turned to controlling food as a way to deal with her fears of a recurrence; she felt she would be immune from a recurrence if only she only ate certain foods. She wanted to train to be a Rekei healer. Eventually, though, it was our disparate attitudes about cancer that drove a wedge between us. She felt it was important to always put a sunny face on cancer; she felt it was necessary to find the joy in it. She had a “head painting party” when she went bald from chemo. She had her daughters paint her head with designs and words. She collected positive sayings into a little book that extolled the virtues of positive thinking as a key to remission success.
I could be her friend and listen but I could not agree with what she believed. The thought of someone placing their hands over my skin but not touching it and transferring energy to me (Reiki) did not work for me. I didn’t believe that food was key to avoiding cancer (after all, I had friends who had been vegetarians before they got cancer; if food were the simple key to avoiding cancer we’d have figured that one out by now, I thought). I felt control of food was a grief reaction, a way to manage fear in an uncertain world. That difference alone would not have come between us, though. I think it was the “positive thinking is the key” that I think was the biggest stumbling block. We just fundamentally differed about how to approach this disease that dominated that period in our lives.
I was strong, determined, motivated. I researched the available options and discussed them with my medical team. I pushed back when they suggested certain treatment options. I was a participant in my treatment plan. But I also felt that this thing called cancer SUCKS. And it was okay to say that. It was okay to have a bad day, or hate shaving my head. I didn’t have to have a head painting party and rejoice in the experience of going bald from chemo. It was okay for me to get halfway through shaving my own head in my garage on the morning of my second chemo and tearfully ask my father to help me finish because I couldn’t get it all. It was okay to cry, to scream, to pout for a bit. Then I picked myself up and moved on. That’s what worked for me.
Every time I got a piece of bad news or felt overwhelmed after a doctor’s appointment I allowed myself 24 hours to recover. That day I could complain, feel the injustice of it all, just react. But the next morning: it was time to get on with it. Those negative feelings were important to me. They were real. They were how I felt. And having someone constantly saying that I should only think positive rubbed me the wrong way. It was, to me, “pinkwashing”: making breast cancer seem less awful than it often is. If the only things I expressed were how “cancer is a gift” and I “had to find the beauty in it” (as she did) that denied a very real truth to me: cancer had fundamentally changed my life and those around me, and those changes weren’t always positive.
It didn’t mean there weren’t experiences or people or lessons that I appreciated. It didn’t mean I didn’t want to emerge a wiser person for having gone through it. But “cancer is a gift”? No way. I saw blogs and books where survivors wrote, “Cancer is the best thing to happen to me.” I will never say those words. I think of all of the people in the world who live with cancer every day, whose lives will be cut short by it, who have lost people they love to the disease. In my mind it diminishes their deaths and diminished quality of life to say their disease is a gift. I will not say that cancer was the best thing to happen to me.
My friend and I just sort of fell out of touch, though we have talked a few times in the last few years. We have only warm feelings for each other and wish each other good health and happiness. But we aren’t close. And what that tells me is that cancer is a part of life. You can’t make a relationship work just because you have the same disease. We have different kinds of friends for different reasons. Some we love them because they are “just like us” and share common interests or senses of humor. Some we love them precisely because they are different– they push us in ways we are not accustomed to or expose us to interests or information we otherwise might miss. In this day and age we have Twitter friends, best friends, school friends, Facebook friends, etc. We interact with a variety of people in very different ways.
I also realize that we have different levels of patience for conflicts at different times in our lives. Maybe the differences I had with my friend about cancer wouldn’t bother me so much now. Maybe we were both raw and stressed about managing our illnesses and our families. We supported each other through the hardest times and once that period was over we just moved on in different ways. Maybe that wasn’t even what really caused our relationship to cool off in the first place; after all, we didn’t part ways on bad terms, the friendship just “fizzled.” It happens.
I realize I’m more likely to make friends in the daily grind of life, and my life is full of more people I consider friends than ever before. I have a rich network of people I like, trust, and enjoy spending time with. We are not always similar, and we don’t even have to share the same beliefs all of the time. Respect and kindness are hallmarks of friendship, and every relationship for that matter. I really enjoyed thinking about the friendships I’ve made, how I’ve made them, and which ones haven’t worked. The topic of cancer and friendship is one I will continue to write about. I treasure the friends I have. I am fortunate.
Thank you to Lindsey for planting the seed for me about this topic; she and her blog frequently push me to think, learn, and grow. I’m still ruminating on this subject… and I like that.
February 3rd, 2012 §
I’ve been public about my criticisms of the Susan G. Komen Foundation for a few years. That criticism has not been easy; after all, I’m criticizing a huge organization which claims to be committed to finding a “cure” for the disease I have. Even my choice of words there is related to my criticism of Komen; I think they need to focus less on a “cure” and more on acknowledging and helping women deal with cancer after their initial treatment and/or those women like me who have metastatic breast cancer. Survivors, and there are more and more of them, have long term physical needs, psychological concerns, and medical issues that are unique.
I started out like many breast cancer women do, looking to give something back when I finished my surgeries and chemotherapy. I was energized, and wanted to help. Of course, the Race for the Cure in Central Park is one way to do that.
In 2008 I joined a family friend and her fellow Yale students for the Susan G. Komen Race for the Cure.

I believed I was a part of something big, meaningful, important.
The following year I asked my parents if they would join me at the Race for the Cure to mark my 40th birthday. At my birthday party I eschewed personal gifts and asked instead that guests donate to our family team. We raised almost $15,000 that year between the party and other donations. My mother (a stage III cancer survivor) and I walked in our pink t-shirts with my father and my daughter Paige.

I wrote a piece in 2009 (titled “A Walk in the Park) about the experience. I’m including the text here because I think it shows my commitment to the cause, to that day… at least what I thought that day meant.
“More than just a walk in the Park.”
That’s the catchphrase that the t-shirts sponsored by Duane Reade had on them at the Susan G. Komen Race for the Cure yesterday. Clever. You spend a lot of time reading people’s backs while you walk the 5k.
Some people just have their registration numbers.
Some have bright pink signs that read “In Celebration of” or “In Memory of.”
Sometimes it’s one name.
Or two.
Or a list.
I didn’t wear a pink sign.
My list was too long.
You guys know who you are.
It would have been a long list.
And then it would have said:
Mom.
Me.
Sometimes there is a photograph or drawing on walkers’ pink placards.
Or a drawing of some hearts.
Sometimes the writing is neat, businesslike, easy to read. Sometimes it’s in a child’s handwriting.
Sometimes it’s hard to read, in magic marker or crayon.
Sometimes there are stickers.
Sometimes it’s a full name,
Sometimes it’s more familiar,
“Aunt Cathy” or “Grandma Rainey.”
It might be “Mom,”
or “Nana”
or “Bubbe.”
“My sister.”
There was a man walking in front of me for almost a mile whose bright pink sign said “In Celebration of ME.” Male breast cancer is not common, but it’s real, and it can be very aggressive. How hard it must be to be a man with breast cancer, I pondered. It’s almost always talked about as a woman’s disease.
There was a t-shirt that said “Pink is the new purple” on the back. We followed it for a few minutes, unable to figure out its meaning. We kept hypothesizing what it meant. Finally my mother ran ahead a few steps and asked the young woman in her 20s what it meant. My mom returned with the explanation:
Her sister had breast cancer.
Her sister’s favorite color was purple.
Her sister had died of breast cancer.
She was walking in her sister’s honor;
Therefore, pink was the new purple.
There was the man we caught up to and quickly passed who did the whole route limping heavily, walking with a cane. “Wow,” Paige said, “that must be really hard.”
“Yes,” I said, “That’s what this day is all about.
It’s not about going the farthest distance.
It’s not a marathon.
It’s not about pushing your body to do the most it can do.
They make this race a distance that lots of people can do.
Even cancer patients who are in the middle of their treatment.
They want to include everyone:
Moms with strollers,
people in chemo,
that man with his cane.
It’s about raising money,
not about making the walk too hard that people can’t do it.
It’s about bringing people together.”
There were families. They forced me to struggle to keep composure. Dads with children. Usually they had matching t-shirts with pictures of a woman on them. They all said a woman’s name and then “Mommy, we miss you.” These were families grieving women who were taken from them. Families who had lost their queen to breast cancer.
Twenty-five thousand people were there yesterday.
We were only four of them.
Everybody had a story.
My mother and I were only two of those breast cancer stories.
We were united yesterday with a purpose: To keep our daughters, nieces, and friends from having to go through what we did.
The distance wasn’t far to walk.
The distance we have to go to find a cure is.
I don’t personally know that I believe a cure is possible.
I don’t think in those terms.
I do believe that the advances we have made/are making in improving treatment are real. They help in terms of lower recurrence rates (fewer women get cancer again after having it once), higher survival outcomes (fewer women die from their cancer), and better quality of life. Even if we can’t find a cure, I believe that the more money we can get into the hands of scientists and foundations to help get women the care they need for their bodies and their minds can only be good.
I wore pink and walked side-by-side my mother yesterday.
I felt lucky to have her with me.
I felt lucky that she was alive to be next to me after being diagnosed with stage III breast cancer.
I couldn’t treasure her more than I already do.
But this disease is one thing I don’t want Paige to have in common with us.
It was a great day yesterday.
Paige and I woke up tired this morning, but happy.
Last night when we pulled into the garage I gently shook her awake.
I told her how proud I was of her.
I told her how happy Nana and I were that she had been with us.
How great it was that we had made a memory like that together.
How proud she should be that she and I had raised about $7000 for Komen for the Cure.
It really was more than just a walk in the Park.
So much more.
…………………………………………………..
In fact, the last time I spoke to my mother-in-law before she was killed in a car crash was a phone call she made to tell us how proud she was of us for raising so much money for Komen.
But after that event my feelings started to change. My health was still affected daily by the aftermath of my cancer. I started to be bothered by staplers with pink ribbons on them and football players decked out in pink sweatbands. I started to dread October’s ubiquitous pink ribbons in the name of Breast Cancer Awareness Month. Facebook status updates with women writing in silly code about where they leave their handbag as a veiled hat tip to breast cancer “awareness” started to bother me more and more. Soon friends and I started a contest; we would snap photos of the craziest products we could find with a pink ribbon on it. When Komen partnered with Kentucky Fried Chicken and Mike’s Hard Lemonade, people started wondering about some of the choices Komen was making; after all, fatty processed foods and frequent alcohol use are risk factors for breast cancer. I wondered, too.
As I’m feeling worse about all of this “pinkwashing,” I learned that Komen was getting litigious against everyone from kids to business owners trying to raise money for cancer charities. Why? Because Komen said that only they could use the phrase For the Cure (a brief overview here). I love what Stephen Colbert said:
Anybody who knows me knows I am a huge supporter of the Susan G. Komen for the Cure foundation, which raises millions of dollars a year in the fight against breast cancer . . . So I’m giving a big Tip of my Hat to the Komen foundation for spending almost a million dollars a year in donor funds to sue these other groups. If they don’t own the phrase “for the Cure,” then people might donate money thinking it’s going to an organization dedicated to curing cancer, when instead it’s wasted on organizations dedicated to curing cancer.
………………………………….
By this point I was getting more and more annoyed with Komen’s corporate actions that simultaneously limited the language others used to raise money for cancer research while expanding its own pink grasp seemingly without standards. I stopped raising money for them. I felt the Komen organization was putting a happy face on breast cancer, and not paying attention to the often-unpleasant realities of life as a survivor (including recurrence). Survivorship isn’t always always smiles and pink ribbons. I wrote one of my most popular posts “These things are not tied with a pink ribbon” to capture some of those feelings:
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
………………………………….
By the time the Planned Parenthood de-funding was announced this week, I was already gone. For years, mail from Komen always went unopened, and a phone call asking if I would be re-registering a team for the Race for the Cure had been met with an emphatic No. I had left the cult of the pink ribbon, and it saddened me that I found it necessary to do so.
So this week I am grateful that I can look at my decision as the right one. When I saw Nancy Brinker (sister of Susan G Komen and the founder and CEO of Komen for the Cure) on MSNBC and how she engaged in what Barbara Boxer correctly termed “revisionist history” I was stunned (click here to either watch the video or read the transcript). This isn’t a woman who speaks for me. This isn’t a woman I want in charge of donations I make. This isn’t even, in my mind, a woman who is in touch with reality.
I’m allowed to vote with my pocketbook. I have dollars I opt to give to charity and Nancy Brinker, they don’t come to your address anymore.
Many people may be surprised this week that Komen isn’t everything they wanted from a breast cancer charity; I’m not surprised. I’m actually glad that this week has brought some of Komen’s actions to light so that others may decide how they want their dollars spent.
I think a better name for them is Susan G Komen For(got) the Cure.
*In October of 2012, the year I wrote this piece, I was diagnosed with a distant recurrence of my breast cancer… I have metastatic, incurable breast cancer. I have revised a few words in the piece to reflect my status. Since that time I’ve learned more about SGK’s history of ignoring metastatic patients in their print campaigns. Only a few years ago did they first put a person with stage IV disease in an ad, and even then they put a happy face on it, concentrating on the woman’s hope and future. That woman has since died from metastatic breast cancer. Rather than educate about the only type of breast cancer that actually KILLS (and was the cause of death of its namesake, Susan Komen), SGK has opted to again pinkwash the reality of this disease.
Some have asked where I think donations should go. Not enough money goes to research into metastatic breast cancer and advanced disease. I have established a
fund at Memorial Sloan-Kettering that is earmarked for this research. You can see my page
here for it. The money goes to research. Another good place is Metavivor.
December 14th, 2011 §
My mother retired a few years ago. For much of her adult life she was a psychologist specializing in grief and loss, death and dying. She wrote her dissertation on the impact a child’s death has on family dynamics. She used a case study method, doing in-depth interviews with surviving family members of various tragic events that happened. In one case, a house fire killed a child; in another, a baby died of SIDS.
They were heart-wrenching stories, and even as a child I could tell this was “heavy stuff.” Of course I couldn’t comprehend the magnitude of a parent’s love for his/her child until I had my own; but, I realized in reading the transcripts that grief is a multi-faceted emotion. And that loss is a process.
Having my mother work in this somewhat unusual profession was excellent training. I learned at an early age so much about sympathy, empathy, guilt, regret, and the discomfort our society feels about the subject of death. Despite the fact that it is the one thing that unites us all, the one common thread in all our lives, most people just don’t want to explore the subject of death. It makes people uncomfortable, makes them squirm, and almost universally makes people change the subject.
When you have had a death in the family, people don’t know what to say. In fact, it is likely many people won’t bring it up. Often, they worry that they will be reminding you of the tragedy, as if you have forgotten it. Anyone who has experienced a death of a loved one knows this isn’t true. The deceased person is never far from your mind, from your heart. And more often than not, you want to talk about that person. My mother taught me this. She taught me that people will never be upset if you remember and talk about the person they loved; it means their legacy lives on. Everyone wants to be remembered. You honor this desire when you talk about a deceased person.
I have said many times that growing up with my two parents was the best training for my string of illnesses through the years. While cancer has been the most serious, it has by no means been the only medical challenge I’ve had. But having a surgeon for a father and a psychologist for a mother was perfect.
I was able to digest complex medical information. When surgeons told me what needed to be done I could weigh my options methodically. I could weigh options of treatment and ask good questions to determine the best course of action for me. I could read pathology reports with ease. And then I could be insightful into my emotional response, being introspective and analytic
And being insightful and analytic about a life-threatening disease means confronting mortality. Often I hear stories of people dying without a will. In fact, often it’s only once people have children that they feel sufficiently motivated to create a will, because their love for their child (and making plans for a guardian) is the only thing that can make them confront this fear.
Often when I was in the midst of chemotherapy I wanted to have conversations about the “what ifs.”
What if they didn’t get it all.
What if the chemo doesn’t work.
What if the cancer comes back.
What if I get another (worse) kind of cancer from the chemo.
What if I die.
No one really wanted to talk about the last possibility even though it wasn’t outlandish. (Interestingly, people are very intrigued with my recurrence likelihood and mortality statistics… they view the numbers as easier to talk about in the aggregate rather than just discussing my own death).
I viewed talking about my death as responsible. I wanted to make sure Clarke understood that if I died, I wanted him to find another wife. I wanted him to be happy and loved. I wanted our children to have a mother to love them. Unsurprisingly, my greatest worries centered on my children.
I sat with a friend at coffee one day and voiced some of these concerns. With 5 children of her own, my friend is an amazing wife and mother in all respects. At first she was resistant to talk about my death with me. She didn’t want to entertain that notion. But I pressed the issue. And finally she looked me in the eye and said, “If you die, I promise I will watch over your children. I promise I will make sure they have the right person love them and raise them. I promise you that I will make sure that happens.” I think she figured it was the fastest way to shut me up. I think she figured she would agree to anything I was asking just so we could get off the subject. But at some point I think she realized that it was really important to me. I wasn’t going to let it go. And I wasn’t going to be able to get past it until I felt they would be safe and watched over. So she told me what I needed to hear. And I know she meant what she said.
Like a balloon slowly deflating, I felt my body go lax. Finally, I could let it go. She had promised me she would do for me what I wanted. I could trust her, and I could move my worry to something else. She did more for me by making this promise than she will ever know.
Here is one of the things I’ve learned from my mother: When someone you love is talking about death, don’t change the subject. Don’t trivialize their worries. Don’t say, “Let’s not talk about that now.” If they want to talk about it, it means it’s important to them, it’s weighing on them.
Focus on the fact that while we don’t need to sit around thinking about death all the time, there unfortunately might be times in our lives when we might not be able to think of anything else. If you haven’t experienced that, I applaud you. But sooner or later, you or someone you love will.
November 28th, 2011 §
This is still one of the most important posts I’ve made. One of the ways you can be a good friend to someone going through a difficult time is to use open-ended questions. In this way, you are not projecting your own feelings onto them; neither are you assuming what feelings they are having. Trust me: they’ll appreciate it.
…………………………………..
There are ways in which I will never make you as readers understand what it’s like to have cancer if you haven’t. However, part of the reason I write this blog is to try to explain some of the cancer patient “mentality” (if you’ll accept such a generalization) to those of you who haven’t had cancer. To that end, you can hopefully be better friends, partners, spouses, sons, and daughters. There are things I didn’t know before I had cancer that I wish I had understood.
It’s not that I am special. It’s not that I am so smart. It’s that I have been there. Hopefully sooner than you have. And so I am reporting back from the field. To try to help you. Prepare you. Because if there is one thing I know, one thing I know for sure: you will know someone. It might be your friend. Your parent. Your child. Or even yourself. Maybe you already know someone. But one thing is for sure: you will know someone who gets cancer. And you know what? You already know me.
One of the ways your life changes when you have had cancer is that you begin to understand the phrase “It’s never over” in a whole new way.
As soon as you hear the three words, “You have cancer” your life changes. From the time you hear those words everything is different. You now have a history of cancer — even if it’s a cancer that can be removed and you don’t need any other treatment. It is now a history that puts you at risk. Now every medical problem, every medical history you give, every question mark, every medical mystery must be filtered through the lens of a history of cancer.
A woman I know from college was writing a brief note to me by email to thank me for something nice I’d done. The last part said, “Hope you’re feeling on top of the world (or close to it).”
My reaction? First I burst out in laughter.
Ah, the naiveté of the healthy!
On top of the world! Ha!
Then it actually got me riled up.
Angry.
How dare she think it was over.
Then I got angry at myself for lashing out.
I became contrite.
Why should she know better?
How could she know better?
It isn’t fair to expect people to know better.
Only once you know better can you do better.
If she only knew.
What was I going to do?
Write back and explain to her the error in her thinking?
Should I write back and say:
I counted every day, every hour, every minute, every second to be “done.” But when each thing was “done” there was always something else I was counting toward. Always something else looming. I’m never “done.” It’s never “done.” It’s never “over.”
The language we use reveals a lot.
When someone says,
“You must be on top of the world,”
that means:
“You should be”
“You ought to be”
or
“I expect you to be.”
For someone like me, if I don’t feel like that it’s hard.
I get angry. I want to say all of the reasons why that’s not realistic– why that’s wrong. Why that’s precisely what I’m not feeling.
But then, when my anger cools, I take that and turn it inward. And all I feel is disappointment. Disappointment in myself. Maybe I should feel like that. Maybe I really should feel on top of the world. The fact that I don’t means I’m not as far through this thing as I thought. It reminds me I’ve still got a lot of work to do.
Maybe the battle is not really with cancer. Maybe it’s with myself.
But I think the point remains: just surviving cancer isn’t necessarily enough. It’s not enough to make you feel on top of the world.
You can help those who have had cancer by not making the leap that just because they have lived through this round that they have “won”; don’t assume that they will necessarily be ecstatic, “done,” and ready to move on.
Rather than telling people what they “must” feel, we all can be better friends and listeners by asking questions rather than making statements.
Rather than saying “you must feel on top of the world” think of the difference it would have made if my friend had said, “Now that your treatment and surgeries are over, how do you feel?”
An open-ended question is always a safe conversation starter. I’m going to try it more often in my everyday life; I hope you will too. My wish is that it begins some good conversations between you and someone you care about.
October 24th, 2011 §

Last week I was featured in an article by Liz Szabo in USA Today. You can find the story here. It was so much fun to see how many people saw the piece and for the kids to see themselves in a national newspaper.
The decision to have a mastectomy is not an easy one. Many men and women with breast cancer are thankful that their cancer is in a location where the tumor and surrounding tissue can be removed. When faced with cancer the reflexive reaction may be “just get the cancer out.” Statistics on recurrence and mortality rates with certain treatment options are handed over; a new language is learned, risks are assessed. How much risk is acceptable?
Dr. Susan Love, noted breast surgeon, argued in a blogpost recently that decisions by breast cancer patients to have mastectomies constitute “wishful thinking” on their part.
I agree with a few of the points Dr. Love makes, first and foremost that a mastectomy is not equivalent with a “cure” and that it does not ensure cancer will not recur. The problem is that her post really makes it sound like she is arguing with the decision.
In my case, I needed to have one breast removed; I opted to have the other removed as well.
Let me be clear: I had no delusions that a contralateral mastectomy was going to save my life or even prevent me from having a recurrence. I knew I could not control if my cancer would return. What I knew is that I could control how I treated my cancer, how I managed it, how I lived with it/after it. I knew there would be choices to be made. I knew cancer would not be a “once and done” thing for me. Survivorship means living with the ramifications of the disease, long after hair has grown back in.
I also very much agree with Dr. Love’s critique of food and eating particular items to prevent breast cancer or keep it from recurring. Dr. Love writes:
Finally, there is the wishful thinking about diet! The headlines scream that if you eat blueberries or drink red wine or don’t drink red wine you will not get breast cancer. We all want to believe this magic!
In reality, these findings come from observational studies, which show you a correlation, but cannot prove cause and effect. If you knew that all drug addicts drank milk as babies, would you really think that drinking milk as a baby could make you a drug addict? Of course not! That’s a correlation. It’s not cause and effect. Exercise and maintaining a healthy weight have been shown to reduce risk, but what you eat seems less critical.
I agree that it may be tempting to cling to food as protective and/or curative. After all, when cancer takes so much from us, there is a desire to control the factors that we can — including what we eat and drink. I can’t tell you the number of women I know whom, at the time of diagnosis or the completion of treatment, decide they will eat “clean” or “healthy” and are right back in their old ways within months. During the acute phases of surgeries, chemotherapy, and/or radiation there can be a desire to take fear and channel it. By controlling what we ingest, we must be controlling what our body does and what happens to cells, right? Dr. Love reports that this is not as strong a case as one might think.
In my own opinion, if what we ate and drank were that instrumental in determining who got cancer and who had a recurrence, we’d have a cure by now. This is not to say that we aren’t learning more about risk factors and how certain foods can affect likelihoods of getting certain cancers. But for now, we do not have the scientific evidence to support such cut and dry statments about causality with breast cancer.
She shows little insight in her post into the mental reasoning that women make when deciding their treatment options. In fact, I don’t care at all for the way she chides the reader that a diagnosis of breast cancer “is not an emergency” and we should not make a deal with the gods to exchange our breasts for a clean bill of health.
In essence, she suffers from what she has just taken us to task for… equating correlation with causation. After all, just because women want to get rid of their cancer and they opt for a mastectomy, this does not mean they are making the decisions with that tradeoff as their guide. In fact, more often than not, it’s not even necessarily a reduction in breast cancer recurrence that women are after. There are other things they do not want to go through: mammograms, MRIs, biopsies, waiting for test results… and in my case, radiation on my left side which could cause heart damage.
I quote Dr. Love at length here:
We use wishful thinking all the time when making treatment decisions. When a woman is diagnosed with breast cancer her first reaction—understandably since she is scared to death!—is to do anything she can to insure that she is cured and make the fear go away. This fear (accompanied by wishful thinking) often leads people to do things that are not supported by the science.
One example of this is the studies that show that the number of mastectomies for breast cancer has been increasing in the U.S. each year. This is not happening because doctors are finding bigger tumors, or because mastectomy is a better treatment. It is the result of wishful thinking: If I offer my breast or breasts to the gods, I will surely get my life back in exchange! If I have no breast tissue, I never have to go through this again !
In reality, a mastectomy never removes all of the breast tissue. (I am a breast surgeon, so I should know.) The breast tissue does not come neatly packaged so that it be easily removed, which is why there always is some breast tissue left behind in the skin, around the muscle, and at the edges. In reality, the local recurrence rate after mastectomy is 5 to 10% and the local recurrence rate after lumpectomy and radiation is 5 to10%! It is exactly the same! And the cure rates are the same as well.
The critical issue is getting the tumor out with a rim of normal tissue and dealing with any cells that might have escaped—which is what radiation, chemotherapy, and hormone therapy are for. It seems like the more radical the surgery the better the results should be . . . but that is really just wishful thinking!
The rollercoaster ride of cancer is not to be underestimated. Once a patient has a history of cancer, there will be frequent monitoring which brings not only potential additional radiation, but also the knowledge that if there is a question, more testing, including biopsies, will be needed. This emotional up and down means a woman must prepare herself each time that her cancer may have returned.
The main problem with Dr. Love’s piece is that she chides patients for making hasty decisions about their heath care. She reminds us that she’s a breast surgeon for thirty years, after all. And yet, with that experience and scientific background, she should know better than to lump women into one decision-making category and not divide them out based on demographic differences. Oncologists (surgical and medical) both make recommendations to patients based on many variables. Issues such as age, whether this is a first diagnosis of cancer, whether other cancers are in the patient’s medical history, grade of the cancer (how aggressive), what type (including hormone receptor status), and family history all come into play in medical decision-making.
Additionally, women may opt to have a mastectomy or double mastectomy for aesthetic reasons. Some of my initial decision to have a mastectomy on my right side was because I wanted my reconstruction to be symmetrical. After three children my breasts were looking their age. If I had a mastectomy on one side I would have needed surgery to reshape my breast to better “match” the breast that would be made with reconstructive surgery.
When confronted with breast cancer, patients get divided into two camps: there are those who want to do the most possible to treat it and there are those who want to do the least they can while still “taking care of it.” Factors of age, grade and stage of cancer, issues of radiation, reconstruction, BRCA-1 and 2 status and personality type all come into play. I personally believe that the ability to tolerate ambiguity and uncertainty is a key part of the decision-making process.
I don’t say I’m cancer-free: I never say that.
I never say a double mastectomy means I won’t get cancer again.
I know what I had.
I know what I did.
It’s about well-informed choices.
I know what might happen…
In the end, it’s not just about the statistics: it’s about the person.
October 18th, 2011 §

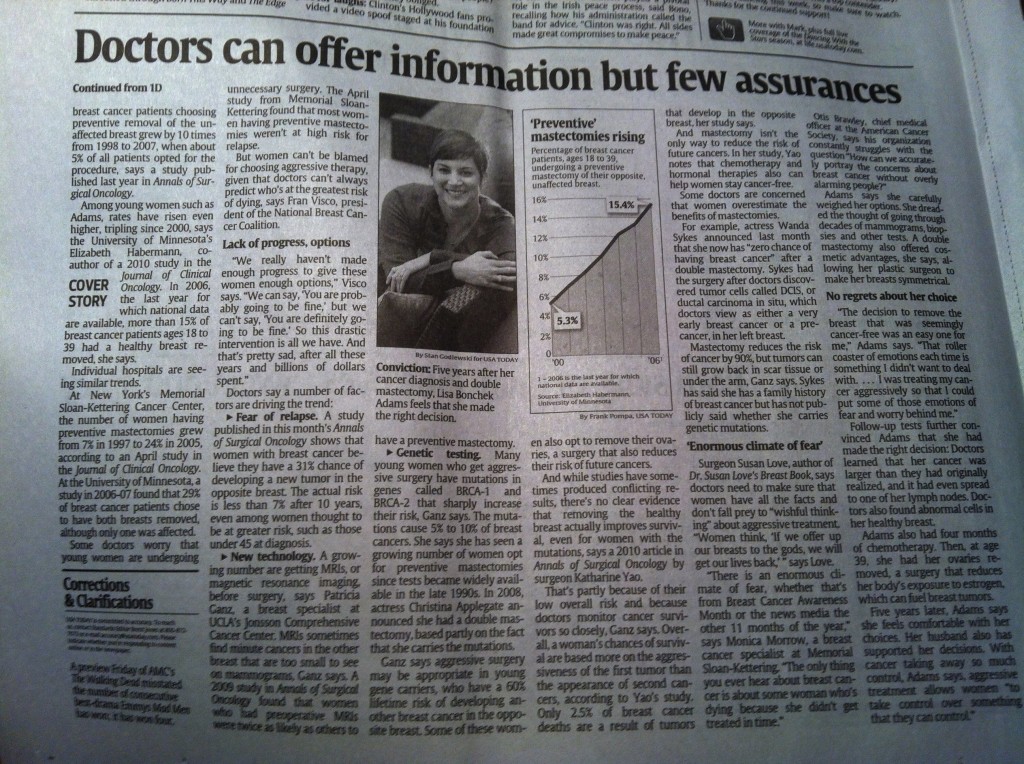
For those of you who missed it yesterday, click here to the USA Today piece that Liz Szabo did about the decision for some women with breast cancer to have a mastectomy.
Everyone was so supportive in sharing publication day with me… thank you. The enthusiasm from Facebook and Twitter friends was truly touching.
The kids feel like celebrities! The photo on the cover page of the Life section was huge and the photographer captured a great laugh with the kids. The children were so patient during the 1.5 hour photo shoot.
I’m still working on a big post with more about the subject of mastectomies for breast cancer. I promise to have that up as soon as I can.
The response was overwhelmingly positive but there were a few criticisms of my decision. Here is what I reply:
I don’t believe that my decision to have a double mastectomy was a guarantee that my cancer won’t come back. There was much I could not control about cancer; some of that uncertainty still remains. However, how you treat your cancer, live with it, and monitor it are things you can control.
The shame is that when observers (many whom have no direct experience with cancer) decide to be critical of people with the disease, survivors may be afraid to tell their stories. Cancer awareness– true awareness– can only happen when men and women with breast cancer feel comfortable enough to talk about their experiences, their choices, and their disease without fear of being challenged.
I will continue to tell my story.
September 29th, 2011 §
I hate October now. I don’t even like the color pink anymore. I get cranky in the last days of September when I start seeing everything from toilet paper to staplers colored pink and sporting a pink ribbon. It’s not that I don’t want attention called to the disease that affects so many people including me; it’s more that I think the focus has gotten misplaced. I don’t support Susan G. Komen Foundation anymore; I think they have lost their way. There is good research going on in many places, but I have come to question the line between commerce and research with Komen’s support of everything from Kentucky Fried Chicken to alcoholic beverages to its own perfume while simultaneously trying to prevent anyone else from using the phrase “For the Cure.” What happened to thinking we are all in this together, trying to achieve the same goals?
Last year I tried to think about awareness and what it means to me. I wrote this and it quickly became my most-read blogpost. It still describes how I feel, it still expresses some of the emotions I have.
…………………………………………………..
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
September 27th, 2011 §
September 29, 2010
Most of you probably read the title of this post and thought I was going to write about the guilt we may feel as parents over the course of our children’s lives when we can’t be there for every event they want us to attend or say no to things we know they might want to do.
But that’s not what I mean by “Mommy guilt.” Instead, it’s the feeling I have today because my mother is coming to visit.
I feel guilty because I have a mother who’s alive and many people I know do not.
I commented on Twitter this morning that my mother was coming for a few days. Author and friend Katie Rosman tweeted back “jealous.” Katie and I actually met because of the moving book she wrote about her own mother’s death five years ago, If You Knew Suzy. I wrote a blogpost about that book; in it I shared personal feelings about having cancer and what my legacy might be for my children.
But there was more.
Katie’s mom is dead. So is my husband’s mother. So are the mothers of many of my friends. And as I go through middle age this will happen more and more. And someday it will happen to me.
Every time I drive the fifteen minutes to the Amtrak station to pick Mom up (when she and my father don’t arrive by car here together) I think about the night I drove to get her at the train station the first time she came to visit after Barbara died.
When I saw my mother step off the train that night last year I almost had to look the other way: it was like looking at the sun.
The sight of her was
so bright,
so intense,
so welcome,
so wonderful,
that I almost had to look away for a moment.
The guilt over being able to see her step off that train and into my arms again overwhelmed me.
And so, today, when I see her again, I will hold her, kiss her, hug her. I’ll hug her for an extra moment and think to myself: this is for all of you. This is for all of you who have lost your moms and can’t do this simple act anymore. A way I can honor her and you is to appreciate these times we have together because I know there are so many who would give anything to have one of these moments with their mom again.
September 27th, 2011 §
A previous discussion about inspiration and setting an example provoked my friend Laura to write to me, “If something ever happens to me where I have to dig deep to find that strength that you have found (and shown), I will think of you. Often. And re-read your blog. Often.”
This was the highest compliment and I appreciated those words immensely. Her words got me thinking.
So many of my friends have mothers who’ve had cancer. In college, my two closest friends, Alex and Deb, both had mothers who had breast cancer. Somewhere in that experience was an expectation for them that someday, inevitably, they would have it too.
It was many years before my own mother did. And then right on her heels, so did I. Before Alex and Deb did. And so, like my mother was for me (see Everyone Needs a Trailbreaker), I suddenly became the trailbreaker for my best friends.
I’ve gone through some cancer scares with friends and acquaintances over the past three years. I’ve sat in waiting rooms, taken phone calls, written emails, met with women in person. I’ve helped friends, strangers, and friends of friends.
When I was young someone teasingly called me a walking encyclopedia. Somehow it still seems true. My husband only half-jokingly shakes his head when he hears some of the questions people ask me. He sometimes says, “They do know you’re not a doctor, right?”
I know that I’m the first of my friends to have breast cancer. And have it “bad.” The whole nine yards. That experience comes with responsibility. I know that having cancer at 37 means that I will be that resource, that friend, that support system.
In the future, others will need me. Friends will ask me how to help, what to do, what things mean.
There is a lot of pressure coming my way and I think about it already: what if I let them down?
That’s the kind of person I am.
I am already worried not only about getting through my own experience; I’m worried how I can help my friends if their time comes.
And statistically it will.
I’m worried who will be next.
I’m angry someone will be next.
I want to be the lightning rod.
I want to take in on for them.
I want to protect them.
Laura, I want to protect you:
I don’t want you to have to read my blog for strength.
I want you to read it because you want a window into a world you never have experienced. And never will.
That is my greatest hope, my greatest dream.
If I could sleep, that would be my dream:
To keep you all safe.
September 19th, 2011 §
Don’t tell me things happen for a reason.
Don’t tell me there is a plan.
Don’t tell me I’m supposed to learn a lesson from this.
Don’t tell me I’m a better person for it.
Tell me I’m strong.
Tell me I’m tough.
Tell me I did it well.
Tell me you care.
I don’t believe I was given cancer for a reason.
I don’t believe there is a master plan.
I don’t believe this is a test.
I don’t believe you only are given what you can handle.
I know I will learn lessons.
I know I will be stronger.
I know sometimes it is too much to handle.
I know sometimes I want to give up.
I know sometimes I thought dying would be easier.
I believe the power is in me.
I believe the power is in my doctors.
I believe in the power of medical science.
I believe unless you have experienced this, you cannot know.
I believe unless you’ve been there, you cannot give advice.
I believe unless you’ve felt it, you cannot judge.
I believe in the power of friendship and love to make the journey bearable.
I believe suffering is a process.
I believe in picking myself up and pressing forward.
Again.
And again.
And again.
I believe persistence pays off.
I believe in enjoying the gifts I’ve been given.
I believe many people will never understand.
It might sadden me, anger me, and frustrate me.
But in the end that does not matter.
I can only be true to myself.
I must be true to myself.
September 16th, 2011 §
September 16 is the anniversary of the death of two women I loved: my paternal grandmother, Sara, and my mother-in-law, Barbara.
Bubbe (Yiddish for “grandmother”) died in her 80s, many years ago, after her health had begun to fail. She lived in Israel, and I did not have the opportunity to see her one last time before her death. In stark contrast, Barbara died only weeks after I last saw her, laughed with her, attended a family wedding with her. We had no earthly idea she would be killed in a car crash, of course, no time to prepare ourselves for hearing the words that rocked our world.
It was Open House at my children’s elementary school that night, and when the phone rang I didn’t recognize the voice. It was my husband’s voice, strained, hiccuping, sobbing. I didn’t understand at first; I couldn’t process what he was saying. In the same way I quizzically furrowed my brow when I sat in the basement of my daughter’s school in New York City and the principal announced on that first day as our preschoolers were upstairs, “A plane has hit the World Trade Center,” I again heard information and my brain responded with Does Not Compute.
Anticipatory grief is real. A diagnosis, a doctor’s report, an assignment to hospice– all are ways others try to prepare us for the death of our loved one. With each step, with each caution, with each added conversation we start to get our minds used to the idea that it may be the end. Like a threadbare shawl we continue to wrap ourselves in, each time we are comforted less and less by others’ words of reassurance.
When a death is sudden and unexpected, there is so much to get used to, so much to process. It is a task to make sense of the death, to integrate it into our consciousness. We must unbreak habits. I remember so clearly when my uncle Alan died, I still continued to pick up the phone again and again to share a piece of news. I had to keep reminding myself, “You can’t call him anymore.”
There are so many talks I have missed with these women. There are so many things I’ve wanted to show them, share with them. However, I am so lucky to have had them in my life for as long as I did.


August 10th, 2011 §
I never wrote about cancer when I was diagnosed.
I never wrote about my body before the surgeon cut into it.
I never wrote about chemo when I was going through it.
I never wrote about dying when I was most afraid.
This morning I was angry at myself. Why didn’t I write during these times? Why didn’t I capture the raw emotion as it was happening? Why did I let this emotional gold mine slip through my fingers?
First, of course, was the pain. When I was in physical pain, I couldn’t be analytical. I couldn’t be intelligent. I couldn’t even be upright. When that pain dulled, and I started to feel better, I didn’t want to be self-indulgent. I didn’t want to think about me anymore. When I felt well, I wanted to be with my family. I wanted to give my children everything I had when I had it. I didn’t want to take time away from them, sit in my office, and write.
So I waited.
What have I gained from waiting? By writing about past experiences, am I living in the past, dwelling on it, and anchoring myself to a difficult stage of my life?
No, I quickly thought. I’m not.
In fact, it is only now that I can look at the past four years clearly. Now that the pain of recovery has shifted I can see it for what it was— for what it is.
Only now can I put the past in perspective. But what does “having perspective” really mean?
Being in the right spot makes all of the objects in your vision align properly, in correct proportion to one another. If the perspective is “off” it means you’re not viewing it from the right place.
Without perspective, your point of view is literally wrong.
What’s changed? The objects you are looking at haven’t changed. Your stance relative to them has. And in looking at the same objects from a different place, you see them differently. When we put life experiences in perspective, we are doing the same thing. By taking a few steps back, putting some distance between us and our experiences, we are better observers, we are more accurate.
My point of view was wrong before. When I was ticking off the boxes of surgeries, procedures, and treatments I was “too close” to them in space and time. Had I written about them then, I would have remembered more details of conversations, dates, and my surroundings. But that’s not what I feel passionately about. I don’t write about what it’s like to go through these things as they happen.
Gene Weingarten writes, “A writer has to figure out what that piece is before she can begin to report her story. Only then can she know what questions to ask and what things to notice; only then will she see how to test her thesis and how to change it if it is wrong. That’s what nonfiction storytelling is about. It is not enough for you to observe and report: You must also think.”
I love to write about what life is like after these events happen– after you live through them and come out the other side… how you go on after, and what it feels like when you look back.
I can see this part more clearly because my emotions are separated from the pain, from the chaos, from the shock.
For a moment I regretted that I didn’t write about all of this while it was happening. Now I know it was the right thing to do for me. Only now, with a bit of distance, can I put it all in perspective.
July 14th, 2011 §
Sunday will be the four year anniversary of the day I had breast recontruction surgery after cancer. My tissue expanders were removed once chemotherapy was over and my silicone implants were put in. Last week I had my annual visit to my plastic/reconstructive surgeon and received the all-clear to now have a visit every two years. It’s always gratifying when the time in between visits gets longer; I remember when I was there at least once a week during the reconstruction process.
“Did you know it’s been four years since your surgery?” my surgeon asked. Immediately he chuckled, “Of course you know that,” he said, realizing my mental calendar was certainly more precise than his– of course I marked the days off in my head.
Whenever I sit in a waiting room I am instantly transported to that place and time. I sit and watch patients walking in and walking out. I can tell by hearing what the time interval until their next appointment what stage of treatment they are in.
I sit in the chair, the same one I did four years ago.
It’s the same chair, but I am not the same person.
My body is not the same.
There is continuity in that chair.
There is a story it tells me.
I wrote this piece to the next person who sits in that chair.
………………………….
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
A cure.
Don’t you think that would be amazing?
I think so too.
July 5th, 2011 §
I met a woman who told me something shocking.
It wasn’t that she’d had breast cancer.
Or had a double mastectomy with the TRAM flap procedure for reconstruction.
Or that she’d had chemotherapy.
What made my jaw literally drop open was her statement that she has never told the younger two of her four children that she’s had cancer.
Ever.
Not when she was diagnosed.
Or recovering from any of her surgeries.
Or undergoing chemotherapy.
She never told them.
To this day– five years later– they do not know.
I like to think I’m pretty open-minded. But I confess, it took a lot of self-control not to blurt out, “I think that is a big mistake.”
I’m a big believer in being open and honest with your children about having cancer. My caveat, using common sense, is that you should only give them age-appropriate information.
When I was diagnosed with breast cancer Tristan was six months old. Of course he didn’t understand what cancer was. Colin, age 5 at the time, understood some of what was happening. I explained to him what cancer meant, that I was going to need surgery to take the cancer out, where the cancer was, what chemo was, what it would do to my appearance and energy level. Using words like “I will be more tired than I usually am. I might feel sick to my stomach and need to rest more” explained things in words he could understand.
Age 8 and the oldest at the time, Paige understood the most when I was diagnosed. She had bigger questions and well as concerns about me (“Will I get it too? Who is going to take care of us? Are you going to be okay?”).
It’s not that I think small children always understand everything. But they are certainly able to sense that things are not “normal.” They can tell when people are acting strange. I think it’s important that they know there is a reason for that change. Children have a tendency to be egocentric; they think that everything is their fault. They may think they have done something wrong if everything at home feels different.
The woman told me she didn’t want to worry her children. She thought it “unnecessary” to tell them. She said when they got older she would explain it. I argue that by keeping her cancer a secret, she runs the risk of doing the opposite: making cancer seem scarier and more worrisome.
If children hear words like “cancer” casually in conversation as they grow up they will be comfortable with them; in that way, they won’t be frightened of them. If they understand the truth of the diagnosis and treatment they are dealing with reality. By hiding the truth, the unintended consequence is to make it seem worse than it is. By not telling children, and waiting until they are older, it reinforces the idea that cancer IS something “big and scary.” After all, if it weren’t, you would have told them already.
I think being secretive is a step backward to the days when cancer was only talked about in hushed tones: the “C” word or “a long illness.” These concepts might seem primitive to us now, but it wasn’t long ago that these vague labels were the norm. By showing our children, our friends, our neighbors, that we can live with cancer, live after cancer, we put cancer in its rightful place.
To me, the deception that goes on to lie to children about where you are going, what you are doing is lying about a fundamental part of your life. Cancer isn’t all I am — but it is a part. And it’s an important part of my medical history. If for the past 3 years I’d covered up where I was going and what I was doing, the web of deceit would have been extensive. I can’t (and won’t) live a life like that.
Further, I think it’s a poor example to set for my children.
Lying,
covering up information,
and omitting important information are all wrong.
With rare exception, the truth is always best.
Presented in the proper way,
commensurate with a child’s age,
a difficult situation can be not only tolerable but surmountable.
It takes work. It takes parents who can manage not only their own emotions about having cancer but also be involved with helping their children cope with it. It’s more work, but it’s worth it.
I think that woman made a mistake. I think her decision was harmful. I am sure she thinks she was doing her children a favor. I totally disagree. I think keeping this type of information from children “in their own best interest” is rarely– if ever– the right thing to do.
April 9, 2010
June 30th, 2011 §
It’s not that I didn’t like my right breast.
It hadn’t really ever done anything “bad” to me, except for the few times when it wouldn’t keep up with the milk production of the left one during the months when I nursed my children.
I didn’t harbor any negative feelings for it. In fact, I didn’t think about my breasts much at all except to chuckle at the sagging that inevitably comes with middle age and three pregnancies.
But all of that changed with four words: You have breast cancer.
The cancer was in my left breast: I needed a mastectomy. But what about the “good” breast?
Note the popular lingo: the non-cancerous breast quickly becomes tagged as the good one– like a good child who behaves and does what it’s told, the non-cancerous breast has faithfully done its duty and stayed healthy.
The left breast?
Well, that’s the traitor.
I had a decision: what would I do with the right breast?
Keep it?
Toss it out in biohazard trash?
With four words, that part of my body became a liability. I didn’t want that breast anymore, thanks. I’d rather have no breasts than one. Mentally, it was much easier to me to part with both, not live the rest of my life in fear of what might be lurking in that tissue.
To be clear, surgeons and oncologists explained that in their opinion, my chance of getting cancer in the right breast was no higher than my chance of getting breast cancer in the first place; I wasn’t necessarily at increased risk of breast cancer on the other side.
But:
I had already been a statistical anomaly.
I had gotten cancer at 37.
I was BRCA-1 and 2 negative (but didn’t know it at the time).
In my mind I thought:
Go ahead and tell me that, but I don’t believe you.
And so I heard their words.
I understood their words.
But I didn’t believe them.
And time proved me right.
I opted for bilateral mastectomies. And when the pathology came back, there was abnormal tube proliferation and some cell dysplasia. Things were awry in my right breast even though nothing had shown up on the mammogram.
Now, yes, eventually I would have found the problems when the cell proliferation got large enough to be detected on a mammogram or MRI. And maybe my chemotherapy would have gotten these cells anyway.
But are you really going to take that chance?
I wasn’t.
Body parts become liabilities.
My perspective about my body has changed so much in the last four years. My body itself has changed so much too.
I’m not exaggerating when I say that, like aging itself, the side effects of removing my ovaries one year after my mastectomies has changed almost everything about my health as I know it.
I went to the kitchen just now and pulled out my binder of cancer records to double-check my pathology report to write this blogpost.
And there it says, quite plainly, that my cancer was 1 mm from the deep margin (chest wall).
One millimeter.
A hair’s diameter.
A grain of sugar.
It always takes my breath away.
A millimeter.
So many people link their happiness to pounds, or inches, or dollars.
Me?
I think part of my future might hinge on that millimeter.
I’m counting on it.
And moving forward.
June 12th, 2011 §
Cancer is not one disease and there is more than one way of coping with a diagnosis. While some patients research every aspect of their illness, treatment, and prognosis, others would rather have their physicians sift through information and chart a particular course of action for them.
While many people with cancer or other illnesses may agree on what they like to hear (or not hear) from friends, family, and acquaintances, Bruce Feiler’s New York Times piece “‘You Look Great’ and Other Lies” falls victim to assuming that just because it is true for Bruce means it’s true for all. While he does use “many” and “most” throughout the piece, his list is prefaced by “Six Things You Should Never Say to a Friend (or Relative or Colleague) Who’s Sick.” If Feiler’s piece were a blogpost I might not feel the need to react in such detail; however, as a highly visible piece, I suspect there are many readers saying to themselves, “I say a lot of those things… was I really that wrong?” All day yesterday my Twitter followers were asking my opinion about the piece; they wondered if he was right.
I recognize that there is a lot of good advice in his piece, and I want to acknowledge how hard it is to write a short article about such an important and personal topic. I think that opening up this subject to a larger discussion may allow readers to see the variation in reactions: remarks are interpreted in a variety of ways by different listeners. Even the same remark may be interpreted as harmless one day and loaded the next; hard and fast rules are unlikely to apply.
Thus far on my blog I have resisted writing rules about what people should and should not say. Readers have forwarded many such lists to me for my opinion. At the time I was diagnosed, I was the first of my friends to have cancer; I didn’t have anyone I could ask for advice.
I was often annoyed with the comments people made. I felt some were just silly (“It must be nice to be able to have time to rest in bed during chemo”) while other comments seemed hurtful or downright rude (“Is your cancer what is going kill you?”). While I was frequently upset or offended by statements people made, I didn’t articulate a list like Feiler’s. Why? While I reacted negatively to some things people said, I still felt that in most cases their intentions were good. That is, they might have made comments that were not helpful, but they weren’t making them to be hurtful. They might have been nervous, naïve, or clueless, but they weren’t trying to be cruel.
While the hope is that people will think before they speak, saying “these are the things you must not say” will make people even more self-conscious. The danger is that people will do something even worse than the things Feiler mentions: they may remain silent and not offer any help or express any affection at all for fear of saying the wrong thing.
Many people don’t know what to say. It’s wonderful to have some suggestions of what you should say as Feiler does (and I think he’s spot-on with every one of those). The danger of criticizing in harsh terms is that every person you’ve interacted with then feels the need to ask, “Are you talking about me?” At that point you are put in the position of consoling those who should be helping you. Frequently I found myself in the position of comforting others about my own diagnosis or that of one of their relatives. My recommendation is to avoid telling a person with cancer about your friend or relative who either had it and has lived 20 years (implies their fears are unwarranted) or that a person you know died a terrible death (discouraging).
One main criticism of Feiler’s piece is that it makes no distinction of or allowance for social proximity. That is, the expectations we have for what others should say to or do for us varies in relation to how close we are to them. It may be reasonable to expect a spouse or best friend to clean your refrigerator but not for your child’s teacher to do so.
Now, on to more actual details of the piece.
It’s interesting that Feiler assumes the offer of food is innocuous. He claims food was one of his great helps and implies that this is a safe way to offer help to those in need. I explicitly forbade food to be brought to my house. I didn’t want anyone spending time or money preparing or purchasing food that might not get eaten. One friend reported that while her son was being treated for leukemia, well-wishers sent so many lasagnas that her kids could no longer look at the dish after a few weeks of receiving them. Similarly, smells eminating from food can often be offensive during chemotherapy.
Feiler starts his list of helpful speech and behavior by outlawing the questions, “What can I do to help?” and “My thoughts and prayers are with you.” he tells readers, “Just do something for the patient… Want to be really helpful? Clean out my fridge, replace my light bulbs, unpot my dead plants, change my oil.” Gee, I’d like someone to do those things for me even when I am not sick!
These things are not only unrealistic in most cases (live far away, don’t have a spare key to the house) but also impractical. These sound like suggestions for close family and spouses/partners. Perhaps saying, “Where’s your to do list—I’ll pick something off of that” might be more reasonable. I don’t want anyone in my house, actually, and how can you know what to do unless you ask?
To me, asking “what can I do to help” is not the same to me as “Call if I can do anything.” His point is that it “puts the burden back” on the person who is sick to come up with a way to help. I predict most people have their mental “to do” list available and could reel off a few suggestions to those who would offer. Close friends can just “do” or insist in a way that others can’t. I do agree with him that being more forceful about helping is the right way to go, just not to the degree he does. Taking children for playdates (phrased as “We’d love to have your child over, please let us/we won’t take no for an answer”) is a lot more likely to receive approval than, “What can I do to help?”
Further, those who are ill may take pride in being able to accomplish a task themselves. I wanted to be able to do small tasts to contribute to taking care of the house. It’s not realistic to think an acquaintance is going to march into your home and scrub your toilet; after all, it’s hard enough to get those who actually make the mess and live there to do it. Arranging for a cleaning service to come might be more helpful. Often it’s easier to allow strangers into the home than friends; and it could be done while the person it at chemo treatment, for example. (with care taken about fumes and smells that might trigger nausea). Offering to do grocery shopping or be available to receive an online grocery delivery might be good, too. There is a whole post I could write about suggestions for how to help a friend.
Feiler also outlaws “My thoughts and prayers are with you.” He writes, “In my experience, some people think about you, which is nice. Others pray for you, which is equally comforting. But the majority of people who say they’re sending ‘thoughts and prayers’ are just falling back on a mindless cliché.”
First, I think this is an extrememly personal reaction. How a person deals with severe illness is highly charged. In my case, I don’t want your prayers under any circumstances. I don’t believe in God and I don’t want you to pray for me. I didn’t tell anyone not to do it; after all, it made them feel that they were doing something for me. However, it also smacked of illogicality; why pray now? The damage is done: I’ve got cancer. I don’t believe that your prayers will make the difference as to whether I live or die from it; after all, I am quite sure that the people who die from cancer every day have people praying for them, too. Feiler assumes again that what is good for him is good for all– not all people with cancer will find prayers comforting. It’s a bit confusing because he also says it’s something not to say; I’m not sure where he really falls on this matter.
Second, when someone says, “My thoughts are with you” (a phrase I use often and am not about to stop) I think it can be nice. When you live far away or don’t know someone well it can an expression said with genuine concern; when said to a close friend or family member it expresses affection while feeling powerless in such a terrible situation. I believe that to be true.
I counsel: empty phrases said without emotional authenticity are likely to fall flat with the recipient. But I think telling people not to say, “I’m thinking of you” is extreme.
I wholeheartedly agree with his #3 (“Did you try that mango colonic I recommended?”), #4 (“Everything will be o.k.”), and #5 (“How are we today?”): double emphasis on numbers 3 and 4.
Then we come to #6 (“You look great”). This is the one the title points to as “a lie.” One major criticism of the piece is that “You look great” is not necessarily a lie (and I believe the compliment most often is true). I think what Feiler is sensitive to is that we have no way of knowing if it is in our particular case that someone is lying or not. Even in the midst of terrible sickness it’s likely the speaker means “considering everything you’ve been through” which can still be an honest compliment. Also, many people appreciate being told they look great, even if the truth is questionable. Some days it doesn’t take much to lift your spirits. In the piece Jennifer Goodman Linn said, “When people comment on my appearance it reminds me that I don’t look good.” She is convinced she looks bad and doubts the honesty of the comment. Why can’t it be that she does look good? Why isn’t there room to compliment anyone on how they are dealing with things?
As I see it the real core of the problem is that “you look great” might imply that “you can’t be that sick.” Observers are trying to reconcile the disease inside with the appearance outside. When pictures of Gabby Giffords emerged yesterday, for example, everyone including newspapers commented “how great she looks.” I did not. While I thought it, and believe it (I guess Ms. Linn would find that impossible to believe), I didn’t say it because I was not trying to undermine the seriousness of her condition. Just because she looks good doesn’t mean she isn’t terribly affected cognitively and physically by the aftermath of being shot in the head. Just like when your hair grows back after chemo and everyone takes this to mean you are “all better,” serious medical situations can be present even when not visible to outsiders.
I loved when people told me I looked good. I looked sick, of course. But the effort I took to put makeup on or compliments to how I wore a scarf to coordinate with my outfit were nice. On a day I felt sad I always loved a compliment.
The irony is that illnesses that are invisible can be harder to live with. “I know you are sick but you look so healthy” is not helpful. It’s always disconcerting when someone who “looks healthy” is diagnosed with a serious disease or dies suddenly. These situations strike fear in all of us because being healthy makes us feel protected. When someone looks like us but is concealing serious sickness it can make us feel vulnerable– but that is not the patient’s problem. I again revert to the advice that you should say what you honestly believe. I don’t think it’s always a lie and I don’t think it should be on the list of outlawed expressions.
“People reminded me that I had a free ‘No’ clause whenever I needed it,” said one person in Feiler’s piece. My advice: let those who need to use it do so. When a friend got her own diagnosis of breast cancer, she assumed she would easily be able to opt out of being a Girl Scout troop leader during surgery and chemotherapy time. Instead, she was not given a gracious “pass” and no one offered to fill her spot (that would have been one way to really help). Instead, “But you’re still going to be able to be a leader, right?” was the reaction that met her.
I totally agree with the suggestions Feiler makes for things to say (Don’t write me back, I should be going now, Would you like some gossip, and I love you). I think there are more, but I think he’s got some perfect ones to start a list there.
Elsewhere I’ve asked readers to contribute the strangest/rudest things people said to them when they (or a loved one) had a serious illness. Some of the responses there are definitely statments I would caution people to think twice about saying. I also heard:
“Is it terminal?”
“What’s your prognosis?”
“It could be worse, you know.”
“Everything happens for a reason.”
“It’s all part of a larger plan.”
“Now that you’ve been through this you’re due for some good things to happen.”
“I’m sure it’s fine/I’m sure it’s nothing” (similar to Feiler’s “Everything will be okay”). And there are many more.
There is an anger that can divide friends and family once a person is diagnosed with an illness. “You just don’t get it” or “You wouldn’t understand” can be a common refrain whether silently or outwardly expressed. The same words spoken by a friend/acquaintance/colleague may be interpreted differently depending on the day or mood of the patient. I quickly learned that physical pain and emotional agony trumped all; I had little patience or care for others when I was hurting. I learned to withdraw during those times or only discuss it with those who did understand. My hypersensitivity was undestandable but not necessarily easy to be around. The desire to be understood is part of how the ill connect, attract, and cling to one another. The fact that most people with a serious illness can rattle off offensive or ineffectual questions or comments made to them means they are important.
Feiler’s piece struck me as one in which his feelings of “you just don’t get it” were overwhelming and raw. While much of the advice is good, in the end I am critical of him for the same reason I didn’t make such a list during treatment: if you go around telling people how what they did was so wrong all the time, and things they should never do, soon enough they won’t say anything for fear of disappointing or offending you. In those cases you may lose people who may have been well-intentioned. Sometimes forgiveness and compassion need to go out from the person who is sick and not just flow to them. I guess I shouldn’t say that will work for everyone, but that’s what works for me.
June 6th, 2011 §
The rest of my family is coming back today. After a week in Jackson Hole, Clarke and Paige and Colin will return tonight, just in time for Colin’s 7th birthday tomorrow.
The refrigerator has been really empty this week. With just a 2-year old and me, it doesn’t take much to keep us fed. So I took the opportunity this morning to clean out the refrigerator and freezer– really clean them. Take everything out, throw away all the junk, the ice cream that now is just ice crystals. I tossed all of those “placeholders” that you never eat, they just take up room.
As I sprayed a wonderful new lemon verbena spray on the glass shelves, I start contemplating this week. The last seven days were my week to recover from surgery (an oophorectomy), to get stronger, to close out my year. I know I made the right decision not to join my family in Wyoming this year. It’s been a reflective time, a time for my soul to be quiet and heal. I think it’s done that a little. I think another week might help. I’ve loved my one-on-one time with Tristan; we have a nice little routine going, and I feel like he’s grown up this week.
But as the new year starts, of course, we are pushed to reflect on ourselves, to make ourselves better in the next 365 days. We reflexively reflect on whether we’ve kept any of those elusive resolutions from the previous year. December 31st is supposed to bring “closure.” In the arbitrary distinction between one year and the next (after all, why is there really a difference between the last day of 2008 and the first of 2009 any more so than any other passage of midnight on any other day of the year), we are pushed to wipe the slate clean and start anew. As I cleaned the house this week, purging old canned goods, papers, clothing, and sprucing up the house I found I was instinctively doing this: “Out with the old, in with the new.”
This annual rehabilitation, then, is supposed to be psychological and physical.
Most of our resolutions are about ways we want to be better, inside and out: concentrating on the new and gaining closure on the past.
One of my dearest friends wrote to me in an email last week, “And yet, you can no more gain ‘closure’ on life-altering events than you can erase moments from your memory.” I read that sentence many times. It is beautiful, and true.
I remember well when my friend Alex’s father died of cancer almost 10 years ago. She was so busy with all of the things that needed to be done, the arrangements that needed to be made, and taking care of her mother who needed constant attention and support. I remember wondering when she was going to grieve. I worried that his death, and his absence from her life, would fester and haunt her.
As I scrubbed the refrigerator shelves this morning I realized that you never grieve the way you think you should.
No one really just sits alone and thinks about the tragedies that befall them.
It’s too painful, too powerful to take that in as one big gulp.
Instead, what we do is weave it into the tapestry of our consciousness.
We make it part of our daily life, quiet, but present.
Maybe at this time of year we reflect more than usual, and maybe that’s why the holidays are painful as we take stock of what we’ve lost during the year and what we’ve gained.
Where that balance lands says a lot.
A year ago I thought surely 2008 would be better than 2007. It really didn’t turn out that way. But I am doggedly optimistic even when I’ve been been proven wrong so many times. I do not believe that there is a “justice meter” in the universe that is going to now dump things on someone else and leave me alone for a year. But maybe as my own tapestry of consciousness keeps getting woven, it will be stronger and more resilient to keep me going this year.
At least I’m starting with a clean refrigerator.
originally written January 2, 2009. Modified June 6, 2011
June 3rd, 2011 §
More often than not, cancer creeps into conversations with friends. New friends, old friends.
I don’t think I’m obsessed with it. I don’t have to talk about it. Why does it come up?
Is there a cancer radar?
Is it just that when cancer folks are together we let our guard down to share?
Do we want to compare notes and try to get information from each other?
Probably all of the above.
Here’s also where I think it comes from: talking about illness is grounding. It puts the emphasis where it should be. I have many friends who have family members who either have had or currently have cancer. We’re a club. There is a support we can provide for each other, a language we can speak. Stages, grades, blood counts, oncologists, PET scans, MRIs, tumor markers… and on it goes. I really think I should get credit for CSL… cancer as a second language.
I like people who “get it”; I find more and more that I am naturally drawn to them. I’m rarely surprised to find that new friends of mine have had some type of hardship in their lives.
Maybe it’s just that more and more people have “something” in their life story.
Maybe those are the people I gravitate to.
Maybe they are drawn to me (or the “vacuous people need not talk to me” sign I have on my back scares others away).
It’s not that I don’t like talking about shoes or The Bachelorette or movies. I do– a lot. And I actually do think they matter. It’s important to have a break from the heavy, serious stuff. Some people think that the small stuff is all there is– that it matters. Those people are hard for me to take.
One day, shortly after I was diagnosed, I sat watching my son take a tennis lesson. I was still numb and reeling from the news that I had cancer. I hadn’t started chemo, and was still awaiting surgery. I knew what I was facing: double mastectomy and chemo. But to the outside world I looked totally normal; no one would know what news I had received.
There were two moms sitting near me chatting loudly while their kids had their lesson. These were the days before the recession, when women in my town were flush with cash, and living high on the hog. They were talking about vacations. “I just can’t decide where we should go for vacations this year,” one said, “John has so many vacation days it’s going to be hard to use them all. We could go to Switzerland again. But that’s kind of boring. And there’s the Caribbean. But I kind of want to do something different. What do you think?” she said to her friend.
I know what I thought. I thought someone needed to hogtie me to the chair before I punched her out. That was a problem? It was one of the few times I really wanted to say “Lady, let me tell you about a problem.” But I didn’t.
Why?
Because maybe her mammogram was the next day.
Maybe she was a day from being told there was something suspicious on it.
Maybe she was a week away from having a biopsy.
Maybe she was a month from having a double mastectomy.
Maybe she was six weeks from starting chemo.
Maybe she was just about to learn the lessons I was learning.
May 18th, 2011 §
A few weeks ago I was talking with a friend about our blogs. She said that she never writes about her husband; some readers didn’t even know she was married. I don’t directly write about my husband Clarke often. I’ve written endlessly about his mother Barbara’s sudden death in a car crash in 2009 (if you want to read more about her, please click on the tag “Barbara” on the lower right of the page) but not about Clarke. Clarke is private, and I respect the fact that he doesn’t want to write or discuss topics that I do.
Clarke wrote a piece that I treasure. In 2009 he nominated me as a “Brave Chick” for a website that celebrated women who had tackled adversity (www.onebravechick.com). The interesting thing to me as I re-read the essay now is how much more has happened since then. We’ve had many medical and emotional challenges since this letter was written. I like to think that the seeds of strength were sown during some of these experiences.
I am re-posting this today not to celebrate myself, but rather to celebrate my husband. We are a team in this thing called life and I couldn’t do it without him. I hope I will get him back here on the blog sometime to write about some more of the issues we have dealt with; I think hearing it from his point of view might be helpful for some readers. But for now I will let his words sing, and hopefully honor him by doing so.
…………………………………..
“The bravest sight in the world is to see a great man (or woman) struggling against adversity.”
-Seneca
“Let us do our duty, in our shop in our kitchen, in the market, the street, the office, the school, the home, just as faithfully as if we stood in the front rank of some great battle, and knew that victory for mankind depends on our bravery, strength, and skill. When we do that, the humblest of us will be serving in that great army which achieves the welfare of the world”
-William Makepeace Thackeray
My wife Lisa and I met for the very first time at the George Foreman / Evander Holyfield fight in the spring of 1991 when, in a scene straight out of Rocky, a forty-two year old Foreman went the distance with the undefeated Holyfield. We met again at a Halloween party later that year and began dating. We got engaged in 1995 and married in the summer of the 1997. Over the course of our 18 years together and in particular the last three, it has become clear to me that my wife possesses more than her share of courage.
As with any 18 year period we have had our ups and downs together but mostly it has been up. We have three beautiful and intelligent children, loving and supportive families and great friends.
In the grand scheme of things, our life together was pretty smooth which is why I think we were completely unprepared for what the last three years have brought us. In August of 2006 we learned that our five month old baby boy was born with a condition that required immediate open heart surgery. He also had complex problems with his cervical vertebrae and the muscles of his hands that would require a significant ongoing investment of time and energy in medical care and therapy.
Since Lisa is at home with the kids when I’m at work, the day-to-day heavy lifting of running the house and managing the often crazy logistics of our lives naturally fall to her. In addition, because she is the medically savvy one in our family (her father is a surgeon and her mother is a psychologist), Lisa ended up quarterbacking and supervising Tristan’s care which included (and still does include to some extent) coordinating treatment with four or five different specialists (neurologists, pulmonary specialists, pediatric cardiothoracic and orthopedic surgeons, etc.) in three different cities. Juggling all of those competing priorities was extremely challenging and time-consuming. It seemed like fate was piling on hardship in January of 2007 when Lisa was diagnosed with Stage II breast cancer.
Lisa spent much of 2007 aggressively treating her cancer with a double mastectomy and chemotherapy. I’m sure many women who read your website are acquainted with the harsh reality of how tough a cancer treatment regimen can be on one’s body and, just as importantly, one’s psyche. I must confess that I wasn’t really prepared for what was to follow. Like many things, cancer treatment seems much simpler in the abstract or on television than in the messy reality of real life. It is a process where you are forced to make life-changing and often heartbreaking decisions while in possession of only limited information all the while dealing with the physical, mental, and emotional side effects of disease itself and the treatment. If adversity is the test by which character is revealed then I’m proud to say that my bride has passed her personal test with flying colors.
At least by the romanticized ideals of literature or history you don’t get to see real bravery very often when you live in Darien, Connecticut (braving the long lines at the local Starbucks doesn’t really count). However, there was something quietly heroic in how Lisa handled the myriad of issues she was dealing with in a thoughtful and calm (with some exceptions) manner all the while taking care of the thousand little details that go along with being a mom to a young family. No matter how much personal pain she was in, the kids’ lunches got made, their homework got done, their boo-boos got kissed, and their very real fears addressed and soothed even on the very worst days. Tending to young kids isn’t easy on your best day but being able to do so and face the world in the midst of cancer and chemo and all that implies is something else altogether.
Looking back, the amazing thing to me is how little impact the whole period had on our children; that speaks to how much of her energy and force of will Lisa put into ensuring that that was the case. We had lots of help from our families and our amazing group of friends, but at the center was Lisa getting up each day and doing her best to move forward with grace and determination (kind of like a 42 year-old George Foreman coming out of his corner, taking his licks and getting in some good shots of his own). In my book, that is all any of us can really expect of ourselves and defines what bravery is all about. When my test comes, I hope I do as well and face up to it with as much strength as Lisa did.
A friend whose wife had just gone through the breast cancer experience told me when I learned about Lisa’s diagnosis “the thing about breast cancer (pardon another tortured sports metaphor) is that you never get to spike the ball in the end zone and say you are done. There is always something else.” I thought I understood what he was saying at the time, but I appreciate it much more now. Although chemo ended in the summer of 2007 and her breast reconstruction finished shortly thereafter, Lisa has been dealing with the often frustrating regimen of drugs and side effects that come along with being a cancer survivor. While things are certainly better than they were, it has been a constant challenge and adjustment for both of us.
As I said earlier, one of the most difficult things about having cancer, even a cancer that is as common and well known as breast cancer, is that you really don’t have any idea what is ahead of you as either a patient or a spouse when you begin the process. There are reams of data and academic studies available but despite that fact, it is difficult to distill and digest all of that into a coherent picture as to what you as an individual (or the spouse of one) will experience.
As part of her life as a cancer survivor, Lisa has taken it upon herself to make understanding the long road of treatment, recovery, and being your own best advocate a little easier for women who will face the same challenges she did. She spends hours and hours speaking to women in our community who are just beginning the process about what she has been through in the hopes it will help them be prepared. As an extension of those conversations she began writing (and later blogging) about her experiences and feelings about cancer and posting them on the web. She sometimes writes clinically about the nitty-gritty medical realities of treatment and recovery which are based on her personal experiences, extensive research of the available medical literature, and her own conversations with her doctors.
Other times she examines the darker, emotional, frustrating, and deeply personal places that being a cancer survivor can sometimes bring you as young woman and a young mom. Her writing is often beautiful and poetic and is always thoughtful and enlightening. She puts it all “out there” for public scrutiny. She posts regularly under her own name to help her fellow women (our moms and sisters and daughters) understand and deal with a path that all too many of them will walk down at some point in their lives. I believe this is noble and selfless and courageous.
So as a very small and modest way of acknowledging her daily efforts and recognizing her achievements, I would like to nominate Lisa Adams (age 39), loving wife, wonderful mother, caring friend, talented writer, and strong cancer survivor to be a featured brave chick. I would invite those members of your community who are interested to check out her writing at lisabadams.com.
Thanks for your time and dedication to Brave Chicks everywhere.
Clarke Adams
July 7, 2009
May 4th, 2011 §
I decided to repost this old piece after reading Katie Rosman’s Wall Street Journal piece “Read It and Weep, Crybaby”
September 3, 2009
It’s 11:30 in the morning and I’ve already done it once today. Cried. Not sobs. But a quiet, empathetic cry. Large tears welling.
It happens less than it used to. I have gotten better at managing it. I can now get to the point where I well up, but the tears don’t actually spill out and run down my cheeks.
It’s progress.
That difference seems to make people less uncomfortable. My doctors are used to it; they know I well up. I figure if you’re dealing with cancer patients you are used to seeing lots of crying– you must have a coping mechanism. Maybe it doesn’t even register anymore. Maybe they are immune to it. I see tissue boxes in all of their offices so it’s likely a common occurrence.
There are certain subjects guaranteed to make me cry.
Tops on the list?
My parents; my mother in particular. Raise the subject of anything happening to my mother— any illness, any harm, most especially her death– these words if spoken aloud instantly make me cry.
My mother is, to me, a prized possession, a beloved security blanket that must remain complete and undamaged.
Other topics do it too.
Today the trigger was talking about a specific day I was bald in front of my plastic surgeon. I remember the way I felt stripped of every ounce of dignity in a way that being naked, topless, breastless countless times in his presence had never made me feel. Obviously I can still connect to that emotion.
I still remember that feeling of being naked. Not clothes-less, but dignity-less, bare of everything that held me together as me. Sitting in a coffeeshop with music playing and the sun shining and my friend sitting with me, I could still feel that feeling two years later.
I could still feel it. And I cried.
I cried for the friend I was with, herself recently diagnosed with breast cancer.
I cried because I didn’t want her to have to feel it too.
I cry for her sometimes. I cry because I want to protect her. I want to be the pit bull. I want to stand guard at her driveway, at her mailbox.
“NO!” I want to yell.
“You cannot have her,” I want to say to the intruder.
To cancer.
To all of the things she might have ahead of her that will cause her pain.
Silly, perhaps.
Childish, perhaps.
But that’s how I feel.
I bet that’s how she feels.
I know that’s how I felt.
As a person with cancer you wake up and think,
You know what?
I don’t want to have cancer today.
I want to take a day off.
I don’t want to go to any doctors.
I don’t want to make appointments.
I don’t want to talk about cancer.
And even though I can’t seem to talk about anything else,
I don’t want to talk about it.
I just want to stay in my pajamas all day
and eat peanut butter from the jar with a spoon
and have the world go on without me
because I don’t want to participate today.
I just want a “sit it out today” note from my mom
so I can just take a break today…
and maybe tomorrow too…
I want to protect my friend.
We moms are good at that.
My daughter started middle school. On the second day she came home and started in on her math homework. Within minutes she was in tears. She got frustrated and started crying. The teacher had given them a very hard sheet of problems and told them to see what they could do. Some of them were complex probability and statistics questions. She brought them to me and was frustrated. I didn’t laugh at her. Or even criticize her for over-reacting. I knew what she was feeling. I knew it was the “everyone else knows what they are doing and I’m the only one who doesn’t” syndrome. I knew that, like me, when frustration takes hold, our kind doesn’t get angry, we get emotional.
It’s not a great trait; it is especially hard for men to deal with. For husbands. For fathers.
My father used to go crazy when I started crying. It was just an irrational, irrelevant act he had to deal with. A distraction.
I know if my husband had been there he would have told our daughter to stop crying. I know the tendency won’t serve her well.
I always think of Tom Hanks’s character Jimmy Dugan in A League of Their Own when he yells “There’s no crying in baseball!”
It’s a good thing there wasn’t a sign on my oncologist’s door that said “There’s no crying in cancer.” Some days I think it’s a necessary part. I think it’s healthy. For me anyway.
I’ve cried on Saturdays.
On my birthday.
I’ve had breakdowns stringing Christmas lights on the trees in my yard when I just couldn’t get it right.
I’ve kicked the tires of my car.
I’ve slammed doors.
I’ve screamed to the sky.
I’ve sworn a blue streak.
I’ve cried so hard my stomach turned inside out and I’ve retched and collapsed because I just couldn’t hold myself up anymore.
I’ve dreaded the night-time because I knew I would be scared and my dreams would frighten me.
I’ve taken medications to muffle the anxiety of the chemo treatments I knew were about to come.
I’ve been terrified and wondered how I was going to get through it.
I’ve faked it and smiled and been the portrait of strength and composure while ready to crap in my pants because I was so scared inside.
I’ve felt the chemo needle go in my arm bringing the drugs in, felt the cold liquid hit my blood and wanted to scream “Wait! I’ve changed my mind! I think it was a mistake! I think it wasn’t me! I think you got it wrong!”
I felt the pre-medication go through me, hit my brain, cross the blood-brain barrier and fog me up.
Pausing, knowing it’s in me.
Thinking
Please.
Please.
Do your work.
Save me.
Drugs, do your work and save me.
How will I know if they did? I won’t.
I don’t say I’m cancer-free. I have no idea if I am.
I will hopefully die of something else and I will have my come-uppance. I will give cancer The Finger.
I will have it say on my tombstone:
Hey, Cancer: I laughed last. I died of something else.
So, call me a crybaby.
I prefer to say I experience the world richly.
Either way, I make no apologies for my tears.
That’s the kind of girl I am.
May 3rd, 2011 §
There isn’t one right way to react to loss. And the thing about grief? It’ll sneak up on you precisely when you’re not looking.
This morning I attended a memorial service for a 38 year-old mother of two. She died of complications from leukemia, leaving a loving husband and two children behind. We were connected by a shared friend and a diagnosis of cancer.
When Kellie was diagnosed fifteen months ago and learned she needed to have chemotherapy I offered her my scarves. I had an extensive collection from my months spent without hair and had been serially loaning them out to friends after my hair grew back. After they’d covered my head, they’d gone to a friend’s sister in Colorado who had breast cancer. Then they went to a friend down the street who also had breast cancer. The fourth head they touched was Kellie’s.
During that time I had to deny others the use of the collection. I know too many women who’ve had cancer, I thought. There isn’t a break in between their tours of duty. The scarves don’t rest, they just keep traveling.
Perhaps some might find it icky to wear a scarf of someone else’s. That never seemed an issue for my friends. In fact, their softness from being washed so often was a bonus; heads are sensitive when hair comes out and the softer the cotton is, the better.
Kellie had those scarves for a long time. Her own fiery red hair was long gone; my scarves were a poor substitute for that ginger hair of hers. I like the thought of her having something comforting and cheery to cover her head during some of those difficult days though.
After the service today the guests stood talking over coffee and tea and far too many sandwiches and baked goods. Unprompted, our mutual friend assured me the scarves were safe and would be returned soon. I know when the stack comes back I’ll touch the scarves longingly, wishing Kellie were delivering them herself.
I’m overwhelmed today with emotions… sadness at the second Mother’s Day without my beloved mother-in-law, anger at cancer for claiming another young mother, frustration that oncology is often an art more than a science, worry that it will happen to me.
I just need to think. I just need to cry. I just need to remember. I just need to live.
May 1st, 2011 §
In the weeks before my surgery, I looked at pictures of double mastectomy patients on the Internet. I Googled “bilateral mastectomy images before and after” thinking I was doing research. I thought I was preparing myself for what was coming.
In reality I was trying to scare myself. I wanted to see if I could handle the worst; if I could, I would be ready. My reaction to those images would be my litmus test.
Some of the pictures were horrific. I sat transfixed. I looked. I sobbed. I saw scarred, bizarre, transformed bodies and couldn’t believe that was going to be my body.
Days later, when I met my surgeon for my pre-op appointment he said, “From now on, don’t look at pictures on the Internet. If you want to see before and after pictures, ask me– look at ones in my office. You can’t look at random pictures and think that’s necessarily what you are going to look like.”
All I could do was duck my head in an admission of guilt. How did he know what I’d done? I realized how he knew: other women must do this. Other women must have made this mistake.
The aftermath is terrible to me though not in the ways I’d anticipated. I have no sensation in most of my chest. I never will.
A major erogenous zone has been completely taken away from me. Yes, I have new nipples constructed, but they have no feeling in them; they are completely cosmetic. The entire reconstruction looks great but I can’t feel any of it. It does help me psychologically beyond measure to have had these procedures though.
Here I sit, two gel-filled silicone shells inside my body simulating the biologically feminine body parts I should have. And sometimes that thought is disturbing.
To be clear: I don’t regret having them put in. I’ve never regretted that. It was a decision I made, and made deliberately. I knew that reconstructing my breasts was the right decision for me. I’m getting used to them– I’m almost there.
I definitely don’t remember what my breasts looked like before. I only remember these.
I once asked my plastic surgeon to see my “before” pictures a year or two after my reconstruction was over. You know what? My “before” breasts didn’t look so great. In my mind they did.
In my mind, everything about my life before cancer was better.
But that’s not the truth.
My mind distorts the memory of my body before cancer. Then forgets it.
My mind distorts the memory of my life before cancer. Then forgets it.
With time, I can get used to a new self.
It’s like catching my reflection in the mirror: only lately do I recognize the person staring back at me.
For over a year the new hair threw me. It’s darker than I remember it being before it fell out. It’s shorter than it was before, too.
And the look in my eyes? That’s different also.
I just don’t recognize myself some days.
Sounds like a cliché if you haven’t lived it.
But it’s true.
April 15, 2009
April 30th, 2011 §
What does it mean to “be an inspiration”? A few people have said that to me recently: I am an inspiration. At first I laugh. I guess I’m an inspiration because I’m still alive. Maybe that’s enough.
What’s inspirational about me? Trust me, I’m not searching for platitudes here. I’m trying to get at “what makes someone an inspiration” and why do people think I and so many other breast cancer survivors qualify? There’s definitely more than one day’s blog in this question.
Is it being a mother and worrying about your children more than yourself? No. That’s what every mother does.
Is it summoning strength to confront chemo when it’s your greatest fear?
Is it putting a smile on your face when you are crumbling inside?
Is it speaking the words, “I have cancer” to your children, your friends, your husband, your parents, your in-laws, your brother, and all of the people in your life enough times that eventually it starts to sound normal?
Is “inspirational” when you offer to show your post-mastectomy body to women so that they will know the results just aren’t as scary as they are thinking they will be?
Is it answering everything and anything people want to know?
Is it putting words and feelings in black on white?
The essence of inspiration is being strong.
When you least want to be.
When you are faking it.
Strength.
When you lack it.
When you have to dig deep for it.
When your kids need dinner and you want to vomit from the chemo.
When you are too weak to climb the stairs.
And you don’t think you can get through another day.
Or hour.
Or minute.
Or second.
And you just want the pain to end.
Somehow.
Some way.
Any way.
Just have it go away.
When your pride is gone.
Dignity is gone.
All of it.
Being inspirational means being tough.
It means feeling rotten but not wanting others to.
It means wanting to put others at ease with how you are doing.
It means being a lightning rod for everything bad.
A catalyst for everything good.
A spark.
A resource.
A friend.
A wife.
A lover.
A mother.
A daughter.
It means telling your parents you feel okay when you don’t.
A little fib so they will go home and get some rest for the week.
Take some time off for themselves before they come back in 8 days and do it all over again.
A break so they don’t have to see their little girl suffer anymore
Because 6 days in a row is enough.
For anyone.
Because looking good makes others feel better about how you are doing.
So you put makeup on.
And dress well.
And put a big smile on your face.
So they will think you are feeling good.
And when you switch the topic of conversation, they will go along with it–
They will believe you when you say you are feeling better.
Okay, so maybe I am inspirational. I don’t call it inspirational. I can only admit to the smaller things. The micro things. Inspirational sounds big. Important. It’s hard to accept that one.
But I think I’m convinced.
The reason I’m going to finally concede is that I just realized something:
That was my goal.
Except I wasn’t calling it that.
I was just calling it doing it right.
I was calling it setting an example.
I was trying to show my family, especially my daughter, how you can tackle an obstacle– a big one.
I was just doing my job.
June 15, 2009




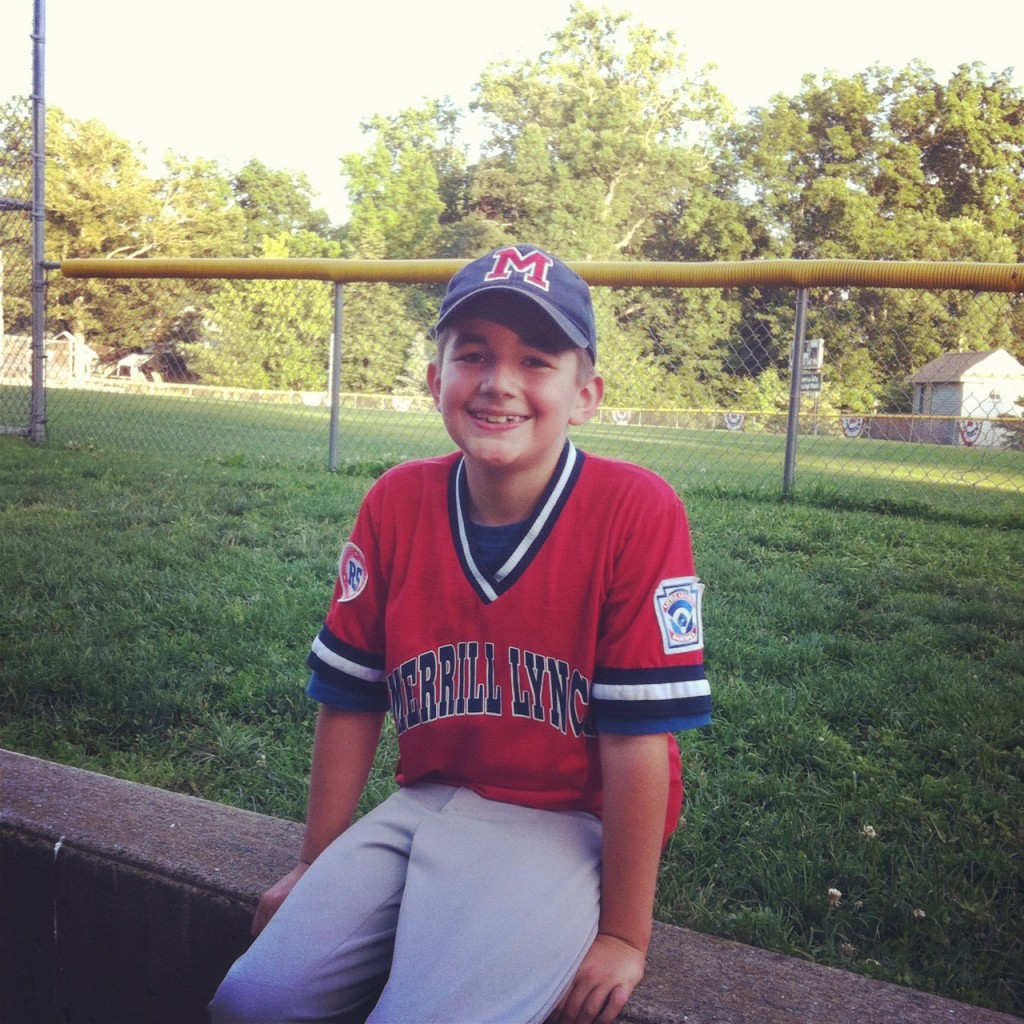










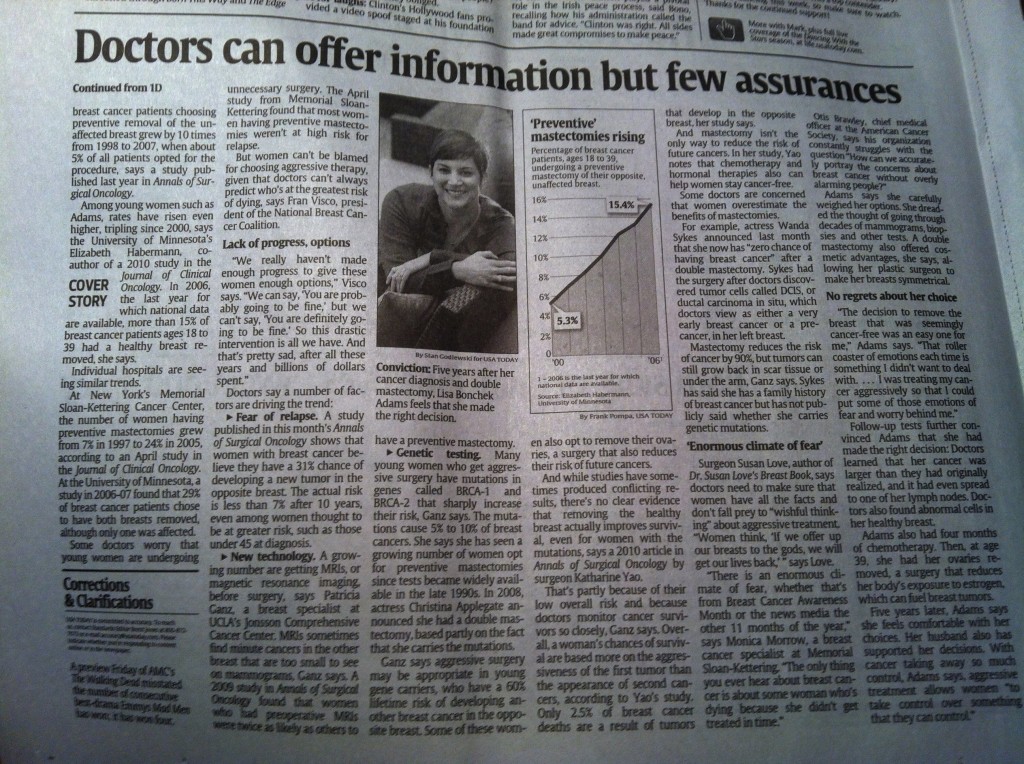


 Link to Twitter
Link to Twitter