October 8th, 2014 §
 It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.
It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.
It does not matter if any of those things are true, your cancer can be worsening.
As I have described here before, metastatic breast cancer is characterized by resistance to therapies. If a treatment works in the first place (and according to my oncologist, most have about a 30% chance of initial success), the cancer will almost certainly become resistant to it and it will cease working. This resistance will happen time after time. This has happened numerous times to me already. I have had some treatments not work at all (Taxol, Fulvestrant+clinical trial drug GDC-0032) while others worked for a few months and then would not work any longer (Xeloda, Aromasin+Afinitor) .
Once again, this resistance has happened. Carboplatin and Gemzar did their work starting in March and did it well, bringing me back from a very dark place this Spring. After 9 complete cycles, though, they are no longer working. It is time to move on.
Moving on is scary. It means being in freefall as we use educated guesswork to decide what agent(s) to try next.
The good news is that I was officially approved to receive palbociclib from Pfizer under their expanded access (compassionate use) program. I will be able to get this drug before it receives final approval by the FDA and therefore before it is on the market sometime in the next year. There is no guarantee this drug will work (alone or in combination with other drugs that are on the market already). It is just one more thing to try.
There are still final bureaucratic hoops to jump through, though, and I won’t have it for at least a few more weeks. This presents a problem: I need a new therapy now. I cannot safely be without treatment for that period of time. It also is best for me to be in a state of control when I start it; the higher a cancer load I carry the harder it would be if what the drug does is provide stability rather than cancer regression. Stability is considered success in metastatic breast cancer drugs. Just keeping things the same, preventing cancer progression, is good. This is considered “success” in using a drug for metastatic breast cancer. However, if you start at a very high cancer load, that stability may be quite intolerable. My oncologist and I feel it is best to have that load brought down (not just held steady), and we don’t know if this drug is a workhorse like that. We can’t count on it to be.
I’ve known for the last week that things were probably over for this chemo. We had tried a higher dose of both drugs already without success. I adjusted to the news over the weekend and yesterday I started on a new chemotherapy regimen. Navelbine is given through my port as an IV “push”; it’s just one syringeful that is given in about 30 seconds. Having a port is really helpful for this one because it is very irritating to veins if you do not have a medi-port implanted in your chest like I do (the port is completely under my skin, it is a lump about the size of a nickel and is accessed with a special needle by the nurses. They can take blood from it, give medication and chemo through it the way you would with an IV except you don’t have to use an arm vein). We are initially planning on a schedule of two weeks on, one week off, but that may change as we go. And of course, if it isn’t working, we’ll have to try something else.
I’m having some other problems now that the cancer is growing so that has been a challenge. Side effects don’t just stop the minute you stop taking a drug. And moving right on to another one means there is no break. It is what is needed though. The good thing is that if you find something that works (like the Carboplatin and Gemzar did for me), they can do astounding things to kill the growing cancer and bring it back under control.
Metastatic breast cancer is like Whack-a-Mole: cancer pops up in places and then can often be whacked back down. If you’re lucky you can play this game for a little while as it takes up residence in different bones and organs. We’ll see how successful we are this time. This is always the hardest time for me mentally: living with the uncertainty of trying to find a new regimen, trying to find something that works, knowing right now there is nothing.
But this is the choice I have made in choosing to treat my cancer. That is the nature of this disease. These are not heroic measures. This is what treating metastatic breast cancer is.
And so we go… onward.
September 12th, 2014 §
 Hi everyone, a quick update before the weekend…
Hi everyone, a quick update before the weekend…
It’s been a really tough few days after the increased dose of Carboplatin with my Gemzar infusion. Every side effect has come out of the woodwork and I’m doing my best to sleep off as much as I can while still doing the necessary daily activities. I went to one Back to School night this week and hope to attend two more soon. Next week will be chemo again (Gemzar only) and then a transfusion a few days later. I’ll also get a Neulasta shot next week and my usual Xgeva shot as well. That will be a rough week.
It’s too soon to know if the higher dose of chemo is doing anything at this point, so I am just forging ahead. We should know more in the next few weeks. Until then we continue to think about what option makes the most sense to try next.
Terry Teachout featured me in a touching piece he wrote in The Wall Street Journal yesterday called “Mortality and Muse” about those of us who choose to write about unpleasant subjects. He honored me in his support and I wanted to share it with you. To read it click here.
Here, too, is a link to the YouTube video from a panel session at Stanford MedX this month entitled “Communicating the Experience of Illness in the Digital Age.” Towards the end (around 30 minutes in) they directly address my story but anyone who wants to hear more about the topic can watch the panel session. Thank you to Susannah Fox, Colleen Young, and Meredith Gould for addressing some of the real issues and challenges of individuals who choose to share their health stories online.
Autumn is in the air here and I hope wherever you are you are able to find a bit of beauty for the weekend. I will be doing just that.
September 8th, 2014 §
 I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
First let me report the good things. I have had some great days after my transfusion last week for severe anemia (expected often now after this much chemo).
On Friday night I drove Colin in heavy traffic to his first travel baseball game (took two hours). Then I sat watching warmup and the game which was another 3.5 hours. Then an hour home. I am detailing that time to brag. Look what I did with my son.
It wasn’t physically easy for me. But it was joyous. We got so punchy in the traffic jam that we were waving our hands in the air “seat dancing” to the music. We nicknamed a car “Duck Dynasty” that was broken down by the side of the road and then got lost at the venue and ended up 4-wheeling over gravel hills. We had a blast. Here is my precious middle child when we arrived at the field. The team won which was exciting. It was his first game on a full-sized field and also under the lights. I also got to take him  to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
The medical update since the last post is that in short, there isn’t a good clinical trial that I qualify for/am willing to enroll in right now. The chemo regimen that I am on makes me ineligible for some because it affects my blood counts so severely each time now (quite a catch-22, I would need to go off chemo to even have a chance at being considered). One trial I can’t be considered for because there isn’t enough tissue left from a previous biopsy to use it for required testing. Because my cancer is primarily in bones or other places inaccessible by surgery, this is not an easy problem to fix.
Now I’m going to get a bit technical. I’m hoping to explain a bit about how the different clinical trial types work since many people don’t know these distinctions. Consider this your breast cancer education for the week! Yeah, you know I’m not a doctor so I’m explaining this to the best of my ability. Ask a doctor for more info, especially one who works in clinical trials to be sure the trials you or a loved one might be considering work the same way.
Here we go:
One type of Phase I clinical trial (which I would qualify for) is risky enough that this option isn’t reasonable to me right now. Let me clearly state that they may become very reasonable options at some point soon and I totally understand why other people choose to do them! These particular phase 1 trials I’m opting out of for the time being are the kind that are testing safety of a medication previously untested in humans. That is, they don’t yet even have a dose that they know is safe. They are called “dose escalation Phase I trials” which means they start with a low dose they think is safe and gradually increase the dose until the side effects become too bad and the test subjects can’t continue and they stop participating. They do these on a small number of people.
This process establishes the maximum tolerable dose and the company hopes to then proceed to a Phase II trial. That Phase II trial tests if that established maximum tolerable dose even does anything measurable (Phase II trials test for efficacy: is this drug keeping the cancer stable or even causing it to shrink?).
To complete the clinical trial trio, a Phase III trial tests the “current standard of care” plus the trial drug against the current standard of care alone. That is, does adding this drug to a treatment that is a normal one for this cancer improve outcomes above and beyond just giving the treatment the patient would normally get (are results better? The same? Worse?). For ethical reasons there are no placebos used alone instead of treatment in Phase III trials in metastatic breast cancer. They would be used only to combine with the standard of care treatment. No patient goes untreated. All get the usual treatment as the guarantee.
This process means that during the Phase I dose escalation trial I first mentioned 1) you don’t know if the trial drug is safe, 2) you don’t know if that dose is too low for some or all of that time to even be doing anything, even if it is eventually going to be efficacious, and/or 3) if it even works at any dose (without making things worse). This means continuing with your cancer potentially untreated for months, an often dangerous proposition in metastatic cancer.
I don’t want to go into more details of those trials but I do think it’s important for me to continue to explain the way that some clinical trials work with metastatic breast cancer.
As I think I mentioned in my last post, the likely immediate plan was to increase the dose of one or both of my current chemo drugs. Because I opted not to pursue enrolling in a clinical trial I will remain on IV chemo. If I had chosen the trial I would need an additional two weeks without any chemotherapy to complete the mandatory washout period where I do not use any medications to treat the cancer because their presence in my body could affect the trial drug results or side effects.
I am going in for an increased dose of Carboplatin and steady dose of Gemzar on Tuesday. I did have one increase already in the Spring on my Gemzar dose. We will see what kind of response we can get from this Carboplatin increase, if any. It will hopefully buy us some time until some other trials open up and/or we can consider if we can do a biopsy once we see a current CT scan.
A few readers were concerned that I was relying too heavily on tumor markers in my decision-making. In short, I’m not. I am well aware (as I’ve said in almost every post except last time) that markers, particularly CA 15-3, are not reliable for many people. This is why this test is not used as a screening test for people to find out if they have breast cancer. If it were valid they would use it instead of or in conjunction with routine mammograms.
I know many doctors don’t use blood tests for markers at all and for some types of breast cancer they are totally worthless. Trust me, oncologists at Sloan-Kettering are well aware of all of this information as am I. The most important piece of information is a history of them in me and how they correlate with scans and my disease progression. I am one of the people for whom they are tightly and reliably correlated with my disease. We have had seven years of studying them in my particular case and two years with close monitoring during metastatic disease. So while I definitely appreciate the concern, you can rest assured that we make decisions with all of this in mind. It was my error in not putting that usual caveat in that last post.
So… for now the plan is: higher dose of one of two chemo agents on Tuesday. Test markers to see what they’ve done in last few weeks.
In case you are curious, going for chemo doesn’t just mean getting two drugs. The infusions I will get on Tuesday are numerous. I will get the following 8 infusions in this order: Decadron (helps with nausea and mainly to help prevent an anaphylactic reaction to Carboplatin because I’ve had more than 6 infusions), Pepcid (helps with anaphylaxis prevention and also bonus heartburn help), Benadryl (helps prevent anaphylaxis), Carboplatin (chemo agent #1), 1 liter fluids (helps prevent dehydration and bonus helps to keep kidneys functioning well to avoid high creatinine levels that can be dangerous), Aloxi (anti-nausea, blocks signals from stomach), Gemcitabine (chemo agent #2), Emend (blocks nausea and vomiting signals from the brain).
Away I go… thanks for the support. These days of uncertainty are difficult for me. I like a plan.We have a short term one and I am, as always, moving forward. As I wrote in a prior post and re-read tonight:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
August 28th, 2014 §
 The last week has been stressful. Unfortunately, my bloodwork shows that the chemotherapy regimen of Carboplatin and Gemzar is losing its effectiveness. It’s time to start looking at options for what to do next.
The last week has been stressful. Unfortunately, my bloodwork shows that the chemotherapy regimen of Carboplatin and Gemzar is losing its effectiveness. It’s time to start looking at options for what to do next.
We watch my tumor markers very closely and check them each chemo cycle (every three weeks). Once there is evidence of an increase in the marker number, my oncologist and I start to construct “if/then” decision trees. I know from earlier this year how fast metastatic breast cancer can spiral out of control. I don’t want to have that happen again if I can avoid it.
There is no guarantee that any given treatment will work. Many chemotherapies won’t work at all. One that works in 50% of cases is considered a great option. If they do work, they won’t keep working. The cancer will mutate, become resistant. We seem to be there again.
There are options to consider: clinical trials, chemotherapy, targeted therapies. Clinical trials are becoming harder for me to qualify for because I have already received too many different chemotherapy drugs. Most of the trials for metastatic breast cancer patients limit the number of chemotherapy agents to two. I’ve already had Xeloda, Taxol, Carbo and Gemzar. I simply can’t be considered for most of these trials.
At this point we are exploring a few options and using the next few weeks to investigate what trials are currently open and enrolling patients (they often take batches of new patients in clusters). The main issue, however, is if they are trials I actually am interested in. I need to look at the science behind each one and try to balance the risk of trying it versus other treatment options. Enrolling in a trial means having a “washout period” with the patient receiving no treatment at all (usually 3-4 weeks) before starting the protocol. This can be a precarious position to put yourself in if you have already been on a treatment that has become ineffective.
So where are things for the immediate future? For now our plan is to go through one more round of this chemo combination but do it at a higher dose and see if we can get either a response or stability at least. That will buy us a few weeks to gather information on what trials are available and what we want to do.
As far as my update for the week, I had chemo on Tuesday and I needed another shot of Neulasta yesterday to boost my white count and thereby restore my infection-fighting capability. The chemo now knocks that down every time and I can’t recover on my own. Once again I will need a transfusion of red blood cells tomorrow because my hemoglobin level is too low. When this happens I don’t have enough oxygen-carrying capability in my blood to allow me to function normally. I get short of breath just walking or standing. This is a predictable part of some types of chemotherapy if you are on them long enough. After enough cycles of constant chemo the body just can’t compensate for what is killed in the collateral damage of treatment. Not all chemos do this, but mine does.
So the news is not what we want. It’s hard to hear. This chemo combination did a great job at shrinking many lesions in a short time. I am functioning in a much better place than I was this Spring, but now I worry that things will progress quickly before we find something new that works. I wonder what will work. I wonder how long it will take to find it, and what kind of shape I will be in when we do. If we do. At this point there are enough options that I do still think it’s when, not if. But this day has come sooner than I’d hoped.
June 12th, 2014 §
 You have all been so patient with me, understanding why I haven’t been able to update as often as I was doing previously. I’m hoping my report will be worth the wait.
You have all been so patient with me, understanding why I haven’t been able to update as often as I was doing previously. I’m hoping my report will be worth the wait.
Let’s cut to the chase with some good news: there is no doubt about it, I am on my 5th cycle of Carboplatin and Gemzar and these chemo agents are effectively reducing the overall amount of cancer in my body (my recent previous chemos were not).
So, the cautionary notes are that the chemo will eventually fail; the cancer will either become resistant or I will lose tolerance for it because of side effects or hypersensitivity as the doses go on and the cumulative totals of the drug I’ve been exposed to rise over time. This is a problem that happens with only some chemo drugs; Carboplatin happens to be one. As you may remember, I am trying to ride carbo’s work as long as I can, it’s not for a finite number of sessions. With metastatic breast cancer you must be on some form of chemo/targeted therapy for the rest of your life if you choose to treat it. So this isn’t a permanent fix.
Additionally, I am right on the cusp (my next cycle) of when I will be most at risk for reactions to the Carboplatin. The other drug, Gemzar, is easier to tolerate in general and doesn’t have this same hypersensitivity issue. Of course we don’t know for sure which chemo is doing the bulk of the work here. Ideally we keep them both.
My tumor markers have all consistently been dropping for last 6 weeks and in my particular case, these markers have always been closely correlated with what scans and clinical signs show (many with breast cancer do not have this correlation, you must know your own case; this is one reason why these blood tests cannot be used as tools to screen for breast cancer or metastases reliably).
What does it mean that my markers are dropping? The numbers are going down significantly, indicating that the chemo is working, something I anticipated because I have been feeling much better in last month. “Better” is relative of course. What is “good” or even “great” for me might be someone healthy saying it was one of their worst days I bet! But what is important is that it’s moving in the right direction. My issues now are more chemo-related (fatigue, weakness, blood counts, infections, shortness of breath, etc.) than cancer-related.
My voice has improved! There is no doubt. I am still raspy and if I talk for a while or have to strain to use it, it deteriorates rapidly. But it is such a change. I can swallow more easily which makes getting needed fluid and swallowing pills easier. I no longer need to go for added IV hydration, I am able now to do it in conjunction with chemo.
 I can get out more for limited times on certain days. Some days this is impossible because of chemo. And I institute a “no hugging” policy for friends during times I know I’m especially susceptible to infection. I’ve made it to the beach a few times, to more special events for the kids, and for the first time this week could stand long enough to fold some laundry. I am still very weak and incapacitated on many days. But now my “off week” from chemo is better.
I can get out more for limited times on certain days. Some days this is impossible because of chemo. And I institute a “no hugging” policy for friends during times I know I’m especially susceptible to infection. I’ve made it to the beach a few times, to more special events for the kids, and for the first time this week could stand long enough to fold some laundry. I am still very weak and incapacitated on many days. But now my “off week” from chemo is better.
Just because people see me in public they shouldn’t assume that I’m “back to normal” or “feeling great.” It is hard to explain that it might have taken me all day to get the energy up to do that one errand or have that one coffee date with a friend, that I’ll need a nap and to rest for the rest of the day after doing it. They might not understand that I was in bed for days leading up to it or will get chemo the next day and not be well for a while. I still have metastatic breast cancer throughout my body, and it takes a hefty toll. Hopefully explaining some of these details can help people to understand a bit what daily life is like for me.
I’m enjoying my garden in bloom and have been taking photos and posting this month on Twitter/Instagram. I’ll be using them with my posts all summer. Every one is taken by me of something in my yard. Today’s are of my beloved Japanese peony, a single petal peony I planted from barefoot years ago. This year it only had three flowers but they were so gorgeous. It’s hard to believe the closeup is of a flower! I think it looks like a sea anemone (some have said it looks like french fries).
So, the takeaway: I’m moving in the right direction for now, for what my particular case of metastatic breast cancer is. Despite many headlines about advances in breast cancer treatments lately, there was NOTHING relevant to me coming out of the big national ASCO conference last month and a good source tells me there really won’t be anything coming out of the San Antonio breast conference for me, either (the few relevant trials just haven’t been going on long enough to have any preliminary results yet). I’m keeping on top of new trials, as is my team, and if there is something that comes up that looks good, we’ll be investigating. For now, for as long as I can, I stay the course on this chemo regimen whether it’s for one month more or eight.
I will try to write more often. I know it’s a bit concerning when long times go by and someone with a serious illness doesn’t post. That only goes to show you how utterly rotten I have felt for a very long time. It has taken seven months (seven months!) to get to this point. I don’t take that for granted. Some with my diagnosis are dead within that time.
It’s so nice to be able to report some good news. It sure does feel like an awfully long time since I’ve been able to do that.
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
January 10th, 2014 §
 The car has always been a place of refuge for me.
The car has always been a place of refuge for me.
The shower, too.
Water to rejuvenate
Clearing away the old,
Ready for a new day ahead.
The moment of awakening is significant.
I have learned quickly what the next few hours will be.
I try to give a nurse a complete report but I encounter one problem immediately.
I really cannot type accurately.
My body shakes, my hips cry out in bony futile gasps. I gather up my pump cords, release myself from the wall’s grip.
I walk, counter-clockwise around the nurse’s station with a vengeance, trying to push the pain and discomfort away.
……………………………………..
I am Angry at this morning and that which has me here.
The tears arrive.
The radiation pain seems to be on the way in.
How long with it last? Does that mean it’s working? I and everyone else ask.
“I don’t know” is the way to do it. I say it aloud to the dark, embarrassed after the first word that I realize I am alone in the room.
I hear my voice, speaking to someone not present.
I can’t help but cry as I push the pole.
The movement makes it better. It reminds me of being carefree on a summer day, wind in my hair from the sunroof, feeling the sun on my face.
I think of my friends readying their homes for the day before work and school.
I can feel the radiation, where it burns, or at least the spots where tumors are trying to escape their home,
where they try to find new lands to conquer in a cat and mouse inside my body.
It doesn’t matter what stinking metaphor you use for it; in this case, all roads lead to Hell.
I contemplate eyeliner while the nurse stands, patiently waiting to see how I’ve done overnight.
…. But there is no one there.
I focus very hard on the tasks at hand: morning medicine most especially.
I start to tell my nurse that I weighed myself already today. Or yesterday. Or two days ago. But I can’t remember now. And so I remain mum.
In each moment my mind leaves. I don’t know where it goes. But in those gaps which feel like seconds, minutes have gone by.
The tea is divine, hot silky relief from the cold my body cannot push out.
I realize whatever it is I thought I could accomplish at the keyboard won’t happen once again.
I can’t concentrate. I find gibberish on the page. It takes hours to do a few moment’s work.
Extra time lost.
Time lost.
My precious time.
I stay committed to sitting up, bedside, fighting the urge to recline.
I listen to music trying to keep myself alert.
I think about my children, wondering what each is doing…
I realize today I am too foggy from medication.
I won’t be able to do much for a while. I am too busy talking to people that are not there.
I will rest, let the pain calm, let my head settle.
January 6th, 2014 §
 The last weeks have not gone as planned.
The last weeks have not gone as planned.
I had the liver biopsy and PleurX drain put in my left lung on 12/31/2013. I was going to only stay one night for observation and to try to address the pain that I was having. Further tests revealed more information. The pain that we thought was coming from my lung and spine wasn’t just coming from my lung and spine. In fact I have some tumors in my bones in the left hemisacrum and right femur too. The spine tumors are now in more vertebrae than we’d thought.
I’ve actually been in the hospital for 6 days now trying to get the pain under control and formulating a treatment plan with my team. I will need to be here for a while longer. I am starting 10 sessions of radiation later tonight after being mapped this morning. We had hoped to do it in five sessions but for reasons I can’t go into now they have decided this is a better route and will be more effective for the future.
This treatment will stop the current progression of pain, but the way this radiation works for me is that it won’t provide true pain resolution for probably about 2 weeks and then improve further over the next few months. The pain reduction will be cumulative and take a while (long after the radiation is actually over) to see final resolution in my case. I’ll have to deal with this for a while yet.
The side effects because of where they are targeting the beams in my spine will be irritated esophagus, trouble swallowing, nausea, vomiting, and heartburn. The other radiation site in my hips will potentially cause decreased blood counts, pain, irritation, gastrointestinal pain and dysfunction and the like.
My pain is still not under control and I’m on a Fentanyl pump system that allows me to dispense medication as needed in accordance with the pain levels. I will convert over to oral medication and patches when it’s time for me to go home once we can figure out my needs. The pain and palliative care team here is unbelievably caring and devoted. So are the physicians and nurses. I have created an expanded family here already and can’t say enough nice things about the quality of care and total commitment to the patient.
I think for now that’s enough news.
Please, please respect my declaration that I do not want uninvited visitors, any gifts, or any flowers sent during this time. I know the intent might be good, but I appreciate so much those who have opted to instead donate to my Sloan Kettering metastatic research fund instead of purchasing anything for me. I haven’t been able to send thank you emails for those recent donations but trust me, they are appreciated. Good thoughts are also always just fine and have the right price tag!
This is a time when I am dealing with severe pain, a medical diagnosis that is unfolding and serious, and needing rest as much as possible. I do read emails but I am not responding to most at this time.
I was not able to start the clinical trial because of these newest announcements. We will see if I am eligible for it again in the future but for now we have to get the disease and pain under control. I did go on chemo for a few days but it now needs to be stopped during radiation. I will resume chemo after radiation is over and about a week of recovery time has elapsed.
Things change hour by hour, day by day. I’m adjusting the best I can. I hope this will at least let you know where we are, a long way from where I thought I’d be in the first days of this new year. Welcome to the world of metastatic breast cancer.
December 31st, 2013 §
I’ll be heading out soon to the hospital for two procedures. The first, a liver biopsy, will take samples of the small metastases to my liver for testing to get information about the cancer to help guide us in choosing targeted treatments. Features of cancer like hormone receptor status (ER, PR) and HER2 status can change over time and be varied in metastases in different parts of your body. It is important to repeat biopsies as time goes on to make sure you are still using the best drugs to treat your cancer.
The second procedure today is the implantation of a PleurX catheter. This will allow fluid to be removed from the lining of my left lung which has cancer in it. The fluid keeps accumulating so until we can get that reduced I will have to use this drain system at home to remove fluid daily. Keeping that level down will allow me to breathe well. This is a quite a process and I didn’t realize all that was involved. I’ll explain more about this in another post. This link shows how it works for anyone interested.
The main info I want to briefly share is that we now know more about where the excruciating pain I’ve been having is coming from. The PET showed that the cancer in my T12 vertebrae has grown and is encroaching on the space in my spinal canal. I also have an active spot of cancer that’s intense in my left hip. The spine, however, is where we are focusing the attention.
For now, we need to do more tests while I am in the hospital, but the immediate goal is to get radiation to my back and, if needed, to my pelvis. There is a lot to do to get all of that set but we are aiming to get radiation started by the end of the week. I do not know yet anything about what the protocol would be in terms of how many sessions but I do know that it will bring a lot of relief of pain once I can have that done. Until then it’s all about pain management.
I will also meet with a palliative care team while in the hospital to get the best assistance with the pain since it will be a while until I get relief at the source. Palliative care doctors are experts in pain management during all phases of cancer treatment, not just end of life. Palliative care teams help with side effects from the cancer and the treatments and are wonderful resources.
That’s all I have time to share for now but it looks like I still have a bit longer to wait for relief. Obviously this wasn’t news I wanted and I’m still adjusting to it. Once again, this latest development shows it doesn’t matter how you look on the outside; you can “look good” and still have cancer treatments that are not working, cancer that is progressing. This is an important message to repeat.
Right now we are still gathering information to decide whether I will participate in the clinical trial I was set to begin this week.
I hope you all have a safe New Year’s Eve and I’ll try to report back as soon as I can. Thank you for all of the support. It seems like a good time to once again share the link to my research fund donation page at Sloan Kettering in case anyone has those last minute end of year contributions to make!
December 29th, 2013 §
 No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
Everyone kept telling me how great I would feel after the thoracentesis. I did feel like I was breathing easier, but I didn’t feel great. In fact, I had quite a bit of pain. They checked for an air leak by x-ray as they always do after this procedure. There were no visible complications. But there was still tremendous pain starting that day and increasing into the next. It was more than the pain from the reinflation of a lung that had been compressed by half its size. But exactly what it was we weren’t sure.
By Thursday when I had to go back to Sloan-Kettering for my PET scan, echocardiogram, and EKG I was in agony. One of the doctors I met with could see how much pain I was in and prescribed some narcotics. I can’t take anti-inflammatories because I am having a liver biopsy next week and they put patients at risk for bleeding. I am so grateful a doctor seeing me about paperwork reached out to offer assistance and relief.
My father met me in the city. After I completed the required tests he drove me home. I can’t think of anyone better qualified to keep an eye on me than a retired cardiothoracic surgeon. Unfortunately, the pain continued. In all likelihood it is a combination of the cancer causing inflammation in the pleura and some nerve inflammation now that some of that fluid is gone and the lung is reinflated. It’s really all conjecture. We will see if the scans and tests reveal any additional information.
Oxycodone couldn’t keep the pain under control so yesterday I had to combine it with a Fentanyl patch. This duo is definitely helping me more; I’m still in pain but it’s more manageable today (Sunday). Each of these patches lasts for 72 hours and will deliver a constant stream of medication to me. I am pretty much bedridden.
It’s looking like Tuesday (New Year’s Eve) will unfortunately be a tough day. I was already scheduled to have a liver biopsy (This is not to check for malignancies; we already know there are metastases here. This procedure will be for repeated genomic sequencing analysis and other testing to make the best choices about chemotherapy and future clinical trials). Now, given all of the events this week, the team has decided that I need to have a PleurX catheter put in. This is a drainage system that will allow me to remove excess pleural fluid at home rather than having to have it tapped with a needle each time it builds up. The catheter will stay in place only as long as I need it, which will be as soon as treatment starts working and the fluid stops being produced in such copious amounts. I assume this will be at least a few weeks.
Having these two procedures and pain control issues means I will need to stay overnight in the hospital for observation. It’s amazing the lengths some people will go to to be in NYC for New Year’s Eve fireworks, isn’t it? Maybe Anderson Cooper will swing by while I’m recovering.
Once we see the results of all of the tests I’ve had and have these two procedures behind me, we will re-assess the plan to start the second clinical trial on Thursday. The most important immediate tasks at this point are to treat the two symptoms and get my breathing and pain under control. Immediately after that we go to work on the metastases to stop the problems at their source.
Thank you for all of the support I’ve had over the last few days including local friends who have been so kind and some friends who came from quite a distance to keep me company this weekend. I’m just putting one foot in front of the other and doing everything I can to gather all of the information I need to make a decision about what the best next step is.
Of course, as much as I can, I’ll keep you posted. Twitter is always the best way to keep up to date on daily happenings. It’s a lot easier for me to get quick bursts of info out in that medium. So many have asked: I have all of the help that I need and respectfully ask for no visitors or gifts during this time.
I would like to wish you all a happy and healthy 2014 if I don’t post again here before we all ring it in.
December 23rd, 2013 §
 For three days I’ve been mostly bedridden. During two days of sixty degree weather I didn’t make it out of the front door. What I believe is a virus sidelined me for the weekend and today (Monday) I’m still trying to get strength back. Thankfully I think it’s my immune system making me the target; no one else in the family has gotten it.
For three days I’ve been mostly bedridden. During two days of sixty degree weather I didn’t make it out of the front door. What I believe is a virus sidelined me for the weekend and today (Monday) I’m still trying to get strength back. Thankfully I think it’s my immune system making me the target; no one else in the family has gotten it.
Tomorrow I will go back to Sloan-Kettering for another attempt at a thoracentesis. I have had many people ask more about the process and what it is. This was a very good summary with a graphic. It kind of gives me the willies (does anyone even say “willies” anymore?) to look at that.
When even television seems too much,
And hours go by staring out the window.
I listen to the sounds of my children playing,
I hear life go on without me.
It was a day like this that I wrote the lyrics to the song “Six Minutes,”
A day I wished for the time to go. Just go by faster.
But as on that day,
Today I am aware that these are the days I’m fighting for.
If I didn’t want them I wouldn’t be doing all of this.
I know that this is a tough day. Tomorrow will be one, too.
But I also know that someday, hopefully long from now, it will count as a good day, a great day.
And that realization scares me too.
I spoke with a patient care representative at Sloan about some of the mistakes that were made on Friday. I told her my story and we talked about some ways she could follow up. I told her I wasn’t angry, I know mistakes happen, but I thought there were ways to try to make sure these things didn’t happen again. At the end she gave me her contact information. I said, “I love my doctors and the care I get. But there are always ways to improve. I appreciate the chance to give those suggestions to someone who can do something about them.”
Then I started laughing. “You know, I hope to be calling you with suggestions for many years to come. That will mean I’m still here, trying to help patients get better care and trying to help doctors and nurses provide it.” She started laughing too. “You know, I really like that perspective. I’m not sure I’ve ever heard it put that way. I like thinking about more suggestions as meaning more time.” We thanked each other and hung up.
And I thought about it.
Everything is an equation now.
Everything is a calculation.
Everything has a cost.
I try to balance risks.
I study statistics and results.
But in each equation I calculate, the result is always time.
Nothing is more valuable than time that I am able to enjoy the world and those around me.
December 21st, 2013 §
 When I was growing up and there was a particularly tough day my mom would use the expression, “Mama said there’d be days like this.”
When I was growing up and there was a particularly tough day my mom would use the expression, “Mama said there’d be days like this.”
Yesterday was one of those days.
My husband and I left the house before dawn. At about 8 AM I started my appointments. First was a physical exam with vitals taken and a review of symptoms. I met a new oncologist who was filling in while so many of the doctors were away (Friday of a holiday getaway week). We arranged this match because she is the Principal Investigator on a new clinical trial the team has been discussing as a good fit for me. As regular readers know, in my last post I explained that my cancer has progressed in some spots (stable in others) so we need to try to find something better now.
We reviewed my scan results and what she and my regular onocologist think we should do next. A slot in a new trial opened this week and it seems to be a reasonable next step to try another non-chemotherapy method. I’m going to save the details of that study for a later post but for those of you who know and understand the jargon, this one involves a Novartis drug called LEE-011 which is a CDK 4/6 inhibitor in combination with an anti-hormonal agent. This clinical trial is what I’m signing up for next.
The protocol for this drug is very challenging. It involves many trips to the city, especially in the first month where it will be once or twice a week, sometimes just for a blood draw. Some of those visits will be 8 hour sessions where blood is taken a few times to check drug levels in the blood before and after taking the pills. None of the blood draws can be done near my house since the conditions and testing all must be carefully controlled as part of the study. I’ll enumerate side effects and other details in a later post but this one looks to affect me more in daily functioning than I’ve had to deal with in the last few months. I’m definitely nervous.
We talked for a long time about the study. I had already gotten word from my oncologist about her own recommendation. I signed consent forms. I scheduled the necessary tests. They require a CT scan (I just did one, though it falls 2 days outside the testing window. We should be able to get an exemption for that so that I don’t need to redo it). I will need a PET scan, likely need a repeat bone scan, an echocardiogram (this drug can have cardiac side effects), an electrocardiogram, blood test, urine test and, (rats!) a liver biopsy. All of these must be completed in the next two weeks during my “washout period” (interval of time where you are not taking any chemotherapy agents and so you are starting with a clean slate to measure effects in a new clinical trial). Of course, the holidays are not an easy time to accomplish all of these.
I then went to get chest x-rays to monitor my pleural effusion (fluid in the sac around my lungs that makes breathing difficult). After those x-rays and fasting until almost noon I had 40 minutes to finally grab a quick bite. Then I went to the main hospital to meet with a pulmonary physician to decide what to do about the pleural effusion and find out how bad it actually is.
I had a full medical history and symptom assessment with a nurse and then met my new pulmonary doctor. He told me that my left lung is compressed to about 50% of its usual size from the fluid that is there. He estimated 1.5 liters of fluid have accumulated. He said it “layered” on x-ray which means it’s still flowing and therefore would be easier to extract. We decided to do a procedure called a thoracentesis to drain it. One of my morning blood tests that had to do with clotting had come back high, something that would mean we couldn’t do the test. We figured out it had been drawn from my port, which should never be done for clotting tests because they use an anti-clotting liquid called Heparin to flush the port each time and that would lead to inaccurate results.
Through a lab snafu it took 2.5 hours to get the new results rather than 40 minutes. By the time we finally had the all-clear to proceed it was about 5 PM. I still had barely eaten or had anything to drink. For the draining they sit you on a table with your feet dangling and have you bend over a stand for support. It is very much like having an epidural placed. They use local anesthetic to numb the skin and then stick a needle between your ribs, insert a catheter and vacuum extract the fluid (which should take about 10-15 minutes). The doctor got the catheter in, got a small sample of fluid going and…
My blood pressure plummeted. My heart rate dropped. I got hot and woozy and clammy. Yup, I passed out. They had to remove the drain and get me on oxygen and lay me down. I revived quickly, but we could not continue. So, I have the pain from the needle in my back but nothing to show for it. I will now have to go back on Christmas Eve to try again (fully hydrated and fed, hopefully this will be the key). I was obviously disappointed and emotional by this point. I had to go get the X-ray you need to confirm that no damage was done by the needle, and we made a train that got us home at 8 PM. It was a long exhausting day without too much to show for it in terms of relief.
It’s hard not to feel defeated on some of these long days when it just seems the mountain is so big to climb. Right now we are making a change to try to get better results in controlling cancer progression. I won’t be able to to travel for the holidays anyway, but now I will be spending time in hospitals rather than resting at home and taking a break. Cancer doesn’t give a damn about Christmas. Or families. Or anything that matters to me. But my doctors do. And they continue to show caring and concern and work so hard to try to make things better. Without that help and support this would be so much harder. Even when mistakes happen (and yesterday there were quite a few with blood draws and lab tests and so on), every doctor apologized. I definitely shed tears many times yesterday out of frustration, which doesn’t happen too often.
As I waited for my results I watched the office staff exchanging gifts, talking about holiday parties and Christmas cookies. One by one they packed up their belongings and turned out the desk lights. I was the last patient left in that department. That was hard. But I also know that I got to walk out of the hospital last night. I still got to go home and sleep in my own bed. And when I got home I made it just in time to hug my children and see Tristan’s artwork, all sparkly and smile-inducing. He asked me at bedtime why I couldn’t go on vacation with the rest of the family again this year. I explained to him that altitude makes it harder for me to breathe. The air is thin, and I would not feel well. I asked if he understood. “Yes, but I am still sad you can’t come.” “Me too, honey. Me too.”
I’m going to need to dig deep over the next 6 weeks. I’m going to need to ask for help with child care and logistics while I’m recovering from procedures and having so many trips to Sloan-Kettering. That’s not easy either. I find it very hard when I feel that I’ve not been strong enough, or that I’ve complained about the way a hard day has gone. I know it’s normal to need to just cry and complain and say to the cold night-time sky, “This isn’t fair. This isn’t how it is supposed to be.” Sometimes you just need to vent, though.
I need to be strong for the next few days and what they will bring. I want to make the holidays joyous for my family to the degree I can. These are the tasks that make me feel like me. The family shopping is done, the teachers’ gifts distributed, the tips for those who help during the year have been handed out, the holiday cards sent. These are the things that I know I could get a “pass” on. But they are the things I value. I will always try to show my gratitude to others.
Yes, Mama said there’d be days like this. But tomorrow is another day. And I don’t lose hope that it will be better.
December 18th, 2013 §
 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.
December 12th, 2013 §
 Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Before each meeting with the Principal Investigator on the trial (an oncologist) I usually meet with a research nurse. On Monday I had the added pleasure of meeting with the Fellow assigned to this trial. She is a fabulous doctor: thorough, curious, caring. We spent more than 45 minutes going over a checklist of symptoms we must review at each appointment. I need to answer if I am having any of those symptoms, describe them in detail, and rate if they are better or worse than at the last visit. Then we discuss what to do to help alleviate the symptoms. Certain medications are allowed and others are not because they could conflict with the investigational drug.
At this visit my main issues were muscle pain in my back, fatigue, occasional bone pain in my collarbone, continued loss of appetite (though my weight has stabilized), occasional shortness of breath, dry skin and cracked heels, and some minor GI issues. My blood pressure and heart rate are elevated. My pleural effusion has stayed at the reduced level, fluid continues just in the lower left lung lobe.
In general, I feel quite good on the combination of GDC-0032 and Fulvestrant. I’m quite happy with my current quality of life on the combo especially compared to other options like IV chemo. I hope that it will continue. I have historically tolerated targeted therapies very well. I have not had any issues so far with mouth sores, rashes, or serious GI issues which are some of the more common side effects with the investigational drug.
I was able to ask all of my questions, most having to do with the coming two weeks. Next week is a big milestone: I will have my first CT scan and that will be the basis for determining if I can continue in this clinical trial. At least two radiologists will examine the CT. One radiologist from the hospital will read the images, while a second, separate radiologist assigned to the trial will make his/her own determination as to how much disease there is compared to the baseline CT 7 weeks ago. If the cancer metastases are considered stable or decreased, I will continue in the trial. If the cancer has progressed (grown) by 20% or more, I will need to stop taking the drugs and be removed from this trial. There are defined days that are the days I must have this scan done so that all of us taking part in the trial are assessed at comparable points in treatment.
Next I met with the Principal Investigator on the trial. This is the oncologist who is the point person for the trial and supervises all of the patients in the trial at Memorial Sloan-Kettering. We reviewed how I am doing in general, what the plan is for the coming 2 weeks, and discussed bloodwork. I told her that am anxious to hear how the other people enrolled in the study nationally are doing. Because we all started within a few weeks of each other, there aren’t many reports yet.
Because I have completed my loading doses of Fulvestrant (an extra dose of the drug is required in the first month of treatment), I did not have to get those injections this week. That was a treat. I will now receive the two injections monthly.
My medication diary documenting the time I stop eating each night and the time I take my medication in the morning was checked as were my pill quantities. I scheduled my next visit (adjusted a few days earlier because of holiday schedules there, I have a +/- 3 day window for the appointments now) and headed up to the third floor to have my blood drawn.
My port incisions are healing beautifully. I’ve toyed with posting a photo of what it looks like but haven’t decided about that yet. The nurse and I donned the requisite masks for port access and the blood draw was easy. I was then allowed to take my GDC pills and start the clock on the 60 minutes until I could eat and drink (I must always wait one hour after taking them). I left the hospital about 3 hours after I arrived.
We’ve been watching my tumor markers and aren’t quite sure what to make of them. They’ve been rising a lot in the past month but I am also getting varied results from my two testing sites. Of course, the key piece of data to look at is the scan. But it’s been a challenging few weeks emotionally as I see where the markers are, watch them rise, and wait for the scan to tell me what’s truly going on inside by body. In a few days I’ll have answers. And then I’ll either be continuing on the trial for another two months or moving on to plan B (which my team and I have already identified).
I continually try to bring my focus back to the distinction between worrying and planning. Worrying is anticipatory. The way I look at it is that worrying is spending time thinking about things that may or may not be/come true. Planning is taking strategic action to set things in place and control things that I can control in the midst of so much uncertainty.
Having a backup plan or a next step if the scan brings bad news next week is planning. It means if this trial isn’t working I know what I will do next and make sure those steps are in place so I’m not suddenly reeling and trying to cobble together a plan. But worrying about the results next week won’t do me any good. The cancer is doing what it is doing. These drugs are either working or they are not. And my sadness or frustration about that won’t change the reality of the cellular processes.
And so I have been quieter this week, choosing carefully how to spend my time. I’m searching for joy each and every day and finding beauty in the small moments: our dog Lucy playing in the first snowfall of the season, Christmas shopping with Paige last weekend, puzzling through math homework with Tristan, Colin and I getting haircuts together and going Lego shopping.
We hug a lot.
We say “I love you” a lot.
We always have done this.
But now I hold on for an extra second each time and I squeeze just a little tighter.
………………………………….
For those readers new to my posts about this clinical trial, you can see my reports about Cycle 1, Day 1 here and Cycle 1, Day 16 here and my port placement and Cycle 2, Day 1 here.
November 26th, 2013 §
 On Friday morning after I sent our three children off to school I traveled to Memorial Sloan-Kettering Cancer Center (MSK) to have a port implanted. My first appointment of the day was at 10:15 to have an electrocardiogram (EKG/ECG). MSK requires an EKG on one of their machines within 48 hours of the port procedure. It takes longer to find the bathroom than it does to have this test done. Electronic leads are attached with sticky sensors to specific points all over your body and hooked up to a machine. After about one minute of recording you are done, and the sticky round patches and the attached wires are removed. Easy as can be. The test measures the electrical activity of your heart to make sure it is normal. I won’t go into details on this test because it’s such a piece of cake and so common.
On Friday morning after I sent our three children off to school I traveled to Memorial Sloan-Kettering Cancer Center (MSK) to have a port implanted. My first appointment of the day was at 10:15 to have an electrocardiogram (EKG/ECG). MSK requires an EKG on one of their machines within 48 hours of the port procedure. It takes longer to find the bathroom than it does to have this test done. Electronic leads are attached with sticky sensors to specific points all over your body and hooked up to a machine. After about one minute of recording you are done, and the sticky round patches and the attached wires are removed. Easy as can be. The test measures the electrical activity of your heart to make sure it is normal. I won’t go into details on this test because it’s such a piece of cake and so common.
After that test was complete (by 10:08) I went to a different floor in the same building to the Interventional Radiology department. There, a friendly team checked me in and sent me to the waiting room, a large attractive area brimming with patients and family members. After a little while a woman called my name and I was taken back to be prepped for surgery about 30 minutes before my scheduled 11:15 arrival time. I will say that for every test and procedure I’ve had so far at MSK’s main hospital they have been on early or on time. This has been a pleasant surprise at such a large medical center.
Once we reached a small prep room a very cheerful nurse gave me a garment bag to store my clothes in and I changed into a standard issue hospital gown with a thin navy blue bathrobe to wear over the top. She weighed me, measured my height, and reviewed my medical history. This was the first surgery I had at MSK so I had to review my surgeries and allergies along with current medications, etc. They wanted to do another pregnancy test but I refused on the grounds that I had an oophorectomy and the test was unnecessary. Because the surgery had not been done there they didn’t have the exemption in my file. They confirmed that I had not used any blood thinners (including medications or pain remedies that can act as blood thinners) in the days prior to surgery.
I then met the surgeon for the first time and he and I discussed the precise placement site of the port and also the ramifications of my sensitivity to adhesives. Usually it’s not too much of an issue but for this procedure the surgeons usually close the incisions with Dermabond (skin glue) and my skin cannot tolerate that. Sutures would be used instead.
The surgeon pinched the skin between my collarbone and the top of my breast implant and said that there was enough tissue there to use the preferred port, called a MediPort or PowerPort. Each person has a different amount of fatty tissue in this area, and a mastectomy may affect this as well. Age, body type and other factors can affect which model of port can be used and where it will be positioned. Obviously, children and people using a port for only a short period of time may have different limitations and needs. There were a few times during the day when someone said to me, “You’ll just have this for a while and won’t even know it’s been there after it’s gone.” They assumed that I would only need it temporarily. “It’s here for good,” I said more than once.
There are many different kinds of ports. They have changed a lot over the years. The one I have is quite small and is triangular in shape. This shape is an indicator that the port can be used for injections of contrast dye (these are called “power-injectable”) in addition to being used for blood draws and any future IV chemo. The power-injectable feature means that when I go for CT scans, bone scans, or PET scans, the technician can inject any dye that might be needed for that test into the port rather than having to use an IV line into my hand or arm. This is one reason I decided to get the port. Being in clinical trials now means frequent blood draws and scans.
The nurse started an IV in the holding area and I was wheeled through a maze of hallways until we stopped outside the operating room. I got off the gurney, walked into the OR, and hopped onto the table. After a lot of prep including hooking me up to monitors and draping and cleaning the area, they finally pushed Fentanyl and Versed into my IV. I didn’t actually go to sleep but probably could have. They numbed the two incision areas with local anesthetic and after about 15 minutes including a few periods of tugging and pushing it was over. I’m going to just link to the actual description that MSK gives about the procedure itself. I’m not sure I can explain it any better than they do.
I stayed in the OR for about ten minutes and then was wheeled to a very small private recovery room where I stayed for about an hour. The one surprise is that in the Interventional Radiology department’s recovery area at MSK they do not give you anything to eat or drink after procedures. So I needed to wait until I left to have anything (tip: if you are going to have a port placed, tuck a snack and drink in your bag. After fasting until the procedure you will want something convenient to eat and drink afterwards and radiology departments might not provide them the way that surgical recovery areas often do).
My husband was able to join me in this recovery area after I was settled. A nurse reviewed my discharge instructions. I needed to wait slightly longer to get the incisions wet than usual because I did not have the Dermabond. Usually it’s a 1-2 day wait. I was quite sore immediately after and was glad I had put a cushion and pillow in the car. If your port is put on the right side, as mine is, the passenger side seat belt will not be pleasant so I recommend bringing a padded seatbelt cover or other method of cushioning the strap. I was quite sore for about 24 hours, but quickly that shifted from being generally aware of the pain to being very localized and only when using that arm. That quickly became localized discomfort if touching it. Today (three days later) it’s still sore to the touch but otherwise not bothersome. I did not use any pain medication.
The port is much smaller than I would have thought. It’s placed so low that it won’t be visible in a tank top. The surgeon was very careful to try to pinpoint a location that would be cosmetically most appealing which I appreciated since this will not be temporary. Eventually I will need IV chemo and this will be used for that as well. For now there are two red incisions but I know those will fade. They are far more visible than the port, a bump under the skin the size of a quarter.
I will not be able to use the port for blood draws that I do near my home and many people are not aware that not all phlebotomists can access the port. Only certain people (most often at hospitals and oncology offices) can access the port because you need special training and also special equipment. In addition, if you do not use the port for a period of about 30 days you must go to have it flushed (with saline and Heparin) to prevent clotting. It only takes a minute to do that.
I’m happy to answer any questions that readers have about the port or anything I missed in the description.
…………………………………
Today I was back at MSK for my regular clinic day for Cycle 2, Day 1 of my clinical trial of Genentech GDC-0032 + Faslodex. I met with a nurse first who checked my weight, blood pressure, oxygen saturation, did a physical exam, reviewed my side effects (I won’t go into those in this post). Next I met with the Principal Investigator on the trial who is the one in charge of my care during this time. I gave her the four remaining pills of my 30 day supply (two each of 1 mg and 5 mg capsules of GDC-0032) and signed and turned in my medication log which lists what time I stop eating each night and what time I take my pills each morning. We discussed scheduling for the month which includes my CT scan three weeks from now where we will get our first look at what, if any, effect the drug combination is having on the cancer.
Next I went to the chemo suite to get my Faslodex injections and have my blood drawn as required by the protocol. I had a different nurse this time from the last two times. I told her that I had a new port and asked her to explain the process for the draw now. She warned me it might be sore as she palpated it to find the right spot to insert the needle and also said the actual needle stick might be a bit more painful today depending on the exact location of my incision.
We each needed to put masks on to cover our nose and mouth during the blood draw to minimize the chance of infection. She gently felt for the circular center of the port where the reservoir is and inserted a special needle to access it. It was a bit tender but certainly not at all more painful than my usual stick on the back of my hand. It really was just a second and it was great to know there was no chance of “failure”… blood would flow! And it did. Six tubes were done quickly and then she flushed the port with saline and Heparin to prevent clotting. The needle was removed, a gauze and paper tape bandage applied (no adhesives for me) and then we removed our masks. Easy and no anxiety. These steps must be taken every time.
Next it was time for the two nasty Faslodex injections. As I’ve written before these are two jumbo intramuscular injections, one in each butt cheek. The nurse kept apologizing and saying how she hates to give them because they’re just so big and painful. They are always very sympathetic when administering these. Today’s were painful, I think the worst of the 3 rounds I’ve had. I think it’s just chance about where they hit and also that I’ve had to do them every two weeks this month during the loading phase. Now I will only need them every month so there is longer recovery in between from the soreness and muscle pain. I find that a heating pad is the most comforting way to ease the pain, I’m definitely getting used to it and also knowing what to expect.
Once done I stopped into the pharmacy (right next to the chemo suite) to pick up my next month’s supply of GDC-0032. I needed to wait to take today’s dose until after my bloodwork. I took my pills with a glass of water while still standing in the pharmacy and noted the time in my new medication log. I would now need to wait one hour before eating or drinking (as I always do when I take my dose each morning).
I went down one floor to scheduling, made my next appointments, and was on my way about 2.5 hours after I first walked back to the exam room. I met a friend for breakfast and had that blissful first cup of coffee at precisely the time allowed. I took the train home, and fell asleep on the way.
I’ll be back at MSK in two weeks for an appointment with the doctor and bloodwork. The week after that will be my scan and then I’ll be back again a few days before Christmas to begin Cycle 3 if all is stable.
If my cancer has grown (“progressed”) by 20% or more, however, the drug combination is deemed not working. I will stop the trial (and be dropped from it) and I will need to move on to something else. I’m already at work researching what that next choice should be.
…………………………………….
We are entering a fragile time of year. The holidays are difficult for many people. Some miss loved ones who have died. Some mourn their own lives, no longer what they were. Grief takes many forms. The pressure to create memorable and uplifting occasions can sometimes be oppressive.
Be kind to those who are struggling during this time; physical and mental illnesses can be especially difficult to manage. Understand that happiness and sadness can coexist. Reach out to others if you can.
Find a bit of beauty in the world. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
November 18th, 2013 §
 I’ve never forgotten seeing the black and white cow with a window carved into its side. I was in grade school, living outside of Milwaukee, and always loved going to the Wisconsin State Fair each summer.
I’ve never forgotten seeing the black and white cow with a window carved into its side. I was in grade school, living outside of Milwaukee, and always loved going to the Wisconsin State Fair each summer.
There was a beautiful cow lazily eating in a pen, indifferent to all of the people milling about.
When I walked around the enclosure to see its opposite side, however, the cow was anything but normal-looking. The cow’s left side had a glass-covered hole in it. The man standing next to it and stroking its head was talking about cows’ digestion. He said the window allowed access to the cow’s stomach for research about nutrition and illnesses. The man then shocked the audience by opening the cover of the hole and reaching inside the cow’s upper stomach to extract a handful of grass that was in the process of being digested. The cow remained aloof.
I have now learned that the cows are called “cannulated cows” or “rumen-fistulated cows.” I have been able to confirm that my memory of seeing one at the Fair is correct. As I remember it back then, the window looked more like a miniature glass dryer door, one that swung open with a small hinge on one side. I am not sure of that. The photos I see of cannulated cows now have a different look. To learn more about rumen-fistulated cows you can watch this video which is extremely interesting.
I woke up thinking about that black and white windowed cow this morning.
I woke up wanting a window into my body and what is happening inside right now, this very minute. I want to know if the clinical trial I’m participating in is having any effect on my cancer. For now we use other indicators but they are unreliable. Even blood tests for tumor markers lack validity and reliability in many people (why they are not used as screening tools to diagnose breast cancer in the general public).
And so I forge ahead, taking pills, getting injections, wondering if it is doing anything to keep my metastatic breast cancer under control. Side effects vary day by day. Yesterday was a bad day. Terrible back pain, gastro issues, a migraine, and fatigue had me down for most of the day. But today I feel better.
So I focus on today.
I envy the researchers who gain knowledge in real time. I envy the way their information can be analyzed and promptly used to help sick cows.
I wish I had an immediate view inside, an indicator as to what my body is doing. Instead, the image of the black and white cow with the window in its side stays with me.
November 14th, 2013 §
 Tuesday was a full day for me at Memorial Sloan-Kettering for Cycle 1, Day 16 of my current clinical trial.
Tuesday was a full day for me at Memorial Sloan-Kettering for Cycle 1, Day 16 of my current clinical trial.
With snow flakes and rain mixing in the morning rush, I decided to skip the train and go early with my husband as he made his usual morning commute to New York City by car. I knew this would get me to the office quite early. I was the first to arrive in the waiting room and didn’t mind the long wait. It gets very busy and noisy later in the day and I’m always happy to sit in warmth and comfort of a quiet room. I arrived at about 7:20 and my first appointment wasn’t scheduled until 8:30. I was fasting, so I did miss my morning coffee quite a bit while waiting, though, especially as other patients began to arrive and use the coffee machine!
I meet with the research nurse first. She weighs me (down 2 pounds from two weeks ago), takes my blood pressure (oops, very high using the machine, we’ll retake it manually, oh that’s much better, thank you very much), pulse (in the 90s), oxygen saturation (better than last time, now normal).
We review how I am feeling on the Faslodex and GDC-0032 combination. This is the first time I am discussing it with the team since starting the protocol. She goes through a list of symptoms and asks about each one. The list ranges from gastrointestinal issues (very important to monitor on this investigational drug) to neuropathy to dizziness to fatigue to rash. I am pleased to report that I feel quite good on the combo. I experienced a few days of hot flashes and night sweats from the first injections of Faslodex two weeks ago, I tell her, but that was it. From the GDC I really only have had appetite loss, metallic taste in my mouth, a bit of muscle pain, and slight fatigue as the most noticeable issues. In general, we both agree, I am tolerating it very well.
The biggest change I’ve experienced in the last two weeks is a drastic change in my breathing– for the better. I’m quite sure, I tell her, that my pleural effusion (excess fluid in the lining around the lungs) is almost resolved. This is great news and I am anxious to find out if my doctor hears the change. I also tell her that after much thought I have decided to have a port placed to make my blood draws and tracer injections for CT and bone scans easier.
Next I meet with my own oncologist. Usually I would meet with the Principal Investigator for this appointment. She was not in the office on the usual days this week, though, and I must have my check-ins on certain days in the cycle. I was told about the switch in schedules well in advance. The plan for the long term anyway is that I will transition back to my own oncologist for monitoring. The two doctors work closely together and there is no problem in doing this.
I haven’t seen my oncologist in what seems like a while (probably about one month) and we are happy to be “reunited” for this appointment. We review how I am doing clinically. She also gives me a physical exam and listens to my lungs. Yes, she agrees, there is a big change for the better. We discuss the port, and she orders the needed additional bloodwork for it.
We talk about the trial and other topics. As always, she asks about my family and writing. I tell her about the song I wrote and promise to send her a link to it. I tell her I have been invited to come talk to the class of Fellows at Sloan-Kettering in a few weeks about caring for the metastatic breast cancer patient. I am truly excited about this invitation. There isn’t anything I can think of that is more important than talking to young physicians about ways to make doctors and patients partners in care in light of a metastatic cancer diagnosis. I’ll share more about that visit as the time approaches.
Next I do scheduling for the next appointment in 2 weeks. That will be a much shorter day than today. Each appointment in the first 8 weeks on the protocol has different elements. Today will be a long day. Next time will just be a visit with the Principal Investigator and a blood draw.
 Next I head upstairs to the chemo suite where they have a room waiting for me. They have already called downstairs while I am doing scheduling to tell me which room to go to so I don’t even need to check in. The nurse I had last time comes in to the chemo room. I immediately tell her that she did a wonderful job with the two huge injections of Faslodex last time. I tell her the slow injection rate seems to have worked; I was sore for days (expected) but no bruising or welts. I always try to give as many compliments as I can; I think these oncology jobs must be very stressful and I would bet the complaints come often. If possible, I try to find something good and comment on it. Everyone likes being appreciated.
Next I head upstairs to the chemo suite where they have a room waiting for me. They have already called downstairs while I am doing scheduling to tell me which room to go to so I don’t even need to check in. The nurse I had last time comes in to the chemo room. I immediately tell her that she did a wonderful job with the two huge injections of Faslodex last time. I tell her the slow injection rate seems to have worked; I was sore for days (expected) but no bruising or welts. I always try to give as many compliments as I can; I think these oncology jobs must be very stressful and I would bet the complaints come often. If possible, I try to find something good and comment on it. Everyone likes being appreciated.
Today I will need to have my blood drawn, take my GDC-0032 pills, wait four hours, and have my blood drawn again. I must always wait one hour after taking the pills to eat. By the time I do all of this today it will be noon. The nurse gets a vein in my wrist easily for the required 12 vials and when we see it’s a good flow we agree to leave the line in and try to use it four hours from now and avoid another stick. I’m reactive to adhesive so she wraps me up carefully and I slide my sweater sleeve back down.
I take my pills with a full glass of water and document the time in the medication diary that I am required to keep. Then it’s time to drop my trousers for the two big Faslodex injections. I am not too nervous about this part now that I’ve done it once already. I will get these today, again in two weeks, and then monthly thereafter. I have mastered the art of muscle relaxation for these shots and use a trick of putting all of my weight on one foot while they inject the opposite side. Again the shots are uncomfortable because the viscous liquid is getting rammed into a muscle. But she does it slowly again as she is supposed to, and we’re done quickly. I still am self-conscious as the lightly-frosted sliding glass doors are all that stands between my tush and the hallway, but I’m already over that. I think the idea of facing the wall and clutching a table as needles are jabbed in my backside is probably more laughable.
I put on my coat, knowing the worst is over for the day and go meet a friend for lunch after waiting the required time to eat.
Later, I return directly to the same room I was previously in at the appointed time. The line still in my wrist yields a good flow, a few more tubes are drawn, and we’re done for the day.
Seven hours after first entering the building I am free to go. I still have two more weeks’ worth of the GDC-0032 in my bag and so I do not need to visit the pharmacy. At the next visit my medication log will be checked and my remaining pills will be counted and confiscated before I am given another 30 day supply.
…….
Over the last two days I have ended up needing two more blood draws, met with my local oncologist, and got my monthly Xgeva shot. After 7 needles in 3 days I’m glad to now have a few days off. I ended up needing to repeat one of the tests required for the port placement procedure (Tests related to clotting are routine before any surgical procedure. One of these was slightly elevated and I needed to repeat it. The second test came back just fine).
I also had my tumor markers done. This blood test is not a part of the clinical trial requirements. I’ve decided to watch these to see what they do while taking the drug. I’m sure some people would not choose to do this. This week’s test showed the numbers were quite elevated over previous weeks. We don’t know what that means. I have no increased pain, none of my other bloodwork shows any reason for concern. The numbers sometimes rise on new therapy before they drop. My breathing is significantly improved. So, we focus on the clinical signs and will just have to see what the markers do. I wish they had dropped, but I’ve seen the imperfect nature of this test time and again. I am able to realize this is only one piece of the puzzle right now. It doesn’t affect anything about my treatment plan. A reminder: in this trial success is measured by doing CT scans at varying intervals. My first one will be five weeks from now, at the seven week mark. Only then is a determination made about whether it is working, which would be disease stability or reduction. If the overall “quantity” of cancer is seen as growing by 20% or more, I would discontinue the trial and need to move to something else; it would be considered ineffective for me.
I was sore far more quickly after the Faslodex injections this time even though they weren’t any more painful at administration time. By the time I was on the train back home in the late afternoon I was hurting. For three days now I’ve had a heating pad on as much as possible. It just feels good. The seat heater in my car is getting a workout too. I know it will only be another day or two so I am not too bothered.
I don’t yet have a date scheduled for the port placement. That could be as soon as next week. I also have meetings with my cardiologist (these inhibitors can drastically change lipid levels. My cholesterol and triglycerides on my previous drug, Afinitor, went quite high. Thankfully they are coming down rapidly now but we still need to watch them carefully.) and my endocrinologist (my thyroid levels are now abnormal again. I have Hashimoto’s Disease which is usually very easy to manage but chemo does sometimes cause changes). I’m not in a huge rush to get the port, I just would like to have it in by the time I need to do the next round of scans.
I’m glad to finally be done for the week with appointments, hard to believe the weekend is almost here. I will see what next week brings and then it will be time to be back at MSK on the 25th of November for Cycle 2, day 1.
 It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.
It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.










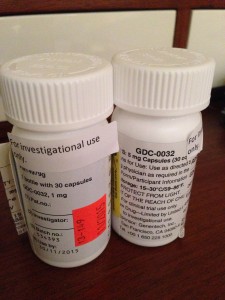




 Link to Twitter
Link to Twitter