March 1st, 2015 §
Hi, Things have gotten exponentially harder in last few weeks. I needed a few paracentesis drains (stick catheter in and drain excessive fluid in abdomen) in shorter and shorter increments at hospital.
A week ago 5.5 liters were removed. This process then was going to need to happen again after only ten days. The fluid is coming from my liver because of the cancer.
I was admitted to hospital Wednesday and had a Tenckoff catheter put in. I was not a candidate for the Denver shunt because my platelets run too low and an internal shunt would be dangerous.
They removed another 5 liters of fluid at surgery. Now I have a catheter that allows me to drain myself at home. But, so much fluid removal in short period messes with electrolytes, BP, etc. and makes you feel rotten until you get equilibrium.
Still cannot walk — no change predicted in short order. We are installing ramps, bought wheelchair, etc.
For now that is all I have energy to update but should give you sense of where things are.
Xo, Lisa
February 12th, 2015 §
 Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.
Once again, it’s been a while since I’ve updated. Somehow most of you know that with me usually no news does not actually equal good news. Before I give an update I want to remind readers that I do update the blog Facebook page (click here to reach it) with short medical updates more often these days if you are interested.
Most of the last three weeks since I last wrote have been dealing still with swelling and blood count issues from radiation and from the extensive disease in my liver that we are working on with the radiation and with chemo. I’ve needed numerous transfusions of red cells for anemia and quite a few for platelets which have really come under attack. We have been taking a break from the Epirubicin and I got a dose of Faslodex (I had it last year as well in a clinical trial with a trial drug, this month I am using it with a daily pill, Letrozole). Rather than being cytotoxic chemos (traditional “cell-killers”) these are anti hormonal agents. We are just trying to let my body recover now for a few weeks.
Last week my abdomen grew and grew with fluid from the liver and overall inflammation. By the end of the week I had an abdomen the size I was when I was ready to give birth. The skin was painfully stretched. We needed to intervene. I went to urgent care for evaluation for a paracentesis (draining/”tap” of fluid). My platelets were too low. They transfused and I just made the cutoff. The process is pretty simple: visualize if the pocket of fluid is drainable (tiny pockets would not be) via ultrasound.
Three needles of increasing gauge are inserted to numb through to the pocket. A catheter is inserted and attached to a drainage bottle that has a bit of vacuum to draw out the fluid. Two and one half liters later we were done. It is a huge amount to see. I did have soreness at the site and discomfort from such a lot of fluid removal after. But this is a very common procedure with metastases to the liver (please, please remember: breast cancer that metastasizes to the liver is not liver cancer. Mets to the brain are not brain cancer. They are breast cancer cells that have moved in the body. There can be/are big differences in terms of prognosis, treatment, chemotherapy agents, etc).
Some patients only need a few of these abdominal taps. Some need them every few weeks depending on how chemo, etc. are working. Sometimes a drain is actually placed to allow a constant ability to remove fluid.
If you were following me last year you know I had a drain placed in my lung while in the hospital that accomplished something similar. I was fortunate to only need that one for a few weeks (I had already had a one-time tap on my left lung called a thoracentesis). For now there are no plans for a drain or other more serious interventions in my abdomen. Now that my potassium levels are holding steady we are using diuretics to manage the issue.
We are working on the plan for next week, it is likely that I will be going back to a chemotherapy called Xeloda (these are pills taken daily) for a bit because it is gentler on blood counts. I’ll update when we have a decision on that.
I’m weak, still unable to drive, or do much more than walk than to the bathroom or a car that is picking me up. I’ve had to adjust some things at home including bathroom rails and so on. Safety is most important and especially with very low platelets falls and any bleeding or injury risk is a serious concern.
I’m sure I’ve forgotten something (or things) but I do want to get this out today. I see snow out the window but I’m still focused on Spring. These hydrangeas in my room this week reminded me March is not far off.
Thank you to those near and far for all different kinds of support given this month with an extra shout-out to my wonderful team at Sloan-Kettering. If any of my doctors, nurses, or support staff there are reading this: you help make these tough days better. I value your care always.
January 17th, 2015 §
 Hi everyone… finally an update. I know I have been quiet. As you probably assumed, it has been a very difficult month. I finished whole brain radiation (and I needed to add the C2 vertebrae) and liver radiation a month ago. The brain and liver were two week regimens each but the start times were staggered so it took three weeks to complete. I was having trouble with my magnesium and potassium levels and those needed to be addressed. As a result I needed to be at Sloan-Kettering every weekday for more than 30 straight days between radiation and the aftermath. It was quite a schedule.
Hi everyone… finally an update. I know I have been quiet. As you probably assumed, it has been a very difficult month. I finished whole brain radiation (and I needed to add the C2 vertebrae) and liver radiation a month ago. The brain and liver were two week regimens each but the start times were staggered so it took three weeks to complete. I was having trouble with my magnesium and potassium levels and those needed to be addressed. As a result I needed to be at Sloan-Kettering every weekday for more than 30 straight days between radiation and the aftermath. It was quite a schedule.
In the last few weeks my problem became swelling (edema) from inflammation from the liver radiation. My abdomen was shockingly distended and that was causing me trouble with discomfort and moving around.
I have had fatigue but it hasn’t been the sleeping-all-day form that I was warned might happen with the brain radiation. Fatigue encompasses more than just “tiredness.” For me the fatigue has been more weighted on weakness. I have had a lot of trouble walking and doing steps. I’ve needed to use a wheelchair at SK for a few weeks now. That shouldn’t last much longer as I get stronger to walk distances again. But on the bad days I couldn’t get more than down to the car for my ride.
I started Epirubicin for my chemotherapy a few days after radiation finished in December. It is dosed based on liver function so the dose has been adjusted each week as we see how my liver is doing post-radiation. I was able to get three straight weekly doses. This current week has been my “off” week; my blood counts are low from three straight weeks of chemo (to be expected in anyone getting it) so a week off is always given for the body to hopefully make enough the replenishment cells of different types.
The magnesium and potassium as of this week are finally holding with home management and no IV supplementation. A helpful tip: the low sodium form of V8 has huge quantities of potassium. Most people think of OJ or a banana to supplement. Only 8 oz of it contain 900 mg of potassium. I drink a few a day, just make sure it is the low sodium version though.
I’ve now tapered totally off the very low steroid dose I had been on for months. Steroids can make your legs very weak if you take them for an extended period of time so it is good to be able to remove them from the equation.
I only needed to go to SK for one trip this week. Diuretics have helped with the edema, each day I see and adjust the dose. I do not have pain beyond what is caused by the fluid around the liver. I do not take any pain pills and haven’t needed them during radiation. I have not had any headaches or neurological issues yet from the brain radiation which is probably due to the fact that my lesions were so small and the low dose of steroids. I am still winning a bunch of my Words with Friends games too! The last time I was able to leave the house to go somewhere except to go to Sloan-Kettering was Thanksgiving. That boggles my mind.
I think this week has been a turning point. I am hopeful the major acute radiation effects are waning. No clue what lies ahead with the delayed ones but I don’t focus on that. For now I will be working on strength (after being basically bedridden for a month) and trying to get more function back. It is a process.
If all goes well I will start a new chemo cycle next week. Radiation effectiveness can’t be assessed immediately so we will do preliminary scans in a few weeks. (I finished on 12/19). Each day is different and I can’t predict how I will feel. But that seems to be the way life will be for me now. I long ago adjusted to that.
I am grateful for all of the support and concern shown over the last month from you, I understandably wasn’t able to return many messages. This past month was really about just getting through. The energy I did have was spent making sure the kids were able to maintain their usual schedules and we made it. Friends who have helped with rides and meals: thank you.
The poppy photo above is from my garden a few years ago… I’m already anxious for Spring to get here. xo
December 27th, 2014 §
 Hi all, a short update.
Hi all, a short update.
I’ve finished two weeks of whole brain radiation (those two weeks had simultaneous radiation to my C2 vertebrae), and two weeks of liver radiation (one overlapping with brain, so all of this was 3 weeks of treatment). I have been overwhelmingly plagued with intense fatigue and other side effects (fatigue is the worst thing at the moment though).
I need to use a wheelchair when I go to Sloan-Kettering now. I’ve needed platelets and red cells once each in the last few weeks and have needed to be at Sloan for one half-day every weekday for the last month or so because my magnesium (despite daily infusions) remains critically low, which is a dangerous situation. My potassium has similarly started to be an issue as well. I get magnesium and potassium in addition to 1.5 to 2 liters of fluids as well each day because I have been having trouble staying hydrated with the radiation effects. Not enough energy here to go into why the magnesium is still an issue now.
Four days ago on Tuesday the 23rd, I began chemotherapy (4 days after finishing all of my radiation). We are starting a new drug called epirubicin which is an anthracycline just like the well-known adriamycin (it is also red like adriamycin).
So basically I’m spending a half day at MSK every weekday and resting (I’m basically bedridden right now) at home the rest of the time. I don’t leave the house except to go to MSK. I expect at least a few more weeks of this.
I’m thrilled that my family has gone away on vacation starting today and they will have a week to ski and be with cousins and grandparents and get a fun break while I recover here. I insisted that they go; it is so important for me to know that our kids and my husband can have some vacation time and get a break. It is not easy to be a family member/caretaker under these conditions so it gives me a lot of joy that they can have a change of scenery. I have a family member staying with me since I can’t be alone and so that will work out just fine in terms of appointments and help with my needs.
I get foggy quickly so I hope this post made sense!
Many thanks as always to those who support me daily with tweets, emails, rides to appointments, donations to my research fund, meals, etc. And to any MSKCC staff who are reading this: you know how much I adore you.
I am grateful that you all continue to join me here. Wishing you a happy and healthy new year if possible and we’ll keep on going into 2015 the best we can…
xo,
Lisa
December 11th, 2014 §
 These are very rough days. Finishing whole brain radiation tomorrow (Friday), have completed one week of liver radiation and have one more week to go. Immediately after I complete those (Christmas week) I will go back to systemic IV chemotherapy. The Y90 SIRT procedures to the liver are not able to be done right now because the brain mets needed immediate attention and we couldn’t afford to have the 6-7 weeks of full Y90 procedures afterward while the rest of the body went untreated.
These are very rough days. Finishing whole brain radiation tomorrow (Friday), have completed one week of liver radiation and have one more week to go. Immediately after I complete those (Christmas week) I will go back to systemic IV chemotherapy. The Y90 SIRT procedures to the liver are not able to be done right now because the brain mets needed immediate attention and we couldn’t afford to have the 6-7 weeks of full Y90 procedures afterward while the rest of the body went untreated.
It is possible since we are only radiating the right lobe of the liver right now that we will later Y90 the left lobe if we can get some stability after radiation and chemo but that is to be determined. You always have to be willing to adjust to what the day brings and what the best new course of action is.
For now I have side effects of being wobbly, absolutely fatigued (unable to walk well or move), dehydrated, pain and nausea. It hasn’t gotten to the worst point it will and we are managing medications each day to deal with each days’s issues. My palliative care doctor and my medical oncologist as well as radiation oncologist are all monitoring me closely.
I have been at MSK for IV fluids and magnesium 4 days this week, radiation for five days this week, and tomorrow I will even then need to head down to NYC for platelets for clotting and red cells to combat my anemia. We need these numbers to be up so I can continue radiation and then get right into chemotherapy again.
I’m not functional for the most part and the days are very tough. But I know this is what needs to happen before I can get my strength back and the cancer under control. These are important weeks and months.
That’s all I have energy to report for right now, thank you for the support.
December 3rd, 2014 §
 I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week.
I realize it has been a while since my last update. Things have been very busy with getting my whole brain radiation going. I’ve spent so much time at Sloan-Kettering… yesterday I was there for 7 hours. By the time I get home I am too exhausted to write. But I do want to let you know where we are this week.
The first thing I want to comment on is the death of my dear friend Ann Gregory. She died the day before Thanksgiving. Her obituary appears here. Some of you came to know Ann through Twitter or through my stories about her in person or through her comments here on the blog. If you did get to know her and chat with her on Twitter over the past few years, you were lucky.
Ann was the strongest person I know and had numerous diagnoses of cancer throughout her life including leukemia and squamous cell carcinoma. She was quite stoic and, like me, was always okay as long as there was a plan for what to do. We spent hours texting each other (often those hours could be in a single day, depending on which one of us was sick or well that day or what phase of treatment we were in), always supported each other, and she was always a valuable source of information for me. I have missed her so much in the week since she has died. We did not want to leave each other. Four days before she died she texted me to say her goodbye. I will never delete those text messages and I am so sad that I have to do all that I have to do without her. My heartfelt condolences go out to all of her family, especially her husband, Chris, and her legions of friends. Her blog appears here. I just can’t do her life and personality justice here right now, but there is a gaping hole in my life now, and Ann is the precise shape of that hole.
…………………………………………………..
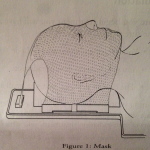 Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.
Last Friday I did my mask-fitting and simulation. The mask-fitting takes about half an hour and is pretty unpleasant. The mask is molded to be skin tight on your face, to the point of leaving indentations when removed. It is rigid plastic, not flexible mesh. There are no eye holes or openings for your mouth… your chin is jammed up so tightly that you couldn’t open your mouth if you wanted to. I cannot speak at all when it’s on and attached. Obviously, this is vital to making sure the radiation is going exactly where you want it to go, and not where you don’t.
Even though the fitting and simulation take a while, each radiation session itself is quite short. After confirming the patient’s identity with name, birthdate, and a photo, you lay down on the table, they hand you a foam ring to hold on to across your chest so your arms are relaxed and easy to keep still, and a foam wedge is placed under your knees. Then the aforementioned mask is placed on and with some tugging and effort, attached firmly to the table you’re on. The photo gives an idea of what it’s like.
The technicians leave the room and the linear accelerator moves into place. The beam goes on and I can see even through my eyelids a very bright light with a bluish cast. It is only on for less than a minute and then it moves and does the same thing to the other side of my head. They say there is no smell to radiation but I always smell something. I have read that others do, too. I can’t describe exactly what the smell is. I’m working on figuring it out. I’m usually focusing on relaxing and not getting claustrophobic so I haven’t solved the mystery yet. It doesn’t quite smell like burning hair but maybe that is part of it. After the actual beams are done then the techs scurry back in right away and release the mask from its mooring. That’s it.
As I said in my last post, side effects don’t usually start for brain radiation until closer to the end of the 10 session series. So, next week I will see more of the fatigue and the start of hair loss. Memory loss takes a bit longer to occur. There are many things that might happen including headaches and nausea and confusion and blurry vision but those are not as common. I did not have any neurological symptoms before starting radiation so that is a good thing. I have some nausea and loss of appetite but that is primarily due to the liver situation. An inflamed liver causes pain, nausea, and so on.
I did my liver simulation for radiation yesterday. This is actually more complicated for the radiation oncologist to map out than the brain because part of my liver already received radiation when I had the radiation to my spine in January. For this reason, she needs to make sure it doesn’t get any additional radiation this time. None of the 13 or so tattoos (permanent ink dots placed by a needle under the skin to mark where the alignment should be for the laser beams for radiation) that I had from the spine and pelvic radiation in January were in the correct spots for the liver so I got about 6 more of those. The radiation oncologist will focus on the right lobe of the liver, but even that is tricky with the kidney and bowel in range.
They will work to map it this week and I will start liver radiation next Monday. That means this week (12/1-5) will be brain only, then one week (12/8-12) of both brain and liver, then one week (12/15-19) of liver only. Then I will wait a few days and begin chemotherapy again. These are hard days ahead. Side effects will be kicking in right as I go back to chemo. Christmas week will be the peak for all of this to hit the fan.
I’m continuing to get IV fluids 2-3 times a week and am also getting magnesium infusions because the most recent chemo continues to cause my magnesium level to stay far too low. Even though I am not getting chemo right now (in this case, chemo and radiation can’t be given together even though with some cancers they are) I am still having lingering effects from the last round of Cisplatin. The magnesium infusions add about 8 hours a week to time I need to be at MSK (Memorial Sloan-Kettering).
There really isn’t time to do anything else besides be there and rest at home. I’ll be there every weekday for the next few weeks. I’m managing okay and know it’s going to get far worse before it (hopefully) gets better.
I think this should give everyone a pretty good timeline of what I’ll be doing in the next few weeks so that if I can’t update much, you’ll still know. I know people have questions and I will do my best to answer them, it might just take me longer than usual.
Thanks for all of the support, as always.
November 24th, 2014 §
 The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
The brain MRI on Friday unfortunately showed that the metastases are to my brain, not just my skull. There are many tiny malignant lesions in the brain (imagine salt sprinkled onto a bowl of popcorn) so I am not able to do focused gamma knife radiation to shrink them individually. I will need whole brain radiation to try to shrink them all before they cause me to have symptoms.
Whole brain radiation will radiate all of my brain tissue, healthy and malignant. It is usually given in a series of 10-15 sessions, every weekday. It has side effects both short term and long term. In addition there is a claustrophobia-inducing session of mask-fitting where a mold of the face and head must be made for the patient to wear during radiation treatments to immobilize them. Here are some photos that one woman made of her WBR process.
I am meeting with the radiation team on Tuesday to get all of the details and do the scheduling. I haven’t met with them yet. I believe the goal is to start next week. I do not yet know what this means for the radiation procedures I had scheduled for my liver. I will also be continuing with chemo as much as is possible during this time. The most serious side effect will be fatigue. As in: sleep 20 or more hours a day fatigue. Can’t get out of bed fatigue. So I will need to make arrangements to get more help here at home to help with the kids and with driving.
For now that’s all I’m going to report because I want to see what the team says about my particular case and let everyone know the plan for me. It’s obviously not the news I was hoping for. But as always I will do what needs to be done to try to manage it.
November 19th, 2014 §
 Nothing poetic here today. Just a report.
Nothing poetic here today. Just a report.
The past week was already one of the most challenging I’ve had this year: my first infusion last week of a triple dose of Cisplatin had me down for the count while I was also digesting the news of the growing liver metastases and what needs to be done to try to reduce those. This week I had a PET scan and CT angiogram of the liver scheduled to assist in my pre-surgical requirements for the Y90 Yttrium radioembolization I talked about in my latest update (the Y90 process is also called SIRT: selective internal radiation therapy).
As a result of the PET scan we got some additional information and what we got was not good. Obviously that isn’t a surprise given that my bloodwork had already told us the prior chemos had stopped working and the cancer has been progressing. The PET confirmed that my liver is an area of increasing trouble with tumors multiplying and growing in size. Not surprising. Also as we suspected, the fluid around my heart appears to be malignant. Then there were surprises: apparently at least one malignant lesion in my brain and new cancerous areas throughout my skull and jaw.
The PET is not a good way to identify exact size and precise location of specific tumors, however. Therefore, on Friday I will need a brain MRI to get good imaging and see exactly what is going on. Then we will see what needs attention, what is watch and wait. Not all brain lesions should be radiated with gamma knife surgery immediately; it is a risk/benefit assessment when you’re shooting radiation into the brain. Obviously, though, gamma knife surgery is a treatment that will be considered once we have details on what we are looking at.
Skull metastases, despite sounding scary, are just bony mets. This is what systemic chemotherapies (treatments that are given orally or through IV that work throughout the whole body) are designed to work on. Brain lesions often need different therapy because many/most drugs do not cross the blood/brain barrier (or do so in an indirect or imperfect way) and so are not effective in counteracting metastases to the brain. Metastases to the brain often require a change in therapy to address this issue.
For now we proceed with the liver plan because that is a local therapy designed to work on just that issue. It needs attention now and isn’t changed (yet) by this new information. As for the rest, I will just have to see what the brain scan shows and go from there. It will be a long week of tests and waiting. Sometimes I wonder how I walk around knowing what is in me and what it is doing to me and still manage to get through the day. I have seen the roller coaster of what this disease does. Some things that sound terrifying end up being able to be managed.
We will be scheduling chemo intermixed with my liver procedures (day before, or maybe a few days after), adjusting the chemo doses to lower ones so that there is time for my blood counts to rise in the time needed. It will be an art and science to balance. By then we will know if the Cisplatin is working. I can only hope that it is and that it will. We have a few choices lined up for if it isn’t.
While all of this goes on I still search for that laugh, I still appreciate the small things.
Most people know my “bit of beauty” tweet by now (“Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.”). Judy Clement Wall has made this into notecards and a print and is donating all funds from sales through 2014 to my research fund at Sloan-Kettering. If interested, go here to her Etsy shop. I know that this is the quote many people will remember me for most. But I have another tweet I like to send out. Some days this one just feels right. It is:
Make the most of this day. Whatever that means to you, whatever you can do, no matter how small it seems.
For now, and again, I say: Onward.
(A housekeeping note: for anyone who has signed up to receive these posts by email but sees that posts aren’t arriving: you must confirm your subscription by clicking the verification option in the first email you will receive. If you have been wondering why you aren’t getting the emails, please re-sign up from the home page at www.lisabadams.com, upper right corner, and make sure to verify. There are loads of unverified requests and only you can do this part!)
November 14th, 2014 §

Some days I don’t
Feel like a gift,
Do much,
Go anywhere,
Want to do this.
Some days I don’t
Know how to get out,
Or want to be the brave one,
Be the strong one.
Some days I don’t
Understand quite how I got here,
Care to see where it is going,
Even want to imagine what it will be like after.
Some days I don’t
Have any words,
Or the strength to take them from my head
And put them on a screen.
Some days I don’t
Believe that this is what my life is,
What it has come to,
Or even think I have woken up for the day.
Some days I don’t
Wish to believe the best days are over,
Know if the adventures have ended,
Want to believe that it can be true that they are.
But even on the days I don’t…
Somewhere inside I know I must
Press onward,
For whatever that means,
For right now.
So every day that is just what I do.
November 7th, 2014 §
 This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
This week has been one of disappointment and adjustment. I met with the interventional radiologist on Wednesday afternoon to discuss what can be done for the metastases to my liver and what options are available. While chemotherapy has done a remarkable job in clearing up the cancer in my chest (it is resolved; if there, is small enough that it doesn’t show up on the scan), there are metastases to my liver that are chemotherapy-resistant. This means they have grown despite the fact that chemo that has worked well in other areas of my body.
Unfortunately, what I learned while reviewing the scan with him is that I don’t just have two tumors in the liver. Instead there are actually many tumors in my liver, with those two being the largest. The fact there are so many tumors is why I am not a candidate for external beam radiation or other non-invasive treatment.
So far I am still a candidate for the Yttrium 90 radioembolyzation procedure where radioactive beads are inserted via a catheter snaked up through the groin into the hepatic artery and subsequently “feed” the tumors radioactive material as the beads work their way into the liver.
It will take three separate procedures spaced about two weeks apart to get this done. I will start the first week of December and finish in January. The first procedure involves mapping things out (in essence, a “dry run” where mock beads are inserted) and the next two are actual placement procedures. This is all a joint approach between interventional radiology and nuclear medicine. Before I start I will need a CT angiogram of the liver and a PET scan. After treatment I will have to monitor progress with PET scans every three months.
In the meantime we need to start on a new IV chemotherapy right away to try to see if we can find a chemo that will work on the liver tumors. We have no way of knowing if we will find one or what it will be. Right now my oncologist is eyeing Cisplatin, a platinum-based chemo like the Carboplatin I was on this summer. We will make the decision by next week and begin then.
The liver situation is serious. The cancer is growing rapidly there and we need to get it under control. Results of using Yttrium 90 for breast mets is pretty good, definitely good enough to proceed with it. To be honest, it is not a choice about whether to do it (I’m not at a point where I would consider doing nothing and stopping treatment, I realize that proceeding with any type of treatment is a choice in and of itself). There aren’t other options to treat these in a “batch” way.
So, there is a lot of adjustment right now. I feel sadness, disappointment, and anger that chemo has worked so well in some areas but the liver has been resistant. Things change so fast with this disease. One day things are relatively stable and within weeks they can be spiraling out of control.
As always, I will continue to educate and do what I can to show what my life with metastatic breast cancer is, what life with the disease can be.
For now, I will begin a new chemo and proceed with plans and pre-surgical testing for December. I’ve appreciated the emails and comments so much and I thank you all for your concern and wishes. I am sorry that I can’t respond to them all individually.
November 5th, 2014 §
 A quick update.
A quick update.
I received my fourth round of Navelbine yesterday and I’m feeling incredibly rotten today. We’ve now confirmed that this drug is not working (at least as a single agent), so I probably will not have to put up with it much longer.
Yesterday I learned my liver tumors are too big to do the ablation procedure we had hoped (please see update on 11/7 for some corrections to this paragraph). Instead, later today I will be evaluated for a more complicated procedure called Yttrium 90 radioembolization. I will learn more about it today but the general idea is that a catheter is snaked up through the groin to one of the two blood supplies to the liver. While the liver usually gets 75% of its blood from the portal vein, when there are tumors present they often get almost all of their blood from the hepatic artery. The interventional radiologists insert radioactive beads of glass or plastic into that artery so when the tumor gets its blood supply, that supply is radiated and hopefully shrinks the tumor locally, without disruption of healthy cells in the rest of the body. Only one tumor can be treated at a time. It is not a cure, it is just palliative for these metastatic tumors to try to stabilize them or reduce them. I will also need to be off chemo for a week on either side of the procedure.
I also need to be seen tomorrow by the cardiology team at Sloan-Kettering for another opinion on my pericardial fluid situation now that I am having some symptoms and have had more imaging done. They will decide if we need surgical procedure to drain the fluid and biopsy it. It is probably malignant but we can’t be sure. If they don’t feel we need to do any intervention right now, we will watch and wait.
So, we have some big decisions to make including what chemo to go to next. I won’t go into those options here now. First I need to deal with these more pressing issues of the liver and the heart. I had hoped to be able to rest and get through these difficult post-chemo days at home but the appointments mean pushing myself beyond what I really think I’m able to do sometimes. But I have to get answers and be able to get scheduled for what I need when I am hopefully feeling a bit better next week.
Once we have some decisions made about it all I will report back. Things just don’t seem to go the easy or simple route and I’m getting used to that. For now I am going to try to conserve energy and stay pretty quiet. Thanks to you all for your continued support.
November 2nd, 2014 §
 Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Last week didn’t quite go as planned. I was hoping to post more pieces here to finish out October with some of my favorites. I will still try to get those up in the coming weeks. What prevented me from doing so was a week that became dominated with medical appointments.
Monday I saw my cardiologist to try to get some information about some symptoms I’d been having. My echo (and later in the week, the CT scan) showed there is some excess fluid around my heart. For now it is not causing any effect on heart function but we can’t rule out that it is a problem. I’ll have to repeat tests in a few weeks to try to see if it grows in volume (this would indicate a more sinister issue, and we would need to rule out a malignancy). For now, though, that goes on the back burner.
Tuesday I had bloodwork and IV fluids. The bloodwork is still a bit unclear about if the current chemo (Navelbine) is working. The rise in tumor markers is slowing but we need some definitive results this week, I think, to feel confident in interpreting them. The bloodwork also revealed I was anemic again, so on Thursday I went to New York City and got a transfusion of two units of blood.
On Friday I had a CT scan to compare to my last scan and help us make decisions about treatment. The CT showed both some good news and some concerns. While the lymph nodes and malignant tissue in my chest have resolved (chemotherapy in the last six months has worked and reduced those areas), my liver unfortunately shows two tumors.
The best thing at this time would be to biopsy portions of them (to gather tissue for future testing; my cancer has rarely been in areas that we can actually get samples, so this presents a rare chance to grab some) and also do ablation on them. Ablation is a localized procedure that when successful, destroys tumors of a particular size with very few side effects.
So, a lot is up in the air at the moment.
Because it is only Monday morning I don’t know what this week will bring in regards to chemo. We also don’t yet know if the interventional radiologists will decide that I am a good candidate for the ablation. For now, I wait.
Palbociclib, a drug I received through the expanded access (formerly “compassionate use”) program from Pfizer should arrive this week. That process took approximately 9 weeks and usually takes longer than that. I am fortunate my oncologist kept the process moving in such a timely manner (all applications and documents for such use must be done by the physician, not the patient).
I’m not feeling that well and have been primarily staying home for the last month. Now that I think about it, though, I’ve been basically staying home for the last ten months. Many days my half hour in the morning driving the older two kids to school is my only outing of the day. But I am patient.
At this point the options are still very reasonable and typical for this stage of the disease. I’m waiting for the next treatment proposal and then onward we go.
October 22nd, 2014 §
 The past few weeks have been some of the most challenging this year. By the time you read this I will have had my third Navelbine infusion. Unfortunately, we do not have any evidence so far that it is working. Each chemotherapy that I try at this point only has about a 30% chance of working even for a short period of time.
The past few weeks have been some of the most challenging this year. By the time you read this I will have had my third Navelbine infusion. Unfortunately, we do not have any evidence so far that it is working. Each chemotherapy that I try at this point only has about a 30% chance of working even for a short period of time.
For now, we anxiously wait. But that waiting means that the cancer is progressing. Increased fatigue, pain, nausea, weight loss, shortness of breath and weakness are my companions right now. I do have my team helping me manage these side effects, but there is trial and error involved. Also, at this point an increased cancer load is part of the problem. The only thing that will truly help that is to find a systemic therapy that works, and let it do its thing. For that reason I haven’t been able to post as often as I wanted this week.
I do want to share that the book auction to raise money for my metastatic research fund at Memorial Sloan-Kettering is now live, and it runs through October 24th. This is an exciting event. You can bid by posting a comment including the amount of your bid below the photo of the box you want (you must live in the USA to participate). All proceeds fund research and do NOT go to my personal medical care. Boxes of signed books have been donated by authors and then collected and curated by Erika Robuck. You can click here to go to the Facebook page and then scroll down to see all of the boxes.
Last year the event raised over $4000 and we are on track to blow that out of the water. If you want to donate directly to the research fund but don’t want to participate in the auction, don’t have Facebook, or don’t want to deal with Facebook, please feel free to go here. Donations of any amount are so appreciated.
For today’s October re-post I’ve chosen one of my first pieces, one that readers ask for again and again. I have decided to revise it here, now that my diagnosis has changed. I’m keeping the original post online, though, and you can see that here.
………………………………………….
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
My first diagnosis with breast cancer took its toll on me and I was quite sure I would never, ever be the same.
I had no way to know then that “never, ever the same” would mean something worse, something fateful, a juggernaut.
I told myself “they’re only breasts.”
I said, “I don’t need ovaries, I’m done having children.”
But that obscured the truth.
The truth is that it did matter,
They do matter.
They said my uterus was atrophied.
It almost sounded funny when they said it.
“Who cares? What does that matter?”
It did. It does. It will.
At the time, to get rid of all hormones was thought to give me a better chance at avoiding a recurrence, but there was a price to be paid.
No estrogen mattered more than I ever thought it could.
It felt worse than taking injections to suppress my ovaries, worse than taking Tamoxifen.
Those were easy.
I had no clue what was ahead.
I wore the skirt, I put the makeup on, I walked the walk.
But I did not feel like a woman anymore.
I most certainly do not feel like much of one now.
Make no mistake, I am proud of what this body has done for me.
My three children top the list.
But now I must focus on some of its cells,
now malignant,
throughout this body,
growing at a horrific pace.
My body has now become a personal science experiment.
Sometimes, when things are going well, you could look at me and have no earthly clue.
You see,
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is just a part of what breast cancer can do.
This is just a part of what breast cancer has done to me.
This is part of what can happen
Even with early detection and treatment.
This is what can happen even years later.
This is why people should not prematurely claim victory.
This is why you are not necessarily safe.
This is what breast cancer could do to you.
This is how what some think they have “beaten” or “bid goodbye to” can still
kill.
This is what it will do to me.
October 17th, 2014 §
My last post (“The Hardest Conversation”) showed you what a conversation with my teen daughter was like when we talked about my diagnosis of metastatic breast cancer in 2012. Today I wanted to share a conversation with my youngest child (now 8) that happened last year so you can see the variation in what their concerns were and how I dealt with each one.
As always, with cancer, age-appropriate explanations are important. Another vital piece of advice I’d like to share is that with all children, but especially young children, it is important to talk more than once about the topic. At the end of the first conversation I recommend asking young children, “Can you tell me what we talked about today?” to see if they have absorbed the most important pieces of information and that these pieces are correct. A day or two later it is always a good idea to ask, “Now that you’ve had time to think about our chat, do you have any questions?”
The following post was written in late 2013 on the eve of the surgery to put my medi-port in.
………………………………………………
 “Why do you have to have surgery tomorrow?” seven year-old Tristan asks from the back seat after we drop off his 11 and 15 year old siblings this morning.
“Why do you have to have surgery tomorrow?” seven year-old Tristan asks from the back seat after we drop off his 11 and 15 year old siblings this morning.
“Because I need to have something put in my body called a port. It’s a little container made of something cool called titanium that lets the doctors put some of my medicines into my body in an easier way.”
“Can you see it?”
“Yes, you will be able to see that there is a lump under my skin, about the size of a quarter. But you will only see the lump. You won’t see the actual thing because that will be inside my body. You know how I have the scar on the front of my neck? It will be like that, here, off to the side, same size scar but with a bump under it.”
“Is it like the bubble I had on my neck when I was a baby?”
“Well, that was a skin tag, so that was a lot smaller. And they were taking that away. This is something they are putting in to help make it easier to get some of my medicines. And you know when you go with me and I have blood taken from my hand? Well now sometimes they will be able to just take it from there instead. So it helps with a few jobs.”
“Will you have it forever or do they take it out when your cancer goes away?”
(Driving the car, trying to keep tears in check, knowing this is a vitally important conversation. I’ve explained this to him before but I know it’s hard for him to understand.)
“Well, honey, remember I had cancer when you were a baby? Well, this time the cancer is different. A lot of the time you can have cancer and the medicines and surgeries make it go away and it stays away for a long, long time. Maybe even forever. Sometimes any cancer cells that might be left go to sleep and just stay that way. Sometimes you have bad luck and they wake up. Mine woke up after six years. And now the cancer cells are in places that I won’t be able to get rid of them all for good. I am always going to have cancer. This time my cancer is the kind that is always going to be here.”
“You’ll always need medicine. And the thing they are putting in?”
“Yes, honey, I will always need medicine for my cancer. And I will probably need to have the port in forever too.”
Long silence.
“I am glad you are asking me questions about it. I want you to always ask me anything. I will try to explain everything to you. I know it’s complicated. It’s complicated even for grownups to understand.”
Long silence.
“Mom, did you know people whose eyes can’t see use the ridges on the sides of coins to tell which one they are holding? So if you have a big coin with ridges that person would know it is a quarter?”
“That makes sense. How did you learn that?”
“At school. And so if it’s smooth you know it’s a nickel or penny. It’s important that they know what coin it is.”
“I think you’re right. That is very clever.”
( I stay quiet waiting to see where he will take the conversation next.)
“Remember when my ear tube fell out and was trapped in my ear and the doctor pulled it out and I got to see it? It was smaller than I thought it would be.”
“Yes, I thought the same thing.”
“I really wanted to see it. I wanted to see what it looked like.”
“Me too.”
“Can you show me a picture of it?”
“Of what?”
“The thing for tomorrow.”
“The port?”
“Yes. Or don’t you know what it will look like?”
“I know what it will look like. Sure, I will show you on the computer after school.”
“Okay.”
“It’s time for school but I am glad we talked about this. I want you to keep asking questions when you don’t understand something. I love you, Tristan. I hope you know how much. I know this is hard for all of us. I wish it were different. But we are going to keep helping each other. And talking about all of this is good. We can do that whenever you want.”
October 15th, 2014 §
 From the time my oldest child, Paige, was born everyone kept telling me, “Just you wait.”
From the time my oldest child, Paige, was born everyone kept telling me, “Just you wait.”
When she made it through the terrible twos without much of a tantrum everyone kept telling me, “Just you wait.”
When she made it through elementary school and a move from NYC without trouble they kept saying, “Just you wait.”
“Just you wait,” they said, “girls are drama. You got lucky before. But the teen years? Oh boy… just you wait.”
Today she prepared me a bowl of soup and brought it up to my bedroom. I was resting after my surgery to remove malignant lymph nodes and tissue for testing yesterday, the room was dark. I invited her to come snuggle with me in the big bed. We’ve never let our children sleep in our bed so they think climbing in is a big treat.
I asked her if she wanted to talk about what was going on, about my news about having metastatic breast cancer. She did.
And so it began: an hour-long talk that started with her first question, “Are you scared?”
She asked questions about genetics and risks of getting cancer to what kind of treatments I might need.
She asked me again, as if to confirm for herself, “It’s not curable, right?”
We talked about my writing, about being public with my health status, about being open and honest with her and her brothers.
I told her that yes, I was scared. I explained that my fear usually comes from the unknown, in this case just how I will respond to treatments. I told her it was okay to be scared. That it’s normal, that sometimes fear makes you brave enough to do things you don’t think you can otherwise do.
I told her that I understood that sickness could be scary, that I didn’t want her to be afraid of me as I got sicker someday. “I would never be afraid of you, Mom. I’m only afraid of cancer,” she said. My heart squeezed and thrashed and the tears flowed.
We talked about her desire to be a doctor, a surgeon. She wanted to know what all of my surgeries and treatments had done. She wanted to know the difference between cancer “stage” and “grade.” We talked about the genetics of breast cancer and discussed the BRCA-1 and 2 genes (which I do not have). We talked about hormones and their role in puberty, menopause, and cancer. She wanted to know why outcomes are so variable. How will we know if treatments are working? I told her about the importance of her monitoring her own health, how hopefully we will have better screenings down the road.
I told her that for now I want her to live her life, for our house to be as normal as it can be for as long as it can be.
I told her she should try to focus on her schoolwork, her sports, and her friends. She told me that I was more important.
I told her that eventually I might need someone to help take care of me. “I will take care of you, Mom. You’ve always taken care of us,” she said.
We talked about her brothers, ages 11 and 6 and how she was going to have to help them. And her dad too. “I’m really good with hospitals and medical things, Mom… I’m just like you.”
She said she liked that I was open about it. That people knew. She thought it was best to be honest and appreciated the offers of support she’d received from friends and adults she knows.
I told her that what we were doing, lying there talking for an hour together about this, was the most important thing we could be doing today. I told her there wasn’t anything more important to me than my family. My job is to help them deal with this. Whatever this is.
I explained that what she needed from me would likely differ from what her brothers need; she is older and each of them would have different needs along the way. It’s my job to figure that out and address it. And my husband’s job now, too. How I take the lead on this will be important.
She asked if that was a lot of pressure, to have so many people reading my words, watching what I was doing. I told her it was. I told her it was my way of trying to help people. The same way that she wants to be a doctor to help others… well, I have always tried to see if I could help in my own way. And the way we talked before about the unknown being what’s scary? Well, my writing here means it’s less mysterious. Knowledge helps. Even if the knowledge is not what you want to hear, knowing is better.
Denial won’t change the course of things, and often makes things worse.
Secrecy is bad. Sharing and supporting are what I champion. And I know that de-mystification is a constant effort. I will continue to teach my children daily. I said I hoped that somewhere in all of this she could see how important science and medicine are in my world. And that if she does decide to be a doctor that is a noble effort. She will make me proud in whatever she does. As will my boys.
The funny thing is how much better I felt after we talked. The conversation was the hardest one I’ve had. The topics are gut-wrenching. But shining the light on them, on this disease, on what happens next, is the only way I know to cope, to help, to keep going.
We talked on and on as I combed my fingers through her long hair. I stroked her smooth, soft cheek. She was giving me strength.
And what I realized about people saying I should just wait because she’s going to eventually act out:
Waiting is a luxury.
Waiting means having time.
And that’s what I want most in this world right now.
October 12th, 2014 §

I make sure my family goes on trips without me now.
It is important that they learn to be without me.
Important that they get time away from here.
Important that they know there can be fun and joy even if I am not with them.
This is what I want.
This is what will be.
It is not easy to be the family of someone who is ill.
I know this is true.
And so I send them away to laugh, to be together, to have fun.
This is what I unselfishly demand.
In April of 2013 we all went to Florida. I didn’t know it would be our last trip together for a while. I could not focus very well. I just knew that life was not the same and it never could be. I had learned about six months earlier that I had metastatic breast cancer. I knew I would never be carefree again. I had intended to stay away from writing for that time, but on this particular day, in this moment, all I could do was realize the agony that was my situation. When I got back to the hotel room I wrote the words that had been in my head.
…………………………………………………
“Floating Away”
 I sit on the beach, feel the sand’s angry texture rub my chemo feet in a way I wish it wouldn’t.
I sit on the beach, feel the sand’s angry texture rub my chemo feet in a way I wish it wouldn’t.
I watch my family in the ocean, turquoise and calm and vast.
My husband flips over, face in the water, takes some strokes out to sea.
His movement is graceful, effortless, just as it was the when I met him 22 years ago.
He was a sprinter on the college swim team then,
and while he laughs and says it doesn’t feel effortless anymore,
nor perhaps fast,
it does not matter.
In my mind’s eye he is that young man,
swimming fast,
joking with his team,
coming over to the stands to talk to me while chewing on the strap of his racing goggles.
I fall in love with him again every time I see him swim.
My three children float, bobbing in the ocean water.
I can feel the distance between us, it feels like a lifetime.
It is my family in the ocean floating away from me.
I see the quartet, I watch as an outsider.
I do this a lot lately.
I watch them from afar and think how it will be without me.
A new family unit.
Behind the big black sunglasses my tears stream down.
Suddenly Tristan is running from the water to me, across the sand.
He stands, dripping, face beaming.
“I just wanted to tell you I love you, Mama.”
I take his picture.
I capture the sweetness.
I grab him, hug him, feeling the cold ocean water on him, melding it to my hot skin.
I murmur to him what a sweet boy he is, that he must never lose that.
I send him back to the ocean, away, so I can cry harder.
By the time they return to shore I’ll have myself composed.
But my oldest immediately senses something amiss.
She mouths to me, “Are you okay?” and pantomimes tears rolling down her cheeks.
Yes, I nod.
I walk to the water’s edge to prove it.
October 10th, 2014 §
 When I die don’t think you’ve lost me.
When I die don’t think you’ve lost me.
I’ll be right there with you, living on in the memories we have made.
When I die don’t say I “fought a battle.” Or “lost a battle.” Or “succumbed.”
Don’t make it sound like I didn’t try hard enough, or have the right attitude, or that I simply gave up.
When I die don’t say I “passed.”
That sounds like I walked by you in the corridor at school.
When I die tell the world what happened.
Plain and simple.
No euphemisms, no flowery language, no metaphors.
Instead, remember me and let my words live on.
Tell stories of something good I did.
Give my children a kind word. Let them know what they meant to me. That I would have stayed forever if I could.
Don’t try to comfort my children by telling them I’m an angel watching over them from heaven or that I’m in a better place:
There is no better place to me than being here with them.
They have learned about grief and they will learn more.
That is part of it all.
When I die someday just tell the truth:
I lived, I died.
The end.
October 10th, 2014 §
 I’ve been struggling with side effects from the new chemo so I haven’t posted for a few days.
I’ve been struggling with side effects from the new chemo so I haven’t posted for a few days.
I know Al Jazeera Television has been rebroadcasting the episode of “The Stream” that I participated in last year. For those who missed it, I want to make it easy for you to watch. This was a rare event because they gave us a full half hour show to talk about Pinkwashing and Breast Cancer Awareness. Dr. Susan Love, Dr. Gayle Sulik, and I were given time to really talk about issues. I give them credit for allowing a whole show for us. To watch, just click on this link https://thinkorbit.app.box.com/thestream101113 (must watch from a computer not a phone).
The photo is of two of my nieces watching me on TV.
October 8th, 2014 §
 It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.
It does not matter how healthy you look. It does not matter if your hair is growing back or you walk a little faster or manage with just one nap a day now.
It does not matter if any of those things are true, your cancer can be worsening.
As I have described here before, metastatic breast cancer is characterized by resistance to therapies. If a treatment works in the first place (and according to my oncologist, most have about a 30% chance of initial success), the cancer will almost certainly become resistant to it and it will cease working. This resistance will happen time after time. This has happened numerous times to me already. I have had some treatments not work at all (Taxol, Fulvestrant+clinical trial drug GDC-0032) while others worked for a few months and then would not work any longer (Xeloda, Aromasin+Afinitor) .
Once again, this resistance has happened. Carboplatin and Gemzar did their work starting in March and did it well, bringing me back from a very dark place this Spring. After 9 complete cycles, though, they are no longer working. It is time to move on.
Moving on is scary. It means being in freefall as we use educated guesswork to decide what agent(s) to try next.
The good news is that I was officially approved to receive palbociclib from Pfizer under their expanded access (compassionate use) program. I will be able to get this drug before it receives final approval by the FDA and therefore before it is on the market sometime in the next year. There is no guarantee this drug will work (alone or in combination with other drugs that are on the market already). It is just one more thing to try.
There are still final bureaucratic hoops to jump through, though, and I won’t have it for at least a few more weeks. This presents a problem: I need a new therapy now. I cannot safely be without treatment for that period of time. It also is best for me to be in a state of control when I start it; the higher a cancer load I carry the harder it would be if what the drug does is provide stability rather than cancer regression. Stability is considered success in metastatic breast cancer drugs. Just keeping things the same, preventing cancer progression, is good. This is considered “success” in using a drug for metastatic breast cancer. However, if you start at a very high cancer load, that stability may be quite intolerable. My oncologist and I feel it is best to have that load brought down (not just held steady), and we don’t know if this drug is a workhorse like that. We can’t count on it to be.
I’ve known for the last week that things were probably over for this chemo. We had tried a higher dose of both drugs already without success. I adjusted to the news over the weekend and yesterday I started on a new chemotherapy regimen. Navelbine is given through my port as an IV “push”; it’s just one syringeful that is given in about 30 seconds. Having a port is really helpful for this one because it is very irritating to veins if you do not have a medi-port implanted in your chest like I do (the port is completely under my skin, it is a lump about the size of a nickel and is accessed with a special needle by the nurses. They can take blood from it, give medication and chemo through it the way you would with an IV except you don’t have to use an arm vein). We are initially planning on a schedule of two weeks on, one week off, but that may change as we go. And of course, if it isn’t working, we’ll have to try something else.
I’m having some other problems now that the cancer is growing so that has been a challenge. Side effects don’t just stop the minute you stop taking a drug. And moving right on to another one means there is no break. It is what is needed though. The good thing is that if you find something that works (like the Carboplatin and Gemzar did for me), they can do astounding things to kill the growing cancer and bring it back under control.
Metastatic breast cancer is like Whack-a-Mole: cancer pops up in places and then can often be whacked back down. If you’re lucky you can play this game for a little while as it takes up residence in different bones and organs. We’ll see how successful we are this time. This is always the hardest time for me mentally: living with the uncertainty of trying to find a new regimen, trying to find something that works, knowing right now there is nothing.
But this is the choice I have made in choosing to treat my cancer. That is the nature of this disease. These are not heroic measures. This is what treating metastatic breast cancer is.
And so we go… onward.
October 7th, 2014 §
 There’s salt on my blue jeans
There’s salt on my blue jeans
And rain left in my hair.
There is a spot of dirt behind his left ear
And mud on his shoes.
I don’t wipe the spot of dirt off.
I stare at it throughout the drive.
I think of when he was a baby, a toddler, a boy.
Now he approaches manhood,
A time when most young men would pull away.
He does not.
He still hugs me in public.
He tells me he loves me.
He doesn’t mind if anyone hears me tell him the same.
He is still mine for a little while longer.
As I contemplate the dirty spot,
I hear the words.
They write themselves
As they often do.
The salt, the dirt, the refrain.
“There is so much left to do.”
It is a track stuck on repeat.
Every moment of my life now it plays.
I showed him a better hamburger today,
He will remember that.
I reminded him about bringing dry socks to the game.
I am quite sure he will forget about that.
I can’t help but smile every time he looks my way.
Or waves from the mound.
During the delay he caught rain in a water bottle,
Shrugged his shoulders when I caught his eye.
He beamed his impish grin.
Later he asks me, “Do you need help?”
He thanks me for coming to his game.
He always thanks me.
He knows.
The salt is gone from my jeans.
The rain in my hair has long since dried.
The dirt and mud are gone too.
But there is so much left to do.
October 6th, 2014 §
 One of the most common questions I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a practical gift for someone who has just been diagnosed and it is a necessity if you are the patient or a caregiver.
One of the most common questions I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a practical gift for someone who has just been diagnosed and it is a necessity if you are the patient or a caregiver.
Being organized is one of the best ways to help yourself once you’ve been diagnosed. When you first hear the words, “You have cancer” your head starts to swim. Everything gets foggy, you have to keep convincing yourself it’s true.
But almost immediately decisions need to be made — decisions about doctors, treatments, and surgeries. Often these choices must be made under time constraints. You may be seeing many different doctors for consultations. Medical oncologists, surgical oncologists, radiation oncologists, recontructive surgeons, internists— there are many different voices that you may hear, and they may be conflicting. It’s hard to keep it all straight in the midst of the emotional news. Not only are you likely to be scared, but also you are suddenly thrust into a world with a whole new vocabulary. By the time you are done with it, you will feel you have mastered a second language.
You can help your care and treatment by being organized. You can also have the psychological bonus of feeling that one part of your care is within your control. Especially if you are juggling different specialists and different medical facilities, you must remember that the common factor in all of this is you. It’s your health. It’s your life. I believe it’s important to travel with a binder of information about your medical history and treatment, as well as notes and questions.
This binder will mean that all of your information about your cancer will be in one place. This will be your resource guide. I cannot tell you how many times physicians have asked about my binder and when I was able to instantly produce test results, pathology reports, or other information they needed, they said, “I wish every patient had one of those.”
I suggest the following:
A heavy 3-ring binder
I think a 1.5″ binder is a good size to start. This size will allow you to easily access reports and pages and have room for the calendar. It will look big at first but you won’t believe how quickly you will fill it up.
Colored tab dividers
I like these to be erasable. I think 8 is the minimum number you will need. If you have a lot of specialists you will need more. The categories you think you will need at the outset may change. It’s easy to erase and reorganize them. Put the categories you will be accessing the most in the front so you aren’t always having to flip to the back. Once the binder is full it will make a difference.
Some starting categories:
- schedules (dates of appointments you have had, when the next ones are due, and how often you need certain tests done)
- test results/pathology (it’s very important to keep copies of MRI, CT, and pathology reports so that you correctly tell other doctors what your diagnosis is. For example, new patients often confuse “grade” with “stage” of cancer)
- insurance (keep copies of all correspondence, denial of claims, appeal letters, explanations of benefits)
- articles and research (handouts, post-surgical information. Ask if there are any websites your doctor does approve of. My own oncologist said, “Do not read anything about cancer on the internet unless it comes from a source I’ve told you is okay. There’s a lot of misinformation out there.”) Keep your post-surgical instructions, any info given to you about aftercare.
- radiation/chemo (keep records of exactly what you had done, number of sessions, dates, drug names, etc. I also asked how my dose was calculated so I knew exactly how much of each drug I received in total)
- medications (drug names, dates you took them, dosage, side effects). I also keep a list of all of my current medications as a “note” in my iPhone. That way I can just copy it down and won’t forget anything on the list. You should always include any vitamins or supplements you take.
- medical history (write out your own medical history and keep it handy so that when you fill out forms asking for the information you won’t forget anything. As part of it, include any relatives that had cancer. Write out what type it was, how old they were at death, and their cause of death. Also in this section include genetic test results, if relevant)
Loose leaf paper
Perfect for note-taking at appointments, jotting down questions you have for each doctor. You can file them in the appropriate category so when you arrive at a doctor your questions are all in one place.
Business card pages
These are one of my best ideas. At every doctor’s office, ask for a business card.Keep a card from every doctor you visit even if you ultimately decide not to return to them. If you have had any consultation or bloodwork there, you should have a card. That way, you will always have contact information when filling out forms at each doctor’s office. For hospitals, get cards from the radiology department and medical records department so if you need to contact them you will have it. Also, you want contact information for all pathology departments that have seen slides from any biopsy you have had. You may need to contact them to have your slides sent out for a second opinion.
This is also a good place to keep your appointment reminder cards.
CD holders
At CT, MRI or other imaging tests, ask them to burn a CD for your records. Hospitals are used to making copies for patients these days and often don’t charge for it. Keep one copy for yourself of each test that you do not give away. If you need a copy to bring to a physician, get an extra made, don’t give yours up. If you need to get it from medical records from the hospital, do that. You want to know you always have a copy of these images.
Keep a copy of most recent bloodwork (especially during chemo), operative notes from your surgeries (you usually have to ask for these), pathology reports, and radiology reports of interpretations of any test (MRI, CT, mammogram, etc.) you may have had. Pathology reports are vital.
Calendar
I suggest a 3-hole calendar to keep in your binder. This will serve not only to keep all of your appointments in one place but also allow you to put reminders of when you need to have follow-up visits. Sometimes doctor’s offices do not have their schedules set 3, 6, or 12 months in advance. You can put a reminder notice to yourself in the appropriate month to call ahead to check/schedule the appointment. Some people like me prefer to use their phones for this, including reminders.
Similarly you can document when you had certain tests (mammograms, bone density, bloodwork) so you will have the date available. I usually keep a piece of lined paper in the “scheduling” section of my binder that lists by month and year every test/appointment that is due and also every test I’ve had and when I had it.
Sticky note tabs
These can be used to easily identify important papers that you will refer to often, including diagnosis and pathology. These stick on the side of the page and can be removed easily. As your binder fills up, they can be very helpful to identify your most recent bloodwork, for example.
Plastic folder sleeves and sheet protectors
These are clear plastic sleeves that you access from the top. They can be useful for storing prescriptions or small notes that your doctor may give you. The sleeves make them easy to see/find and you won’t lose the small slips of paper. Also a good place to store any lab orders that might be given to you ahead of time.
The above suggestions are a good working start to being organized during your cancer treatment. If you want to do something for a friend who is newly diagnosed, go out and buy the supplies, organize the binder and give it to your friend. He or she will most likely appreciate being given a ready-made tool to use in the difficult days ahead.
I also believe a modified version is equally useful for diagnoses other than cancer. When our youngest son was born with defects in his spine and hands it took many specialists and lots of tests to get a correct diagnosis. Having all of his tests and papers in a binder like this was instrumental in keeping his care coordinated. In fact, at his first surgery at The Children’s Hospital of Pennsylvania they gave us a binder to assist in this process. I know some hospitals do this for newly diagnosed patients already.
Maybe my tips will help you or a friend know how to better use the one you already have. You may not need all of these elements depending on the complexity of your case, but I hope you will find some of these suggestions useful.
October 3rd, 2014 §
 It seems like you can’t rank anguish. You shouldn’t be able to “out-suffer” someone. How do you quantify misery?
It seems like you can’t rank anguish. You shouldn’t be able to “out-suffer” someone. How do you quantify misery?
And yet, somehow we do.
“My problems are nowhere near as bad as yours are.”
“I feel terrible complaining to you about it when you are going through so much yourself.”
I hear these types of comments all the time.
I make these types of comments all the time.
Placing ourselves in a hierarchy of pain and suffering serves to ground us; no matter how bad our situation is, there’s comfort in knowing there is always someone who has it worse.
Like being on a really, really long line at the movies or at airport security, as long as there is someone behind you, it somehow seems better.
Hospitals use a pain rating scale: “On a scale of 1 to 10, how bad is your pain?” When our son Colin was in the hospital for 9 days with a ruptured appendix, they asked him to rate his pain. I was intrigued at his difficulty in answering the question. At the time he was 5 years old and didn’t understand what they wanted him to do. Colin didn’t understand the concept of comparing one level of pain to another; His abdomen hurt… that’s all he knew. He used a binary scale to assess his pain: did it hurt or not? As adults we know better: pain is not a yes-or-no question. Rather, there can be levels, ranking, quantification, and comparisons.
These mental exercises are necessary to keep us going through hard times, no matter what type. Before I got cancer, cancer was a “go-to” negative reference point. I mean, how many times had I, and everyone I know, thought or said, “I’ve got health problems, but at least it’s not cancer”?
I had done that a lot.
A benign lump needs to come out? At least it’s not cancer.
A mole needs to be removed? At least it’s not cancer.
My son has hand and neck deformities and a cyst in his spinal column? At least it’s not cancer.
Then one day it was cancer.
So what could I pacify myself with?
At least it’s not terminal.
At least they can remove the body parts the cancer is in.
At least this debilitating treatment will be temporary and I have the possibility of returning to a normal life again.
Then there was the big one: at least it’s happening to me and not my child.
And when I found out that my cancer had metastasized, I could not calm myself with those comforting refrains anymore.
Now it is terminal.
Now they can’t remove the body parts it is in.
Now the debilitating treatments are permanent and I don’t have the possibility of returning to anything close to a normal life again.
I have often said I have hated becoming anyone’s negative reference point. “At least I’m not her” people now often think of me. I always thought that meant they pitied me. I didn’t want that. But now I realize that it is okay for people to be glad they haven’t walked in my shoes– in reality, that’s what I want. I don’t want anyone to be where I have been and where I am; I’d like to be the lightning rod that keeps other people safe. But we all know it doesn’t work like that.
Denial has never worked for me.
Denial doesn’t kill cancer.
I still believe it could be worse.
I know that is true.
And so, for today, I focus on the fact that I’m not the last one on line.
On the really challenging days sometimes that knowledge is all I have.
And on those days, that knowledge is enough.
October 2nd, 2014 §
 There is comfort in routine.
There is comfort in routine.
Some people are superstitious. Sometimes they want the same chemo nurse, the same appointment time, the same chair. “If it is working don’t mess with it” applies to many things about treating cancer.
I am always thinking about continuity and the stories that objects tell. I’ve written twice about the tape measure my plastic surgeon used to measure me before surgery. I’ll post those pieces again this month.
Whenever I sit in a chair in a doctor’s office I think about all of the people who have sat in that chair before I have.
Each person has a story. So, too, does each chair. That chair is the starting point for this piece from 2011.
………………………….
“I think so too”
That chair you’re sitting in?
I’ve sat in it too.
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Radiation. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too.
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too.
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” Anniversary day. Chemo day. Surgery day. PET scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too.
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments. Tears. Avoidance.
Those side effects you dread?
I’ve dreaded them too.
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Mouth sores. Fevers. Anemia.
That embarrassment you’re feeling?
I’ve felt it too.
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Asking the grocery line folks to “make the bags light, please.” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on. Holding on to the bannister for dear life. Passing out in public.
That fear you’re suppressing?
I’ve squelched it too.
Will this kill me? When? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too.
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year” day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
More research. Easier access. Targeted therapy. Effective treatments. Better quality of life. More options. Longer life. Less toxicity. Fewer guesses.
Ultimately, someday, for my children or grandchildren perhaps: a cure.
Don’t you think that would be amazing?
I think so too.
October 1st, 2014 §
 Today is October 1st. It is officially Breast Cancer Awareness Month. To me every month is Breast Cancer Awareness Month. I will have breast cancer for every minute of the rest of my life. I need no reminder of what this disease is, what it does, what it can do.
Today is October 1st. It is officially Breast Cancer Awareness Month. To me every month is Breast Cancer Awareness Month. I will have breast cancer for every minute of the rest of my life. I need no reminder of what this disease is, what it does, what it can do.
To me, it isn’t about pink products, or a five mile walk, or a bake sale. It’s about life and death. My life and death. It is about having cancer detected early and doing everything possible and still being diagnosed more than five years later with stage IV disease.
October 1, 2012 was the day I found out I had metastatic breast cancer. That was the day my life changed.
The average life expectancy after diagnosis is given as 26 months. Today marks 24 months from my date of diagnosis.
I have a lot to say about October, about research, about education, about how those of us with incurable breast cancer are mostly forgotten. I want to do my part to make the voices of people with metastatic breast cancer heard. I will be posting the link a lot this month to the fund I’ve established at Memorial Sloan-Kettering for research into metastatic breast cancer. This month I will also repost some of my own favorite blogposts and also my most-read pieces. I hope you will find posts you have never seen before and find something new in a post you might have read when I first published it.
Some will be practical advice pieces. Some will be purely poetic. Some will be about me, some will be about our children.
I find that when I re-read a piece I find something different in it because I, the reader, am different. I encourage you to tell me posts that have resonated with you throughout the years that you would like to see again or want others to see.
I’m starting the re-posts today with a piece I wrote only about 6 weeks after my diagnosis of metastatic breast cancer.
……………………………………….
“And Yet the Morning Comes”
Each day is different. Each moment, too.
It still seems surreal, this diagnosis of metastatic breast cancer.
It’s strange how quickly the horrific can become regular: the chemo, the side effects, the new routines.
Oncology appointments, IV infusions, medication refills all start to fill my calendar.
I start making lists of things I need to do. I prioritize them.
It’s not always about what’s actually the most important, it’s also about finding things that bring me small moments of joy.
The small moments are the ones that bring tears to my eyes. Tristan’s little voice saying, “I love you, Mama. You’re the best Mama in the whole wide world” is enough to make me misty.
I still lose my temper. I still yell sometimes. Often it’s misplaced anger, a manifestation of my frustration with my situation.
I haven’t suddenly turned into the world’s most patient person. Sometimes cancer makes me the most impatient one, in fact. I feel the clock is ticking. I don’t have time for nonsense. But that’s not a way to be. I will still try to be better.
I try to be the one to do things with my children as much as I can. Even if there is a babysitter in the house Tristan always reads to me at night for his homework: that is sacred. I still save artwork and photographs and remind them to brush their teeth and clean their rooms.
I try to do the little things: helping Colin with a school project, keeping Paige company while she does homework, watching a sports practice if I can. I go to the grocery store and I work on the holiday card. I still take pleasure in getting the stubborn stain out of Clarke’s dress shirt that the dry cleaner couldn’t.
My motto is that I will do as much as I can for as long as I can.
I don’t ever have a moment that I forget about my cancer. I think that’s the part about it being new. Even when I was diagnosed the first time — even after I finished chemo and surgery and all of it– it still took at least a year for me to be able to push the daily fear down. Of course now the fear has been realized. I am living it. I am living my nightmare, one many people share.
And yet, the morning comes.
I see the light of day and I get out of bed. I see the faces of my children. I kiss my husband goodbye when he leaves for work. Each day I have is a day that matters. Each day is one to make a memory with my family and friends.
Each day is one more than I had the day before.
But let’s be clear: there is no joy in this disease.
My appreciation for my days should not be interpreted as supporting the nonsensical idea that “cancer is a gift.” There is nothing positive about this disease; I would give it back if I could. I did not need cancer to show me the value of things. I always knew these things were true. I never took them for granted. I knew what demons could be lurking.
I did all I could. It was not enough to keep it at bay. But maybe, just maybe, I can keep it at bay for a while.
I still haven’t fully come to terms with what this diagnosis means, but that’s because there’s no real way to know. We don’t know enough yet. It is the uncertainty that is the most difficult part for me. Will this chemo be the one that lasts for a while? Will it fail? When? What next? How long will that one last? My body holds the answers, but it’s not showing its hand yet.
I have to learn to ride this roller coaster. I’m just not there yet. And I don’t really know how long that is going to take.
I walk past people on the street and know they have no idea what is going on inside my body.
People in front of me in line at the gas station don’t know there’s chemo in my purse.
I look like everyone else. I have hair on my head. I ask the checkout person to pack the bags light because I can’t carry anything with my left arm now (the cancer has fractured two ribs on my left side).
Sometimes I want special treatment. I want a Get Out of Jail Free card. Most of the time, however, I want to stay home. Hide out. Be invisible.
I’m still processing. Reeling. But while I’m doing that I’m living.
September 26th, 2014 §
 I have become an expert in uncertainty.
I have become an expert in uncertainty.
I don’t know how I will feel from one day to the next. I don’t know if the chemotherapy that worked a few weeks ago will still work today. I don’t know how my body will tolerate what I’m doing. I don’t know how long this all will last.
I was supposed to get chemo a few days ago (Tuesday) as usual. However, when I arrived and had my bloodwork done I found out that the higher dose of Carboplatin the week before had really continued to hit my body hard. My platelets were too low to safely receive chemo. This means I had very little clotting ability. The Gemzar I was due to get that day hits platelets hard so it presented an even more dangerous situation. My hemoglobin was on its way down, too. I was told I couldn’t get chemo as planned.
Instead, during what turned out to be a 13 hour medical day, I received two bags of platelets by transfusion and one unit of packed red cells. I had never received platelets before. I had no idea what they looked like… they look like pale orange juice (shown at left).

This is a great opportunity to share a link to Sloan-Kettering’s online information about blood and platelet donation and eligibility criteria. I do not need designated donations at this time but I do rely on donor blood and platelets so if you are eligible please donate when you can! It’s a great way to help those with cancer for free.
Today (Friday) I was finally able to get chemo. We will see how I tolerate this dose but the plan now is that rather than receiving my next Carbo/Gem in 14 days, I will get it in 11 days to get back on schedule. This means I will have to do a few daily Neupogen shots next week to boost my white count.
There will be another book auction this year with proceeds going to my fund for metastatic breast cancer research. Authors you know and will recognize are donating signed copies in many genres. I will be sharing links here and on my blog Facebook page if you want to window shop or place a bid. That will be in October. Thanks to Erika Robuck again for arranging this; I know it’s a lot of work.
Wishing you all a good weekend, we expect a last burst of summer here in Connecticut.
September 18th, 2014 §
 Paradoxically, the one thing I can count on now is uncertainty.
Paradoxically, the one thing I can count on now is uncertainty.
In my last post I talked about the plan to get Gemzar this week after a higher dose of Carboplatin (and usual dose of Gemzar) last week. Unfortunately, the higher dose gave me some trouble. I knew within a few days of that treatment I would need a blood transfusion this week, but I deteriorated fast over the weekend. I wasn’t able to stand up on Sunday without nearly passing out and when I arrived at the hospital my heart rate would sprint to 165 when I stood up. The higher dose of chemo last week and the cumulative effects of so many cycles of chemo have just beaten my body down a bit for now. It’s hard to believe I’ve made it almost two years now with constant treatment.
I received one unit of blood on Sunday at Urgent Care at Sloan-Kettering and came home to rest and let it do its work. For that reason I did not get chemo this week. Instead I’m getting an extra week to let my body get its strength back. Next week I will move forward with a higher dose of the other chemo drug and we’ll see if these changes can get a response.
In the meantime I was able to get my flu shot. Please realize how important it is to get this vaccine. You absolutely cannot get the flu from the shot. The virus is inactivated (in contrast to the live virus FluMist). According to the CDC the flu and complications from it kill almost as many people each year as breast cancer. Let that sink in. The flu kills about 36,000 people each year. Metastatic breast cancer kills approximately 40,000 people.
Hope you all have a good rest of the week and weekend. This week really felt like Fall here and the garden is changing. The pictured hydrangea is one of the last with color for the season…
September 18th, 2014 §
 I know I’m supposed to stop and smell the roses
I know I’m supposed to stop and smell the roses
But life is going to keep moving on
Without me.
So maybe instead you should just
Keep the motor running,
Let me hop out for just a moment.
While you’re not looking
I might just try to run.
But I realize you’re not paying attention any more…
I’m taking too long,
So I will linger a while,
Taking in the glory,
Before the last breath.
September 12th, 2014 §
 Hi everyone, a quick update before the weekend…
Hi everyone, a quick update before the weekend…
It’s been a really tough few days after the increased dose of Carboplatin with my Gemzar infusion. Every side effect has come out of the woodwork and I’m doing my best to sleep off as much as I can while still doing the necessary daily activities. I went to one Back to School night this week and hope to attend two more soon. Next week will be chemo again (Gemzar only) and then a transfusion a few days later. I’ll also get a Neulasta shot next week and my usual Xgeva shot as well. That will be a rough week.
It’s too soon to know if the higher dose of chemo is doing anything at this point, so I am just forging ahead. We should know more in the next few weeks. Until then we continue to think about what option makes the most sense to try next.
Terry Teachout featured me in a touching piece he wrote in The Wall Street Journal yesterday called “Mortality and Muse” about those of us who choose to write about unpleasant subjects. He honored me in his support and I wanted to share it with you. To read it click here.
Here, too, is a link to the YouTube video from a panel session at Stanford MedX this month entitled “Communicating the Experience of Illness in the Digital Age.” Towards the end (around 30 minutes in) they directly address my story but anyone who wants to hear more about the topic can watch the panel session. Thank you to Susannah Fox, Colleen Young, and Meredith Gould for addressing some of the real issues and challenges of individuals who choose to share their health stories online.
Autumn is in the air here and I hope wherever you are you are able to find a bit of beauty for the weekend. I will be doing just that.
September 8th, 2014 §
 I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
I am writing this on Monday night; by the time email subscribers read this it will be Tuesday and I’ll be done with chemotherapy again, having risen before dawn to head down to New York’s Memorial Sloan-Kettering
First let me report the good things. I have had some great days after my transfusion last week for severe anemia (expected often now after this much chemo).
On Friday night I drove Colin in heavy traffic to his first travel baseball game (took two hours). Then I sat watching warmup and the game which was another 3.5 hours. Then an hour home. I am detailing that time to brag. Look what I did with my son.
It wasn’t physically easy for me. But it was joyous. We got so punchy in the traffic jam that we were waving our hands in the air “seat dancing” to the music. We nicknamed a car “Duck Dynasty” that was broken down by the side of the road and then got lost at the venue and ended up 4-wheeling over gravel hills. We had a blast. Here is my precious middle child when we arrived at the field. The team won which was exciting. It was his first game on a full-sized field and also under the lights. I also got to take him  to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
to another game on Sunday; the team lost that one but it didn’t much matter to me. I got to not only be there to cheer the boys on, but also bring them water and popsicles on a scorcher of a day on the field.
The medical update since the last post is that in short, there isn’t a good clinical trial that I qualify for/am willing to enroll in right now. The chemo regimen that I am on makes me ineligible for some because it affects my blood counts so severely each time now (quite a catch-22, I would need to go off chemo to even have a chance at being considered). One trial I can’t be considered for because there isn’t enough tissue left from a previous biopsy to use it for required testing. Because my cancer is primarily in bones or other places inaccessible by surgery, this is not an easy problem to fix.
Now I’m going to get a bit technical. I’m hoping to explain a bit about how the different clinical trial types work since many people don’t know these distinctions. Consider this your breast cancer education for the week! Yeah, you know I’m not a doctor so I’m explaining this to the best of my ability. Ask a doctor for more info, especially one who works in clinical trials to be sure the trials you or a loved one might be considering work the same way.
Here we go:
One type of Phase I clinical trial (which I would qualify for) is risky enough that this option isn’t reasonable to me right now. Let me clearly state that they may become very reasonable options at some point soon and I totally understand why other people choose to do them! These particular phase 1 trials I’m opting out of for the time being are the kind that are testing safety of a medication previously untested in humans. That is, they don’t yet even have a dose that they know is safe. They are called “dose escalation Phase I trials” which means they start with a low dose they think is safe and gradually increase the dose until the side effects become too bad and the test subjects can’t continue and they stop participating. They do these on a small number of people.
This process establishes the maximum tolerable dose and the company hopes to then proceed to a Phase II trial. That Phase II trial tests if that established maximum tolerable dose even does anything measurable (Phase II trials test for efficacy: is this drug keeping the cancer stable or even causing it to shrink?).
To complete the clinical trial trio, a Phase III trial tests the “current standard of care” plus the trial drug against the current standard of care alone. That is, does adding this drug to a treatment that is a normal one for this cancer improve outcomes above and beyond just giving the treatment the patient would normally get (are results better? The same? Worse?). For ethical reasons there are no placebos used alone instead of treatment in Phase III trials in metastatic breast cancer. They would be used only to combine with the standard of care treatment. No patient goes untreated. All get the usual treatment as the guarantee.
This process means that during the Phase I dose escalation trial I first mentioned 1) you don’t know if the trial drug is safe, 2) you don’t know if that dose is too low for some or all of that time to even be doing anything, even if it is eventually going to be efficacious, and/or 3) if it even works at any dose (without making things worse). This means continuing with your cancer potentially untreated for months, an often dangerous proposition in metastatic cancer.
I don’t want to go into more details of those trials but I do think it’s important for me to continue to explain the way that some clinical trials work with metastatic breast cancer.
As I think I mentioned in my last post, the likely immediate plan was to increase the dose of one or both of my current chemo drugs. Because I opted not to pursue enrolling in a clinical trial I will remain on IV chemo. If I had chosen the trial I would need an additional two weeks without any chemotherapy to complete the mandatory washout period where I do not use any medications to treat the cancer because their presence in my body could affect the trial drug results or side effects.
I am going in for an increased dose of Carboplatin and steady dose of Gemzar on Tuesday. I did have one increase already in the Spring on my Gemzar dose. We will see what kind of response we can get from this Carboplatin increase, if any. It will hopefully buy us some time until some other trials open up and/or we can consider if we can do a biopsy once we see a current CT scan.
A few readers were concerned that I was relying too heavily on tumor markers in my decision-making. In short, I’m not. I am well aware (as I’ve said in almost every post except last time) that markers, particularly CA 15-3, are not reliable for many people. This is why this test is not used as a screening test for people to find out if they have breast cancer. If it were valid they would use it instead of or in conjunction with routine mammograms.
I know many doctors don’t use blood tests for markers at all and for some types of breast cancer they are totally worthless. Trust me, oncologists at Sloan-Kettering are well aware of all of this information as am I. The most important piece of information is a history of them in me and how they correlate with scans and my disease progression. I am one of the people for whom they are tightly and reliably correlated with my disease. We have had seven years of studying them in my particular case and two years with close monitoring during metastatic disease. So while I definitely appreciate the concern, you can rest assured that we make decisions with all of this in mind. It was my error in not putting that usual caveat in that last post.
So… for now the plan is: higher dose of one of two chemo agents on Tuesday. Test markers to see what they’ve done in last few weeks.
In case you are curious, going for chemo doesn’t just mean getting two drugs. The infusions I will get on Tuesday are numerous. I will get the following 8 infusions in this order: Decadron (helps with nausea and mainly to help prevent an anaphylactic reaction to Carboplatin because I’ve had more than 6 infusions), Pepcid (helps with anaphylaxis prevention and also bonus heartburn help), Benadryl (helps prevent anaphylaxis), Carboplatin (chemo agent #1), 1 liter fluids (helps prevent dehydration and bonus helps to keep kidneys functioning well to avoid high creatinine levels that can be dangerous), Aloxi (anti-nausea, blocks signals from stomach), Gemcitabine (chemo agent #2), Emend (blocks nausea and vomiting signals from the brain).
Away I go… thanks for the support. These days of uncertainty are difficult for me. I like a plan.We have a short term one and I am, as always, moving forward. As I wrote in a prior post and re-read tonight:
Cellular biology is King.
But paired to that fateful ruler
I shall be an argumentative, rebellious Queen.
Wring the most out of each day.
Find those bits of joy and beauty,
Make sure that what I’m doing isn’t waiting around to die.
For truly, that would be a waste.
August 28th, 2014 §
 The last week has been stressful. Unfortunately, my bloodwork shows that the chemotherapy regimen of Carboplatin and Gemzar is losing its effectiveness. It’s time to start looking at options for what to do next.
The last week has been stressful. Unfortunately, my bloodwork shows that the chemotherapy regimen of Carboplatin and Gemzar is losing its effectiveness. It’s time to start looking at options for what to do next.
We watch my tumor markers very closely and check them each chemo cycle (every three weeks). Once there is evidence of an increase in the marker number, my oncologist and I start to construct “if/then” decision trees. I know from earlier this year how fast metastatic breast cancer can spiral out of control. I don’t want to have that happen again if I can avoid it.
There is no guarantee that any given treatment will work. Many chemotherapies won’t work at all. One that works in 50% of cases is considered a great option. If they do work, they won’t keep working. The cancer will mutate, become resistant. We seem to be there again.
There are options to consider: clinical trials, chemotherapy, targeted therapies. Clinical trials are becoming harder for me to qualify for because I have already received too many different chemotherapy drugs. Most of the trials for metastatic breast cancer patients limit the number of chemotherapy agents to two. I’ve already had Xeloda, Taxol, Carbo and Gemzar. I simply can’t be considered for most of these trials.
At this point we are exploring a few options and using the next few weeks to investigate what trials are currently open and enrolling patients (they often take batches of new patients in clusters). The main issue, however, is if they are trials I actually am interested in. I need to look at the science behind each one and try to balance the risk of trying it versus other treatment options. Enrolling in a trial means having a “washout period” with the patient receiving no treatment at all (usually 3-4 weeks) before starting the protocol. This can be a precarious position to put yourself in if you have already been on a treatment that has become ineffective.
So where are things for the immediate future? For now our plan is to go through one more round of this chemo combination but do it at a higher dose and see if we can get either a response or stability at least. That will buy us a few weeks to gather information on what trials are available and what we want to do.
As far as my update for the week, I had chemo on Tuesday and I needed another shot of Neulasta yesterday to boost my white count and thereby restore my infection-fighting capability. The chemo now knocks that down every time and I can’t recover on my own. Once again I will need a transfusion of red blood cells tomorrow because my hemoglobin level is too low. When this happens I don’t have enough oxygen-carrying capability in my blood to allow me to function normally. I get short of breath just walking or standing. This is a predictable part of some types of chemotherapy if you are on them long enough. After enough cycles of constant chemo the body just can’t compensate for what is killed in the collateral damage of treatment. Not all chemos do this, but mine does.
So the news is not what we want. It’s hard to hear. This chemo combination did a great job at shrinking many lesions in a short time. I am functioning in a much better place than I was this Spring, but now I worry that things will progress quickly before we find something new that works. I wonder what will work. I wonder how long it will take to find it, and what kind of shape I will be in when we do. If we do. At this point there are enough options that I do still think it’s when, not if. But this day has come sooner than I’d hoped.
August 22nd, 2014 §
 Grow up faster,
Grow up faster,
Need me less,
Reach the sky,
Stand up tall.
Make time go,
Speed it up,
Get it done,
Don’t look back.
Hear my voice,
Feel my embrace,
Know I tried,
Look straight ahead.
Keep forging,
Thinking,
Feeling.
There is no choice,
This world is all there is,
Make it last.
Ours will be far shorter a time than it should be:
Years compressed into months, days, hours, minutes.
It will never be long enough,
It simply could never be enough time with you.
August 17th, 2014 §
 My most recent round of chemo almost three weeks ago fell on my 45th birthday. I didn’t reschedule the appointment; I got up at 5 A.M. as planned and spent the day going to Sloan-Kettering getting my 7th Carboplatin and 14th Gemzar infusions. It seemed a fitting way to spend the day, doing what I can to see as many more birthdays as possible.
My most recent round of chemo almost three weeks ago fell on my 45th birthday. I didn’t reschedule the appointment; I got up at 5 A.M. as planned and spent the day going to Sloan-Kettering getting my 7th Carboplatin and 14th Gemzar infusions. It seemed a fitting way to spend the day, doing what I can to see as many more birthdays as possible.
Thank you to those who donated to my fund for research on metastatic breast cancer at Sloan-Kettering in honor of my birthday, I so greatly appreciate it.
My blood counts finally are having trouble rebounding between the constant hits. The blood draw that they do to check my counts before chemo showed that my white count and ANC were the lowest we’ve seen this year (this means the patient is dangerously susceptible to infection). Chemo is sometimes postponed under these conditions but we opted to proceed. Twenty-four hours after chemo I received a shot of Neulasta to spur my bone marrow to make more white cells.
This type of injection often causes intense bone pain for days afterward. A three day regimen of over-the-counter Claritin (night before injection, night of injection, and one more the night after) seems to help many people with this pain. I did the Claritin and did well after (though I tolerated them well when I had them 7 years ago). If you suffer from terrible bone pain after Neulasta shots it might be something to ask your oncologist about. I learned about it from the nurses on my team.
My red blood cell count also took a hit the following week after chemo. I needed to get another blood transfusion. I’ll need Neulasta and blood transfusions more frequently now as the cumulative toll of this chemotherapy is taking effect. Muscle pain increased significantly this cycle as well. For days I was unable to bend over to even pick something off the floor. I couldn’t walk more than a few steps or leave the house. I’ll be meeting with my palliative care doctor on Tuesday to try to get some ideas on the best things to do for this new development. I’ll take this opportunity to remind you that palliative care does not equal hospice care. It is NOT for end of life care only. Palliative care is supportive care. The specialists help with all side effects at any stage of diagnosis/treatment.
Every day brings something new. It’s definitely getting more challenging in some of these ways but the good days are so grand to have.
School is going to start in another week and on the good days I am busy taking the kids to buy all of the things they need to start the year. It’s nice to be able to do some of these traditional August things with them. I treasure the most mundane activities of buying a new baseball glove, picking up school supplies, getting the back-to-school haircuts.
On Tuesday I will be back again for cycle 8 of Carbo/Gemzar; there won’t be a family summer trip. It’s been tough to see all of the photos online of everyone’s trips and summer fun and adventures. Cancer is a thief, stealing the carefree week my family and I should have had.
I always think these medical updates must be rather boring to read, I confess I hesitate to write them. I will probably start sharing more frequent quick updates on my blog Facebook page for those who are interested.
I’ll leave you with a few photos that make me smile. One is a new one with my beloved medical oncologist, Dr. Chau Dang (on my birthday). I couldn’t do this without her leading the team that treats me. The next one is part of my front garden in bloom last week. One is of our corgi, Lucy, who keeps me company on these housebound days.



And something I wrote a while ago that I read almost every morning:
Make the most of this day. Whatever that means to you, whatever you can do. No matter how small it seems to you. Don’t waste it.
I hope you all have a good week and I hope to have a post about resilience coming soon…
August 4th, 2014 §
 They were already seated when we arrived, a sea of white sitting cramped.
They were already seated when we arrived, a sea of white sitting cramped.
Mostly couples, though some were in girl groups.
They didn’t rise when we needed to pass by.
Clearly that effort would be too much.
I know how that feels.
Almost all wore glasses, most eventually pulled out bags of snacks or sucking candies.
No one texted or emailed or checked the time on a phone.
They all had small watches on their wrists for that.
In front of me a man had a bandage on the top of his head, white gauze perched amidst his silver hair, a good head of it.
I decided a funny looking mole, irregular in shape, had lain there recently; his wife pressed him to go see the dermatologist to have it checked.
The two looked out for each other, you see, having been together so long.
The air was still and thick and choked me as the minutes wore on.
I could see the veins protruding on the back of their hands, the wrinkles, the hunched shoulders.
We were the youngest there.
And while I felt more like them in many ways, closer to the end than to the beginning, I realize I am an outsider in every group.
There are few like me.
My hair won’t get that white, you see,
My hands won’t be rewarded with that saggy skin.
I won’t be privileged enough to see him go bald.
It will always be “in sickness” now.
The lights finally went down and I tried to forget.
But my body and mind do not ever let me.
How jealous I was of those elderly people crowded into a movie theater on an August Sunday afternoon.
July 9th, 2014 §
 Now that all three of our children are at sleep away camp I get asked a lot “what I’m doing with all of my free time” and “what fun things I have planned.” Clearly what people think life is like for me are a bit skewed. I have nothing planned. I can’t travel and haven’t been able to take a trip for over a year. I’ve missed family celebrations, holidays, and get-togethers. I’ve eschewed visits from family and friends because I’m not well enough. What others consider “free time” is recovery from chemotherapy and struggling to do day-to-day functioning including the many medical appointments. Being able to make it out for a coffee date is a thrill and isn’t possible many days. Most of the rest of the time my “free time” is spent in bed fighting nausea or fatigue or pain or other side effects.
Now that all three of our children are at sleep away camp I get asked a lot “what I’m doing with all of my free time” and “what fun things I have planned.” Clearly what people think life is like for me are a bit skewed. I have nothing planned. I can’t travel and haven’t been able to take a trip for over a year. I’ve missed family celebrations, holidays, and get-togethers. I’ve eschewed visits from family and friends because I’m not well enough. What others consider “free time” is recovery from chemotherapy and struggling to do day-to-day functioning including the many medical appointments. Being able to make it out for a coffee date is a thrill and isn’t possible many days. Most of the rest of the time my “free time” is spent in bed fighting nausea or fatigue or pain or other side effects.
For the last few weeks my blood counts were sliding and I couldn’t do anything without huffing and puffing in a much more severe way than usual. I struggled to bend over to pick something off the floor without needing to sit down to catch my breath. My hemoglobin levels had been hovering around 8.2 for months and I pushed through but they dropped to 7.2 and by then it seemed I needed a boost to be functional. Ten days ago I received two units of red cells in a transfusion that because of some problems with the samples and testing and a five hour infusion ended up being a ten hour marathon day. It was so worth it. Red counts came up within days and I felt better starting about 24 hours after receiving the cells and that continued to increase within two to three days. My platelets were also very low at 24 but regenerated on their own (low platelets are a predictable result of this chemo regimen) and I was able to avoid a transfusion of those. This was, by the way, the first time I had ever had a blood transfusion in my life.
I had chemo yesterday: Carboplatin and Gemzar cycle #6 (that means I’ve had 6 infusions of Carboplatin and 11 of Gemzar so far). Starting now, but especially with cycle 7 and every time after that, there is a risk (reported at 27% for round 7, here is an article for anyone interested) of an anaphylactic reaction to the Carboplatin (and the other platinum-based chemotherapies like it). We are being conservative and premedicating with drugs that will hopefully help blunt or avoid this type of reaction altogether. There isn’t any reliable way to predict if it will happen to any individual patient. I did have a reaction to Taxol when I received it in the metastatic setting (after not having a reaction the first time I had 4 cycles of it seven years ago) but that is not a reliable indicator of a reaction to platinum-baed drugs.
It will be time for a scan soon I think, we are watching my tumor markers which have dropped consistently in the last few months which is fantastic but on yesterday’s test just stabilized without a drop. We’ll have to see if this is just stabilization (fine) or if this is the start of the chemo losing its effect. It is unsettling to think about losing another chemo combination that has been working, even though it’s a tough regimen to tolerate.
My voice has returned to almost normal unless I use it on the phone or talk a lot. With the kids gone I really am not talking much. I had an extra five days off chemo because my oncologist was on vacation and that allowed me to get things done I usually don’t have enough rebound time to do. The transfusion timing helped too.
 I haven’t been outside much, the humidity and heat have been too oppressive for me, but I am hopeful it will break soon. I do try to make it to the beach once a week to get a change of scenery.
I haven’t been outside much, the humidity and heat have been too oppressive for me, but I am hopeful it will break soon. I do try to make it to the beach once a week to get a change of scenery.
We will get to see the kids this weekend and I can’t wait to hug them and hear all of their stories before they go back. They love camp, always have. They look forward to it year-round and now that they all go it’s great they can share these stories and experiences (they are 15, 12, and 8. Last year the youngest begged to go for a week to try it out. We said yes, knowing his siblings would be there and he would have a blast. Five days in he called in tears, begging to stay. That repeated every week until after a month we said it was time to come home!).
Some may wonder why, at this time, I let them go instead of keeping them home with me. I do it because it’s not about me. It’s about them. It’s something they love. It’s an important routine, tradition (this is the sixth year for the oldest). In my eyes, it’s important that they have a change of scenery, freedom to be kids, get away from the ways my cancer and its chronic treatment limit what I can do, and therefore what they can do. It’s a gift I can give them and I also feel it reassures them that I am doing better than I was a few months ago. This is important.
 I love having them away from electronics, away from wondering if asking me to take them somewhere or do something with them will be “too much” or “bothering me” which I know the older ones are always concerned with. I want them to be with friends old and new, having fun with young and energetic counselors, trying new things. There are so many (most/all) physical activities I cannot do with them that they can do there. So many new games to play, achievements, laughs, experiences. I never hesitated when they were ready to sign up last October for this summer. I knew that no matter what, they needed and deserved it. On the left is my favorite photo from camp so far: Tristan getting hooked in to try rock wall climbing for the first time. It makes me laugh every time I look at that facial expression!
I love having them away from electronics, away from wondering if asking me to take them somewhere or do something with them will be “too much” or “bothering me” which I know the older ones are always concerned with. I want them to be with friends old and new, having fun with young and energetic counselors, trying new things. There are so many (most/all) physical activities I cannot do with them that they can do there. So many new games to play, achievements, laughs, experiences. I never hesitated when they were ready to sign up last October for this summer. I knew that no matter what, they needed and deserved it. On the left is my favorite photo from camp so far: Tristan getting hooked in to try rock wall climbing for the first time. It makes me laugh every time I look at that facial expression!
That doesn’t mean it’s easy for us to be apart. We are very close. Especially the older kids worry about me I am sure. But I stay in touch by email, will see them on visiting days, and I send them weekly care packages.
But the truth is that separation is good. It’s a selfless act for me to teach them how to to be without me. One of the most important things, in my mind. Coddling them and making them stay home is not what I feel is best for them right now. It is part of our job as parents to teach our children how to be independent, how to solve problems on their own, how to go off in the world without us for whatever reason. I will always want more time with them. It will never be enough for me. But this is my old age. I must teach them as many lessons as I can, while I can, for as long as I can. And that is true for everyone, but of course I have not only the urgency to do it NOW but also I have no idea how long I have and will likely be debilitated in some form until that time comes.
Yes, it’s true no one knows how long they have to live. But those diagnosed with a terminal disease know what is most likely to kill them. And that their time is not just going to be shortened, but consumed daily with the treatment and effects of that disease. It’s not having a normal, healthy life that is relatively good and healthy until a sudden accident happens. It’s just not the same as the general worries of growing older or aches and pains. It’s never-ending. I don’t get to count down how many chemotherapy (or other treatment) sessions until I’m done this time. Being done will mean there is nothing left for me to try. Anyone who has had chemo or radiation or some other type of therapy knows how important it is to have an endpoint, a countdown. Knowing that will never happen (and in fact what you’re really hoping for is a lot of them, because that means you still have options) is one of the mental struggles each week, since it isn’t just spending one day a week getting chemo, it’s how it makes you feel each day after that.
My hair is growing slowly back on this current combo. I know many people mistakenly think this means I’m “better.” I do like that soon I won’t be covering my head and that means I can be more invisible in public. But I also know how many comments I get on the occasions I have done it that people think I am done with chemo or all better. Not all chemotherapies cause hair to come out. My hair will come and go numerous times by the time we are done with this. Its presence or absence only indicates something about which chemo I’m on, not its success or failure.
Someone on Twitter asked for my piece on what to say and how to be a friend to someone who has cancer/serious illness. Here is a link for anyone that missed it and is interested (it’s too long to include the text in this post).
Also, I am including two posts from last year at this time. One on the eve of the kids’ departure for camp and one written while they were away. Of course I was doing even better than I am now, my thoughts were similar, but not as urgent, strong, painful as they have been the last seven months.
I’ll post again with an update if there is anything to report on change in treatment, scan results, etc. For now we stay the course which is not easy, but is the best possible choice of the options I have right now. And that’s the best I can do.
I appreciate the support, as always!
…………………………………………….
In these last remaining hours (Camp) original post here
In these last remaining hours
Before my children disappear
One,
Two,
Three…
In these last remaining hours before they go and spread their wings again,
Leave this nest,
I miss them already.
I put the dinner pots and pans away.
Wipe the crumbs from the table,
Load the dishwasher,
Play fetch with the dog.
I sit in the garden,
Listen to the wind in the trees,
The birds settling down before nightfall,
As we settle, too.
I tuck them in one last time,
Hear their doors click shut.
One,
Two,
Three.
Tomorrow night there will be no mess to clean,
No yelling upstairs that the TV has been left on again,
No trunks piled high with carefully labeled belongings in the dining room.
I will cry, I know.
Not because I am sad that they are going– no, that gives me great joy.
Children being children.
Forgetting stress at home and doing new and varied things.
I cheer their independence.
I will cry because I know they will always need me somehow and I just wish I could be there for them to outgrow
by choice,
by time,
by age.
I hear the mother bird in the tree calling out.
I don’t know to whom.
I will be like that tomorrow,
calling out,
with no child to hear.
……………………………………………………….
Like dollhouse rooms left abandoned (original post here)
Like dollhouse rooms left abandoned,
The rooms stay tidy:
Beds made tight,
Pillows square,
Hampers empty.
It’s been one week since the children left for camp.
Littlest Tristan was due back yesterday but a few days ago he said he was having so much fun he wanted to stay another week.
I realized this week that after being sick for the previous two that I needed this time to catch up, to rest, to regroup.
I miss them but am so glad they are having fun doing what they love.
I pack up care packages,
write letters,
wake in the middle of the night and mentally picture our children sleeping in cabin beds.
Our dog Lucy follows me, sleeps in my room now, not Paige’s.
She doesn’t want to be alone and stays within feet of me every moment.
I tell her it’s okay:
The kids will come back.
The rooms will get messy again.
There will be crumbs dropped at the dinner table and car rides galore.
Paige and Colin and Tristan will come back tired and dirty and happy.
They will come back.
They will.
That is the key.
I think of absence like a hole:
How different it is when it’s temporary and filled with happiness,
Rather than when that hole is a pit of grief. Of ache. Of loss.
The way it will someday be for them.
June 12th, 2014 §
 You have all been so patient with me, understanding why I haven’t been able to update as often as I was doing previously. I’m hoping my report will be worth the wait.
You have all been so patient with me, understanding why I haven’t been able to update as often as I was doing previously. I’m hoping my report will be worth the wait.
Let’s cut to the chase with some good news: there is no doubt about it, I am on my 5th cycle of Carboplatin and Gemzar and these chemo agents are effectively reducing the overall amount of cancer in my body (my recent previous chemos were not).
So, the cautionary notes are that the chemo will eventually fail; the cancer will either become resistant or I will lose tolerance for it because of side effects or hypersensitivity as the doses go on and the cumulative totals of the drug I’ve been exposed to rise over time. This is a problem that happens with only some chemo drugs; Carboplatin happens to be one. As you may remember, I am trying to ride carbo’s work as long as I can, it’s not for a finite number of sessions. With metastatic breast cancer you must be on some form of chemo/targeted therapy for the rest of your life if you choose to treat it. So this isn’t a permanent fix.
Additionally, I am right on the cusp (my next cycle) of when I will be most at risk for reactions to the Carboplatin. The other drug, Gemzar, is easier to tolerate in general and doesn’t have this same hypersensitivity issue. Of course we don’t know for sure which chemo is doing the bulk of the work here. Ideally we keep them both.
My tumor markers have all consistently been dropping for last 6 weeks and in my particular case, these markers have always been closely correlated with what scans and clinical signs show (many with breast cancer do not have this correlation, you must know your own case; this is one reason why these blood tests cannot be used as tools to screen for breast cancer or metastases reliably).
What does it mean that my markers are dropping? The numbers are going down significantly, indicating that the chemo is working, something I anticipated because I have been feeling much better in last month. “Better” is relative of course. What is “good” or even “great” for me might be someone healthy saying it was one of their worst days I bet! But what is important is that it’s moving in the right direction. My issues now are more chemo-related (fatigue, weakness, blood counts, infections, shortness of breath, etc.) than cancer-related.
My voice has improved! There is no doubt. I am still raspy and if I talk for a while or have to strain to use it, it deteriorates rapidly. But it is such a change. I can swallow more easily which makes getting needed fluid and swallowing pills easier. I no longer need to go for added IV hydration, I am able now to do it in conjunction with chemo.
 I can get out more for limited times on certain days. Some days this is impossible because of chemo. And I institute a “no hugging” policy for friends during times I know I’m especially susceptible to infection. I’ve made it to the beach a few times, to more special events for the kids, and for the first time this week could stand long enough to fold some laundry. I am still very weak and incapacitated on many days. But now my “off week” from chemo is better.
I can get out more for limited times on certain days. Some days this is impossible because of chemo. And I institute a “no hugging” policy for friends during times I know I’m especially susceptible to infection. I’ve made it to the beach a few times, to more special events for the kids, and for the first time this week could stand long enough to fold some laundry. I am still very weak and incapacitated on many days. But now my “off week” from chemo is better.
Just because people see me in public they shouldn’t assume that I’m “back to normal” or “feeling great.” It is hard to explain that it might have taken me all day to get the energy up to do that one errand or have that one coffee date with a friend, that I’ll need a nap and to rest for the rest of the day after doing it. They might not understand that I was in bed for days leading up to it or will get chemo the next day and not be well for a while. I still have metastatic breast cancer throughout my body, and it takes a hefty toll. Hopefully explaining some of these details can help people to understand a bit what daily life is like for me.
I’m enjoying my garden in bloom and have been taking photos and posting this month on Twitter/Instagram. I’ll be using them with my posts all summer. Every one is taken by me of something in my yard. Today’s are of my beloved Japanese peony, a single petal peony I planted from barefoot years ago. This year it only had three flowers but they were so gorgeous. It’s hard to believe the closeup is of a flower! I think it looks like a sea anemone (some have said it looks like french fries).
So, the takeaway: I’m moving in the right direction for now, for what my particular case of metastatic breast cancer is. Despite many headlines about advances in breast cancer treatments lately, there was NOTHING relevant to me coming out of the big national ASCO conference last month and a good source tells me there really won’t be anything coming out of the San Antonio breast conference for me, either (the few relevant trials just haven’t been going on long enough to have any preliminary results yet). I’m keeping on top of new trials, as is my team, and if there is something that comes up that looks good, we’ll be investigating. For now, for as long as I can, I stay the course on this chemo regimen whether it’s for one month more or eight.
I will try to write more often. I know it’s a bit concerning when long times go by and someone with a serious illness doesn’t post. That only goes to show you how utterly rotten I have felt for a very long time. It has taken seven months (seven months!) to get to this point. I don’t take that for granted. Some with my diagnosis are dead within that time.
It’s so nice to be able to report some good news. It sure does feel like an awfully long time since I’ve been able to do that.
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
April 27th, 2014 §
 It’s been a long time since my last update. The weeks have been very tough and I haven’t had the energy to do much of anything, much less update the blog. I have switched chemotherapy agents to Carboplatin and Gemzar. These are given in a bit of an unusual schedule: both drugs the first week, just Gemzar the second week, and then a week off to allow blood counts to rise back to (hopefully) normal levels. I will be starting my third cycle this week.
It’s been a long time since my last update. The weeks have been very tough and I haven’t had the energy to do much of anything, much less update the blog. I have switched chemotherapy agents to Carboplatin and Gemzar. These are given in a bit of an unusual schedule: both drugs the first week, just Gemzar the second week, and then a week off to allow blood counts to rise back to (hopefully) normal levels. I will be starting my third cycle this week.
I’ve had tremendous fatigue and the palliative team is trying some medication to hopefully help with this. There still may be effects from radiation weakening me (fatigue from high doses of radiation like I received to my spine and pelvis can last up to six months they say) and of course when certain blood counts drop it makes you feel just tired and rotten. I fervently hope that the medication will help and I will be gaining some strength and energy soon. It’s been such a long few months. Good news is that radiation did such a great job on the two areas that I’ve been able to completely wean off of pain medication. The pain I have from the current tumors throughout my body does not require medication right now. I know that will change as those tumors grow, but the gradual weaning process I have been doing for the past 3 months has been a huge success and I’m so glad to see the vertigo and other side effects from the pain meds disappear.
On the flip side, while the pain component has been a success, the last few weeks have been fraught with some unexpected problems. For the last month I’ve been seeing specialists and having tests to figure out why my voice has completely deteriorated and I also developed a varying left eye droop and lack of dilation in the left eye.
After a brain MRI to rule out a brain metastasis the doctors have determined that it is actually a malignant lesion in my left chest causing Horner’s Syndrome in my eye. The lesion is also pressing on the nerve cluster that controls my left vocal chord. It’s not totally paralyzed yet, but they say that it is on its way. My voice is almost completely unusable in any situation with noise (ordering in a restaurant is impossible, being heard on the phone is difficult, etc.). I can get out a strong whisper to a quiet raspy voice for about ten to twenty minutes in the morning sometimes but communication outside the quiet house or after twenty minutes is very, very hard.
I already do know there are things like voice magnifiers or computer generated voices. I know they are out there but I am not ready to use them. The damage will almost certainly be permanent they tell me. Swallowing will become more difficult and dangerous as the chord deteriorates. There is an injection they can do to stiffen the chord but at this point they are not ready to do that because I won’t get any additional improvement over where I am now.
The lack of voice limits further the amount of social contact I can have these days and the energy it takes to communicate is magnified because breath control is reduced so much. I will go back in three months and we will re-evaluate. Even my voice isn’t off limits to cancer it seems. I really just feel a period of stability would be so welcomed.
The rest of my family went to Florida for Spring Break two weeks ago while I had my tough week of chemo and some appointments with specialists. I was so glad they could go get some sunshine and respite from the stress that I know my situation brings. It is so important to me to try to always look at things from their point of view and know what this situation asks from them. I wish I could be a better wife and mother right now, but wishes don’t count for much I know. It was hard to miss yet another family trip, there have been a few this year.
I try to get out once a day but I tire easily and usually am not able to get out on chemo weeks (more than 2/3 of days). Walking and standing are still my challenges. I continue to be very isolated. My daily life of exhaustion, immunosuppression, chemotherapy, and treatment effects keep me chained to cancer, much as I hate to be. I try to be as independent as I can, not ask for help often, and keep my thoughts to myself about what is happening and what is yet to come.
For now, I keep plugging away, hoping the new chemo is continuing to work and doing the best I can even when things seem stacked against me. My medical team continues to be warm, caring, and helpful and I am so grateful to them and to you.
Things are very hard right now. It takes all of the strength I have to get through each day doing things I otherwise would be giving little thought to. I miss that part, the carefree, energetic part of me I had.
For now, I just keep going, doing my best. It just is going to have to be good enough. Spring has been lagging, the garden isn’t flowering as it usually is. The days have been chilly and nights sometimes still have freeze warnings. Let’s hope by my next update the flowers and I are both blooming a bit more.
March 25th, 2014 §
 It’s been such a rough few weeks. I’m going to keep this short. I’ve wanted to update and haven’t been able to… you know that means it’s been tough.
It’s been such a rough few weeks. I’m going to keep this short. I’ve wanted to update and haven’t been able to… you know that means it’s been tough.
I’ve switched chemo. Taxol wasn’t doing what it should/had hoped. So we have changed plans.
Last week I started a three week course of Carboplatin and Gemzar (both drugs are given the first week, just Gemzar the second week, third week is a break week in my particular plan). We may have to modify this because the fatigue and steroid crash have been giving me a really hard time.
Taxol wasn’t doing a great job but the scans show that radiation did a good job on the tumors in my spine and hips. There are others that we are watching in bones and will monitor them. Now we also go to work on liver tumors and when they shrink down we will radiate (ablate) those. It’s always like Whack-a-Mole. Something drops down and something pops up. You try until you find something that works.
I still have problems with my esophagus from the radiation. Each chemo session aggravates it and it gets hard to talk. Thankfully it’s not too painful. But it does flare each week and means no talking on phone and not much in person. It does affect eating as well.
I haven’t been able to be out much at all, just a few times in the last few month, usually on days when steroids are giving me a boost or I need to be at a doctor’s office for fluids to prevent dehydration. I’m sleeping a lot… sometimes for literally days at a time and trying to let my body work through this. There’s no other choice. I wish I could be doing more with my family. But I hope they know I am doing the best I can, admittedly not so much right now.
I can’t truly explain how debilitating the feeling is: needing a nap after a shower, sleeping for most of the day and then sleeping right through the night, trying to decide how many times it’s manageable to get up to go to the bathroom. But we will keep working to find a way to get through it. The radiation with chemo right on its heels is still knocking me back even months later, as are ongoing chemo treatments.
I’m so grateful for the rides, help from friends, and delivered meals that keep things going. I couldn’t do it without the friends that drive the kids to school and bus stop daily, take me to doctors’ appointments on the spur of the moment for IV fluids, and those who offer assorted favors. I need you more than you know and am grateful to those who offer. I am not answering most emails at this point but I do read them.
Thank you.
March 4th, 2014 §
 Hi everyone, an update to briefly say hello since my posts are still infrequent. It’s been about three months now since this particular acute metastatic breast cancer episode started. First I was stuck at home in pain with tumors in my spine and hips before and during the holidays. Then I was in the hospital for three weeks at the start of 2014 getting pain under control and having two weeks of radiation. Now I’ve been home for another six weeks since leaving the hospital.
Hi everyone, an update to briefly say hello since my posts are still infrequent. It’s been about three months now since this particular acute metastatic breast cancer episode started. First I was stuck at home in pain with tumors in my spine and hips before and during the holidays. Then I was in the hospital for three weeks at the start of 2014 getting pain under control and having two weeks of radiation. Now I’ve been home for another six weeks since leaving the hospital.
After such a long period of time many people will start to assume you “must be back to normal by now.” Each day they anxiously wait for news that someone “feels better.” It doesn’t work like that all the time, just the way with metastatic cancer you don’t “beat it.” A good day or two may come, but they are often followed by a bad one, or two, or three. Add chemo to the mix and you start to realize the good days are relative and elusive in incurable cancer. Support is always so appreciated as the days, weeks, months go by. It’s friendship for the duration.
There are many situations where isolation may be a real danger including examples of infertility, chronic illness, and grief. Those who must deal with these problems start to feel isolated. Additionally, they may start to actively separate from others when they feel that life is just moving on without them. As time goes on, they may hesitate to talk about their problems because they fear that friends will have grown weary of hearing about it/ still can’t relate to it. More and more, they keep these things to themselves. This leads both to further isolation and also the faulty notion from their friends that the person is “over it.”
The truth is that it’s very hard when difficult situations of all kinds linger. I think we all do better when tough times are brief. Being in one of these situations has shown me the depth to which this is the case.
Today I had to miss Tristan’s Spring music show at school. It broke my heart to tell him I couldn’t attend. They were able to videotape it and I know we will watch it together and have a special time doing that. If it were just one thing it would be different. But as any parent can imagine, saying, “I’m so sorry but I can’t…” again and again for months is difficult. The truth is that if I knew it were temporary it would be easier. But I know that there will be more and more things I can’t do with the kids. And that’s what weighs on me: this thing is part of a whole.
I tried driving last weekend but unfortunately, for now, the verdict is that I am still unable to do more than go to the bus stop at the end of the street if needed. So I continue to be housebound.
I’m working with my doctors to adjust my medications and try to manage the vertigo, sedation and pain. I am using less pain medicine (hooray) but unfortunately I still feel so rotten I sometimes can’t get out of bed and most often can’t go anywhere except to chemo. It is a cruel balance. This weekend I was stuck in bed for three days. It saddens me to lose so much time.
I still long to write here more. I miss the creative part of my brain working the way it used to. I miss poetry and photography and so many things. I will bring them back though! The orchid photo above is one I took in the kitchen this week. My friend Alex brought me lunch and a beautiful potted orchid. I even ordered daffodils with my groceries this week to remind myself of the garden outside and what’s waiting under this snow.
Winter break at school came and went. I know it’s a very busy time for everyone as Spring approaches. It’s hard to see life outside passing me by while I wait for Spring so I can at least get fresh air here at home. It has continued to be cold and wintery over the past few weeks. If you’re able to be outside today doing anything: errands, standing at the bus stop, or waiting the train platform on your way to work: think for a moment what it would feel like not to do any of that for three months. It’s a very long time. Mundane things can be sweet when viewed in a different light.
I am so grateful for the offers of help and meals that continue to come. Let me assure you they are so needed and appreciated. I will have chemo again this week. In two weeks’ time the plan is to do scans to see if there is any visible evidence about whether radiation and chemo have shrunk the cancer.
My daily reminder: Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
In case you need a bit of beauty I will leave you with one of mine, a good laugh this week from Tristan. With a very serious expression on his face he says to me quietly from the dinner table, “Mom, I have something to tell you and you’re not going to like it. It’s something I learned. I was reading it in a book. But I think you will be upset. The book was about Albert Einstein. It said that for a while he didn’t want to go to school. He didn’t want to learn things in school that they wanted him to learn. He just wanted to learn what he wanted to learn. He stayed home for a while and didn’t go to school. See? I think you would not think that was very good that Albert Einstein didn’t want to go to school.”
February 23rd, 2014 §
 Sunday morning.
Sunday morning.
A different kind of strength: shave the few soft but strong hairs that are finally ready.
Now gone to the floor.
No tears.
Necessity.
……….
You’ll be seeing more posts here in the near future about some of my feelings over the last two months. I’m starting to feel more like myself. The vertigo is lessening with the decrease I’ve been able to make in the pain medication, as we’d hoped. I’ve reduced the pain meds by 20% and the hope is that as the radiation effects start to kick in I will be able to decrease more. It’s been five weeks now since I finished radiation. I needed these Fentanyl patches desperately while the tumors were out of control. I could not have done it any other way. But certainly we all want me only using the amount I need to control my current level of pain.
I will be going back to meet again with my palliative care doctors this week to reassess my pain meds and talk about the plan for the next few weeks. I was thrilled to see that my last post about the importance of early palliative care and its definition (not end-of-life pain management… but instead total patient care pain management) was so well-received by patients and doctors alike. I encourage both sides to really form a team and focus on all side effects that patients are having with all kinds of treatment.
Patients function better not only emotionally but also physically in that they will heal better if their bodies are not weakened by pain. It takes trial and error to find the right drugs and the right amounts. It takes patience. Most palliative care doctors are experts in patience, I have fortunately found. I know that is not always the case and I always receive emails and comments from people who have had distressing experiences with their care. I am so sorry for that. I am hoping by relaying my own experiences, readers who have not yet found help with pain will have strength to ask again or pursue help if they’ve been unable to.
I’ve started my second month of chemotherapy (Taxol). I do three weekly treatments in a row and then have one week off each month. I had my first infusion of my second month on Thursday. I haven’t had any additional reactions to the chemo so I’ve been able to have the sessions done rather quickly (30 minutes for the 3 pre-medications and then 60 minutes for the actual Taxol). Sometimes I go alone and sometimes I have a friend join me. I am developing a routine and it has worked well so far.
 We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
We still have a lot of snow on the ground and on sunny days like today the brightness is astounding. We are all anxious for Spring but it’s just not here yet (more snow due to arrive this week). I am thinking of my snowdrops and daffodils just waiting under the snow pack. The photo at left is from last year… can’t wait to see this in the front yard again soon.
For today I’m sporting a head scarf and getting used to seeing a new reflection looking back at me in the mirror.
………
Make the most of this day. Whatever that means to you, whatever you can do. No matter how small it seems to you. Don’t waste it.
February 7th, 2014 §
 It’s hard to believe how many days went by when I was in the hospital. It’s hard to believe how many days have gone by since I’ve been home.
It’s hard to believe how many days went by when I was in the hospital. It’s hard to believe how many days have gone by since I’ve been home.
I have wanted to write a blogpost so often. I sat down at the computer many times in the last few weeks to update you on what has been going on.
Most often what happened when I did that is simple: I got very tired and fell asleep. Sometimes my vertigo was really distracting. Sometimes the distraction was something wonderful: one of the kids wanted to tell me something. Frequently it was Tristan in his little voice saying, “I love you, Mama.” That one always takes priority, of course.
I’m on a lot of pain medication at the moment. I have been since leaving the hospital almost three weeks ago. The positive effects of radiation haven’t quite kicked in yet. I still have many of the negative effects of radiation. These will go away soon. But right now I’m still waiting. This is totally normal for radiation that is used in the way I used it, I should point out; it takes weeks, and in fact months, for the positive benefits of radiation to be fully realized. During that time the negative side effects of radiation can linger.
They radiated my spine in the T9/T10 areas from both the front and back and also radiated my pelvis through from the left and right sides for ten sessions over two weeks. The side effects that I have are related to the particular lines of radiation and what areas the beams hit while also hitting their targets. For me, esophagus, stomach, intestines, colon, pelvis, sacrum, and spine were the main areas hit. Esophagitis which makes eating and drinking painful is starting to decrease (but the raspy voice continues). Problems with digestion continue. Lowered blood counts continue. Pain and inflammation in nerves and tumor sites continue. Heartburn and colitis have decreased. I do not have radiation burns right now and they really didn’t get too bad over the course of those two weeks, just some sensitive pinkish/brownish areas.
The pain that was so debilitating is finally under control with pain patches. It takes quite a high dose to keep it managed right now but we will try decreasing this amount as the weeks go on. I will meet with the palliative care team in a few weeks to talk through a strategy for the reduction. The team is always available by phone for any fine tuning or questions that I have until that time.
Again I’d like to remind readers that palliative care is not synonymous with end-of-life care. Palliative care is for pain management and side effect management at any point of treatment for cancer or other diseases. If you have pain or other problems that are bothering you or a loved one, I encourage you to talk to the specialists in palliative care. They will be able to help.
Patients and their families often wait too long to consult with these specialists because they think talking to them implies something about death. It does not. In fact, if you wait too long (until the very end of life) the palliative team will probably be less likely to fully help you or your loved one because they won’t know how the patient responds to different medications, what their side effects are, what doses they respond to, etc. Palliative care doctors can help better if they know the patient and their particular side effect profile. I implore you to use them sooner rather than later. Time and again, studies have shown that healing occurs better when patients are not in pain.
We aren’t quite sure where it’s coming from, but my vertigo is quite the problem right now. We know it is from one of my medications, presumably the pain one. Of course for now I still need to make my pain medication the priority. As I said earlier, as soon as I can, I’ll be decreasing that dose. We know from a scan a few weeks ago that I do not have any metastases in my brain causing the vertigo. Of course that was a natural concern and it’s nice to have that possibility off the list. I still can’t drive because of the vertigo. So I’ve been housebound for the three weeks I’ve been home. Before that I was in the hospital for almost three weeks. I don’t have cabin fever too much because of the bad weather we have been having. But I’m probably getting close.
I’m still trying to figure things out. I’m still adjusting to the new information about the tumors and the progression that’s been happening in my body over the last few months. I’m learning about the genomic mutations that are present in the metastases and what they mean for future chemotherapy and clinical trial choices. I did not start the clinical trial I was planning to, obviously. Instead, we needed to do more aggressive and surefire treatments rather than investigational. Therefore, I did the radiation and then started chemotherapy 5 days after the completion of radiation (a bit of a fast track but I felt up for it and my bloodwork and exams indicated to my oncologist that I was ready).
I started chemotherapy two and a half weeks ago. I’ve had three infusions so far of Taxol. This is an intravenous chemotherapy that works on rapidly dividing cells of all kinds. One ramification of that action is that it will make my hair, eyebrows, and lashes come out in the next few weeks. I received it in a different regimen six years ago as many people do with early stage breast cancer following the use of Adriamycin and Cytoxan on a dose-dense schedule (every 2 weeks). It’s a popular drug.
The way it’s used now in the metastatic setting is different in terms of dose and frequency of infusions. In the metastatic setting there are different doses that are used. I’m using the highest right now. It is done in a “three weeks on, one week off” schedule. That means I get it once a week for three weeks and then I get a one week break. Though I never had a bad reaction to it in 2007, I did have a reaction to the drug the first time I got it a few weeks ago. I won’t go into the details of it here. I’ll just say that with increased amounts of steroids as pre-meds I’ve done just fine with the Taxol since that first episode.
For now I’ll close by saying I’m grateful for the friends that have been lending a hand with rides and playdates and meals while I’ve been housebound and unable to drive. I’m thankful for all of my readers who have been checking in on me and waiting patiently for this update. I am so happy to see so many new blog readers and Twitter followers in the past few weeks!
I want to give special recognition to all of the doctors, nurses, aides, therapists, and everyone else I came in contact with at Sloan-Kettering while I was hospitalized. Yes, there are always ways to improve, but I can truly say that I felt fortunate to be in such a caring environment for those weeks. I never doubted that it was the right place and that everyone there had my health and overall well-being first and foremost in their minds. It was always a team effort and for those of you who helped me in every way, I thank you. The fact that I miss so many of the you who cared for me shows that you made an impression on me.
The blogposts will return to a mix of updates, practical advice, and poetry as the weeks go on and I feel more and more like myself. Most posts will be shorter than this one but I know most of you have been wondering how I am and what I’ve been up to. I think this brings you up to date.
*Please note that I do not need suggestions for my side effects. I haven’t gone into the details here of what I’m taking, but I do have what I need from my team. Thank you!
Find a bit of beauty in the world. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
January 10th, 2014 §
 The car has always been a place of refuge for me.
The car has always been a place of refuge for me.
The shower, too.
Water to rejuvenate
Clearing away the old,
Ready for a new day ahead.
The moment of awakening is significant.
I have learned quickly what the next few hours will be.
I try to give a nurse a complete report but I encounter one problem immediately.
I really cannot type accurately.
My body shakes, my hips cry out in bony futile gasps. I gather up my pump cords, release myself from the wall’s grip.
I walk, counter-clockwise around the nurse’s station with a vengeance, trying to push the pain and discomfort away.
……………………………………..
I am Angry at this morning and that which has me here.
The tears arrive.
The radiation pain seems to be on the way in.
How long with it last? Does that mean it’s working? I and everyone else ask.
“I don’t know” is the way to do it. I say it aloud to the dark, embarrassed after the first word that I realize I am alone in the room.
I hear my voice, speaking to someone not present.
I can’t help but cry as I push the pole.
The movement makes it better. It reminds me of being carefree on a summer day, wind in my hair from the sunroof, feeling the sun on my face.
I think of my friends readying their homes for the day before work and school.
I can feel the radiation, where it burns, or at least the spots where tumors are trying to escape their home,
where they try to find new lands to conquer in a cat and mouse inside my body.
It doesn’t matter what stinking metaphor you use for it; in this case, all roads lead to Hell.
I contemplate eyeliner while the nurse stands, patiently waiting to see how I’ve done overnight.
…. But there is no one there.
I focus very hard on the tasks at hand: morning medicine most especially.
I start to tell my nurse that I weighed myself already today. Or yesterday. Or two days ago. But I can’t remember now. And so I remain mum.
In each moment my mind leaves. I don’t know where it goes. But in those gaps which feel like seconds, minutes have gone by.
The tea is divine, hot silky relief from the cold my body cannot push out.
I realize whatever it is I thought I could accomplish at the keyboard won’t happen once again.
I can’t concentrate. I find gibberish on the page. It takes hours to do a few moment’s work.
Extra time lost.
Time lost.
My precious time.
I stay committed to sitting up, bedside, fighting the urge to recline.
I listen to music trying to keep myself alert.
I think about my children, wondering what each is doing…
I realize today I am too foggy from medication.
I won’t be able to do much for a while. I am too busy talking to people that are not there.
I will rest, let the pain calm, let my head settle.
January 9th, 2014 §
No matter where you are
There is always beauty in the delicate unfurling of the morning as
It and its inhabitants come to life for the day.
A chair scrapes on the floor upstairs,
An electric bed adjusts,
An IV pump sounds,
A shade gets lifted to see the twinkling city.
A soft voice enters the room,
Two pills in a plastic cup down the hatch without disturbing a keystroke.
Vital signs are taken, the velcro cuff rips.
Vials of blood from my port,
The soft tapping of the tubes as the tech manipulates them deftly in one hand to keep refilling constant.
An IV pole whines like a morning toddler standing in her crib, anxious for first attention of the day.
Toilets flush,
Breakfast orders placed.
Young doctors starts to trickle in to find out how each patient’s night went.
And then some of the real business of the day starts.
Decisions made each day about life and death.
Who has surgery today,
Or a chemo change,
A transplant,
Biopsy.
Some will go home, some will not be ready.
News will be given.
Each person has a life unfolding here today. But remember it is a life.
Not a diagnosis, not a body part.
But just as the tide goes in and out,
Gives and takes,
So does metastatic breast cancer.
It progresses, taking more,
You hopefully have an arrows left in the quiver to try.
You tame it back and do the dance again. And again.
Leapfrog through treatments trying to stay one step ahead.
There is always adjustment.
It is a shifting target. You’d best be on your toes.
I am at the beginning of what treatments are available for me.
Don’t you count me out yet. Far from it.
Just because this disease can’t be cured doesn’t mean there isn’t a lot of life left in me; there is still so much for me to do.
I am living with cancer.
I want to count the days until I can be home and me again. But we do not know exactly how many are left. Getting closer I hope.
When I get back home it will be a different me, but that is not the point.
This is part of metastatic breast cancer and now I’ve had my first introduction.
It’s been 15 months since I received my diagnosis.
This is the first time I’m needing any type of radiation.
I will have to pull out some more aggressive weapons in chemotherapy options.
 But as I’ve done each time, my oncologist and I will research and discuss.
But as I’ve done each time, my oncologist and I will research and discuss.
She and I took this photo last night in my room as we talked about what the treatment plan will be for this week to get me out of the hospital. Once we have a short term plan then we will know what the next few months will look like. There is defiance in setting out on a new path.
The first step should be a confident one, not a toe dip into the shallow end.
For now the hospital is where I need to be as we finish evaluating exactly where the cancer is how to best target it. Additionally, we are still are fine-tuning pain control via the pump. It is a process to convert from using IV pain medication (rapid and adjustable help) to oral ones. The excruciating pain that comes from the tumors in my hips and spine demands serious pain management until we can allow time for the effects of radiation and chemo to settle in. That’s been a main focus. The pain will get worse before it gets better in those spots it seems. Radiation pain will precede improvement in many cases like mine.
The discovery in the past two weeks of more metastases was a curveball. But it’s standard practice for metastatic breast cancer. Totally typical.
I have quickly come to care for the people who work on the floor. There is so much care and assistance and tenderness every day. I look forward to sharing some of those stories in the weeks and months ahead. I could not be more grateful for the daily affection mixed in seamlessly with medical care.
Each room has a story.
My room has smiles and laughs and love. It has tears and anger and bewilderment. It has every part of life.
As I attack the cancer cells in my body I must always search for ways to bridge to the outside world. My family and friends have made that easy. They are my heart and soul. The supporters I have online help so much too. Your words of compassion and care keep me going and remind me why what I’m doing is so important. Using the time I have now while I am able to be functional is precisely the point… continue to give those too weak or unable to share the true experience of daily life with this disease a voice. To teach, to enlighten, to share, to support, to fundraise for research… and to always honor those who have died.
As always I could not do any of this without my oncologist Dr. Chau Dang. I love this photo we took last night in my room.
There’s always so much more to say. But I’ve got some time to do that.
So for now, my dad is here for a visit and I’m going to go have a cup of coffee with him… thanks again for the support I receive from so many of you. You know how much I treasure it: it’s my beauty.
Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.
January 8th, 2014 §
 I add another ball of surgical tape to the back of the photograph of my family hanging at foot of my bed.
I add another ball of surgical tape to the back of the photograph of my family hanging at foot of my bed.
Don’t fall.
Stay there.
Just stay.
Together.
…………………….
I wake up fettered, chained, restrained in body and mind.
The room is cold and yet it stifles:
Choking, pulling, grabbing me back, reeling me in.
I start to shake, fear manifest in movement,
Waiting for Reality,
The next interloper…
Another who will not be pushed away,
Ignored,
Wished or willed or
Bargained for.
I search for powers to rise above, get out, fly away.
Those dreams cannot escape that reality.
That shaking cannot stop.
When repeatedly pushing the button of narcotics is an act of acceptance,
A realization of what is,
In part an impotent attempt to eject myself from the room, the bed, my body.
The tears which accompany my pathetic try stay safely tucked away,
Hiding with hope and mental acuity and certainty.
Like middle school children the fear starts to divide, partners off, chooses a companion for the evening.
Two by two, hands on hips, turning tightly into a circle
Guarding spots of possession,
Declaring ownership,
This is mine.
The fetters must remain and yet I will not budge.
I have my spot.
Small perhaps,
But it is still mine.
I have my life.
I watch it shrink.
I have my words.
But now I see them dissolve around the edges
Like watercolors they bleed as they search for pristine lands to conquer
As they stretch that lifeline.
The words of disease become words my brain gravitates to.
The ebb and flow of cancer,
Of life.
And so too,
Inevitably,
Of death.
Each night when I return to my room after radiation now it happens:
My voice instantly is quiet, reverent.
I am resepectful of what I ask that beam to do,
I ponder the magnitude of something I cannot see.
And so I affix that photograph, one more piece of tape just in case.
Holding on to all that matters,
Doing as much as I can for as long as I can.
Day by day,
Storing up bits of beauty wherever I can find them.
January 6th, 2014 §
 The last weeks have not gone as planned.
The last weeks have not gone as planned.
I had the liver biopsy and PleurX drain put in my left lung on 12/31/2013. I was going to only stay one night for observation and to try to address the pain that I was having. Further tests revealed more information. The pain that we thought was coming from my lung and spine wasn’t just coming from my lung and spine. In fact I have some tumors in my bones in the left hemisacrum and right femur too. The spine tumors are now in more vertebrae than we’d thought.
I’ve actually been in the hospital for 6 days now trying to get the pain under control and formulating a treatment plan with my team. I will need to be here for a while longer. I am starting 10 sessions of radiation later tonight after being mapped this morning. We had hoped to do it in five sessions but for reasons I can’t go into now they have decided this is a better route and will be more effective for the future.
This treatment will stop the current progression of pain, but the way this radiation works for me is that it won’t provide true pain resolution for probably about 2 weeks and then improve further over the next few months. The pain reduction will be cumulative and take a while (long after the radiation is actually over) to see final resolution in my case. I’ll have to deal with this for a while yet.
The side effects because of where they are targeting the beams in my spine will be irritated esophagus, trouble swallowing, nausea, vomiting, and heartburn. The other radiation site in my hips will potentially cause decreased blood counts, pain, irritation, gastrointestinal pain and dysfunction and the like.
My pain is still not under control and I’m on a Fentanyl pump system that allows me to dispense medication as needed in accordance with the pain levels. I will convert over to oral medication and patches when it’s time for me to go home once we can figure out my needs. The pain and palliative care team here is unbelievably caring and devoted. So are the physicians and nurses. I have created an expanded family here already and can’t say enough nice things about the quality of care and total commitment to the patient.
I think for now that’s enough news.
Please, please respect my declaration that I do not want uninvited visitors, any gifts, or any flowers sent during this time. I know the intent might be good, but I appreciate so much those who have opted to instead donate to my Sloan Kettering metastatic research fund instead of purchasing anything for me. I haven’t been able to send thank you emails for those recent donations but trust me, they are appreciated. Good thoughts are also always just fine and have the right price tag!
This is a time when I am dealing with severe pain, a medical diagnosis that is unfolding and serious, and needing rest as much as possible. I do read emails but I am not responding to most at this time.
I was not able to start the clinical trial because of these newest announcements. We will see if I am eligible for it again in the future but for now we have to get the disease and pain under control. I did go on chemo for a few days but it now needs to be stopped during radiation. I will resume chemo after radiation is over and about a week of recovery time has elapsed.
Things change hour by hour, day by day. I’m adjusting the best I can. I hope this will at least let you know where we are, a long way from where I thought I’d be in the first days of this new year. Welcome to the world of metastatic breast cancer.
December 31st, 2013 §
I’ll be heading out soon to the hospital for two procedures. The first, a liver biopsy, will take samples of the small metastases to my liver for testing to get information about the cancer to help guide us in choosing targeted treatments. Features of cancer like hormone receptor status (ER, PR) and HER2 status can change over time and be varied in metastases in different parts of your body. It is important to repeat biopsies as time goes on to make sure you are still using the best drugs to treat your cancer.
The second procedure today is the implantation of a PleurX catheter. This will allow fluid to be removed from the lining of my left lung which has cancer in it. The fluid keeps accumulating so until we can get that reduced I will have to use this drain system at home to remove fluid daily. Keeping that level down will allow me to breathe well. This is a quite a process and I didn’t realize all that was involved. I’ll explain more about this in another post. This link shows how it works for anyone interested.
The main info I want to briefly share is that we now know more about where the excruciating pain I’ve been having is coming from. The PET showed that the cancer in my T12 vertebrae has grown and is encroaching on the space in my spinal canal. I also have an active spot of cancer that’s intense in my left hip. The spine, however, is where we are focusing the attention.
For now, we need to do more tests while I am in the hospital, but the immediate goal is to get radiation to my back and, if needed, to my pelvis. There is a lot to do to get all of that set but we are aiming to get radiation started by the end of the week. I do not know yet anything about what the protocol would be in terms of how many sessions but I do know that it will bring a lot of relief of pain once I can have that done. Until then it’s all about pain management.
I will also meet with a palliative care team while in the hospital to get the best assistance with the pain since it will be a while until I get relief at the source. Palliative care doctors are experts in pain management during all phases of cancer treatment, not just end of life. Palliative care teams help with side effects from the cancer and the treatments and are wonderful resources.
That’s all I have time to share for now but it looks like I still have a bit longer to wait for relief. Obviously this wasn’t news I wanted and I’m still adjusting to it. Once again, this latest development shows it doesn’t matter how you look on the outside; you can “look good” and still have cancer treatments that are not working, cancer that is progressing. This is an important message to repeat.
Right now we are still gathering information to decide whether I will participate in the clinical trial I was set to begin this week.
I hope you all have a safe New Year’s Eve and I’ll try to report back as soon as I can. Thank you for all of the support. It seems like a good time to once again share the link to my research fund donation page at Sloan Kettering in case anyone has those last minute end of year contributions to make!
December 29th, 2013 §
 No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
No news isn’t always good news. A lot has been happening in the last few days. On Tuesday they successfully drained 2 liters from my left pleural space after the unfortunate failed attempt last Friday. There is still about one liter remaining in there (the doctor can only safely remove about 1.5 liters at a time). Think about that: two liters. The size of a soda bottle… a few pounds. From one side. It’s astounding how much space and weight that is. Those are the actual bottles of fluid in the photo.
Everyone kept telling me how great I would feel after the thoracentesis. I did feel like I was breathing easier, but I didn’t feel great. In fact, I had quite a bit of pain. They checked for an air leak by x-ray as they always do after this procedure. There were no visible complications. But there was still tremendous pain starting that day and increasing into the next. It was more than the pain from the reinflation of a lung that had been compressed by half its size. But exactly what it was we weren’t sure.
By Thursday when I had to go back to Sloan-Kettering for my PET scan, echocardiogram, and EKG I was in agony. One of the doctors I met with could see how much pain I was in and prescribed some narcotics. I can’t take anti-inflammatories because I am having a liver biopsy next week and they put patients at risk for bleeding. I am so grateful a doctor seeing me about paperwork reached out to offer assistance and relief.
My father met me in the city. After I completed the required tests he drove me home. I can’t think of anyone better qualified to keep an eye on me than a retired cardiothoracic surgeon. Unfortunately, the pain continued. In all likelihood it is a combination of the cancer causing inflammation in the pleura and some nerve inflammation now that some of that fluid is gone and the lung is reinflated. It’s really all conjecture. We will see if the scans and tests reveal any additional information.
Oxycodone couldn’t keep the pain under control so yesterday I had to combine it with a Fentanyl patch. This duo is definitely helping me more; I’m still in pain but it’s more manageable today (Sunday). Each of these patches lasts for 72 hours and will deliver a constant stream of medication to me. I am pretty much bedridden.
It’s looking like Tuesday (New Year’s Eve) will unfortunately be a tough day. I was already scheduled to have a liver biopsy (This is not to check for malignancies; we already know there are metastases here. This procedure will be for repeated genomic sequencing analysis and other testing to make the best choices about chemotherapy and future clinical trials). Now, given all of the events this week, the team has decided that I need to have a PleurX catheter put in. This is a drainage system that will allow me to remove excess pleural fluid at home rather than having to have it tapped with a needle each time it builds up. The catheter will stay in place only as long as I need it, which will be as soon as treatment starts working and the fluid stops being produced in such copious amounts. I assume this will be at least a few weeks.
Having these two procedures and pain control issues means I will need to stay overnight in the hospital for observation. It’s amazing the lengths some people will go to to be in NYC for New Year’s Eve fireworks, isn’t it? Maybe Anderson Cooper will swing by while I’m recovering.
Once we see the results of all of the tests I’ve had and have these two procedures behind me, we will re-assess the plan to start the second clinical trial on Thursday. The most important immediate tasks at this point are to treat the two symptoms and get my breathing and pain under control. Immediately after that we go to work on the metastases to stop the problems at their source.
Thank you for all of the support I’ve had over the last few days including local friends who have been so kind and some friends who came from quite a distance to keep me company this weekend. I’m just putting one foot in front of the other and doing everything I can to gather all of the information I need to make a decision about what the best next step is.
Of course, as much as I can, I’ll keep you posted. Twitter is always the best way to keep up to date on daily happenings. It’s a lot easier for me to get quick bursts of info out in that medium. So many have asked: I have all of the help that I need and respectfully ask for no visitors or gifts during this time.
I would like to wish you all a happy and healthy 2014 if I don’t post again here before we all ring it in.
December 23rd, 2013 §
 For three days I’ve been mostly bedridden. During two days of sixty degree weather I didn’t make it out of the front door. What I believe is a virus sidelined me for the weekend and today (Monday) I’m still trying to get strength back. Thankfully I think it’s my immune system making me the target; no one else in the family has gotten it.
For three days I’ve been mostly bedridden. During two days of sixty degree weather I didn’t make it out of the front door. What I believe is a virus sidelined me for the weekend and today (Monday) I’m still trying to get strength back. Thankfully I think it’s my immune system making me the target; no one else in the family has gotten it.
Tomorrow I will go back to Sloan-Kettering for another attempt at a thoracentesis. I have had many people ask more about the process and what it is. This was a very good summary with a graphic. It kind of gives me the willies (does anyone even say “willies” anymore?) to look at that.
When even television seems too much,
And hours go by staring out the window.
I listen to the sounds of my children playing,
I hear life go on without me.
It was a day like this that I wrote the lyrics to the song “Six Minutes,”
A day I wished for the time to go. Just go by faster.
But as on that day,
Today I am aware that these are the days I’m fighting for.
If I didn’t want them I wouldn’t be doing all of this.
I know that this is a tough day. Tomorrow will be one, too.
But I also know that someday, hopefully long from now, it will count as a good day, a great day.
And that realization scares me too.
I spoke with a patient care representative at Sloan about some of the mistakes that were made on Friday. I told her my story and we talked about some ways she could follow up. I told her I wasn’t angry, I know mistakes happen, but I thought there were ways to try to make sure these things didn’t happen again. At the end she gave me her contact information. I said, “I love my doctors and the care I get. But there are always ways to improve. I appreciate the chance to give those suggestions to someone who can do something about them.”
Then I started laughing. “You know, I hope to be calling you with suggestions for many years to come. That will mean I’m still here, trying to help patients get better care and trying to help doctors and nurses provide it.” She started laughing too. “You know, I really like that perspective. I’m not sure I’ve ever heard it put that way. I like thinking about more suggestions as meaning more time.” We thanked each other and hung up.
And I thought about it.
Everything is an equation now.
Everything is a calculation.
Everything has a cost.
I try to balance risks.
I study statistics and results.
But in each equation I calculate, the result is always time.
Nothing is more valuable than time that I am able to enjoy the world and those around me.
December 21st, 2013 §
 When I was growing up and there was a particularly tough day my mom would use the expression, “Mama said there’d be days like this.”
When I was growing up and there was a particularly tough day my mom would use the expression, “Mama said there’d be days like this.”
Yesterday was one of those days.
My husband and I left the house before dawn. At about 8 AM I started my appointments. First was a physical exam with vitals taken and a review of symptoms. I met a new oncologist who was filling in while so many of the doctors were away (Friday of a holiday getaway week). We arranged this match because she is the Principal Investigator on a new clinical trial the team has been discussing as a good fit for me. As regular readers know, in my last post I explained that my cancer has progressed in some spots (stable in others) so we need to try to find something better now.
We reviewed my scan results and what she and my regular onocologist think we should do next. A slot in a new trial opened this week and it seems to be a reasonable next step to try another non-chemotherapy method. I’m going to save the details of that study for a later post but for those of you who know and understand the jargon, this one involves a Novartis drug called LEE-011 which is a CDK 4/6 inhibitor in combination with an anti-hormonal agent. This clinical trial is what I’m signing up for next.
The protocol for this drug is very challenging. It involves many trips to the city, especially in the first month where it will be once or twice a week, sometimes just for a blood draw. Some of those visits will be 8 hour sessions where blood is taken a few times to check drug levels in the blood before and after taking the pills. None of the blood draws can be done near my house since the conditions and testing all must be carefully controlled as part of the study. I’ll enumerate side effects and other details in a later post but this one looks to affect me more in daily functioning than I’ve had to deal with in the last few months. I’m definitely nervous.
We talked for a long time about the study. I had already gotten word from my oncologist about her own recommendation. I signed consent forms. I scheduled the necessary tests. They require a CT scan (I just did one, though it falls 2 days outside the testing window. We should be able to get an exemption for that so that I don’t need to redo it). I will need a PET scan, likely need a repeat bone scan, an echocardiogram (this drug can have cardiac side effects), an electrocardiogram, blood test, urine test and, (rats!) a liver biopsy. All of these must be completed in the next two weeks during my “washout period” (interval of time where you are not taking any chemotherapy agents and so you are starting with a clean slate to measure effects in a new clinical trial). Of course, the holidays are not an easy time to accomplish all of these.
I then went to get chest x-rays to monitor my pleural effusion (fluid in the sac around my lungs that makes breathing difficult). After those x-rays and fasting until almost noon I had 40 minutes to finally grab a quick bite. Then I went to the main hospital to meet with a pulmonary physician to decide what to do about the pleural effusion and find out how bad it actually is.
I had a full medical history and symptom assessment with a nurse and then met my new pulmonary doctor. He told me that my left lung is compressed to about 50% of its usual size from the fluid that is there. He estimated 1.5 liters of fluid have accumulated. He said it “layered” on x-ray which means it’s still flowing and therefore would be easier to extract. We decided to do a procedure called a thoracentesis to drain it. One of my morning blood tests that had to do with clotting had come back high, something that would mean we couldn’t do the test. We figured out it had been drawn from my port, which should never be done for clotting tests because they use an anti-clotting liquid called Heparin to flush the port each time and that would lead to inaccurate results.
Through a lab snafu it took 2.5 hours to get the new results rather than 40 minutes. By the time we finally had the all-clear to proceed it was about 5 PM. I still had barely eaten or had anything to drink. For the draining they sit you on a table with your feet dangling and have you bend over a stand for support. It is very much like having an epidural placed. They use local anesthetic to numb the skin and then stick a needle between your ribs, insert a catheter and vacuum extract the fluid (which should take about 10-15 minutes). The doctor got the catheter in, got a small sample of fluid going and…
My blood pressure plummeted. My heart rate dropped. I got hot and woozy and clammy. Yup, I passed out. They had to remove the drain and get me on oxygen and lay me down. I revived quickly, but we could not continue. So, I have the pain from the needle in my back but nothing to show for it. I will now have to go back on Christmas Eve to try again (fully hydrated and fed, hopefully this will be the key). I was obviously disappointed and emotional by this point. I had to go get the X-ray you need to confirm that no damage was done by the needle, and we made a train that got us home at 8 PM. It was a long exhausting day without too much to show for it in terms of relief.
It’s hard not to feel defeated on some of these long days when it just seems the mountain is so big to climb. Right now we are making a change to try to get better results in controlling cancer progression. I won’t be able to to travel for the holidays anyway, but now I will be spending time in hospitals rather than resting at home and taking a break. Cancer doesn’t give a damn about Christmas. Or families. Or anything that matters to me. But my doctors do. And they continue to show caring and concern and work so hard to try to make things better. Without that help and support this would be so much harder. Even when mistakes happen (and yesterday there were quite a few with blood draws and lab tests and so on), every doctor apologized. I definitely shed tears many times yesterday out of frustration, which doesn’t happen too often.
As I waited for my results I watched the office staff exchanging gifts, talking about holiday parties and Christmas cookies. One by one they packed up their belongings and turned out the desk lights. I was the last patient left in that department. That was hard. But I also know that I got to walk out of the hospital last night. I still got to go home and sleep in my own bed. And when I got home I made it just in time to hug my children and see Tristan’s artwork, all sparkly and smile-inducing. He asked me at bedtime why I couldn’t go on vacation with the rest of the family again this year. I explained to him that altitude makes it harder for me to breathe. The air is thin, and I would not feel well. I asked if he understood. “Yes, but I am still sad you can’t come.” “Me too, honey. Me too.”
I’m going to need to dig deep over the next 6 weeks. I’m going to need to ask for help with child care and logistics while I’m recovering from procedures and having so many trips to Sloan-Kettering. That’s not easy either. I find it very hard when I feel that I’ve not been strong enough, or that I’ve complained about the way a hard day has gone. I know it’s normal to need to just cry and complain and say to the cold night-time sky, “This isn’t fair. This isn’t how it is supposed to be.” Sometimes you just need to vent, though.
I need to be strong for the next few days and what they will bring. I want to make the holidays joyous for my family to the degree I can. These are the tasks that make me feel like me. The family shopping is done, the teachers’ gifts distributed, the tips for those who help during the year have been handed out, the holiday cards sent. These are the things that I know I could get a “pass” on. But they are the things I value. I will always try to show my gratitude to others.
Yes, Mama said there’d be days like this. But tomorrow is another day. And I don’t lose hope that it will be better.
December 18th, 2013 §
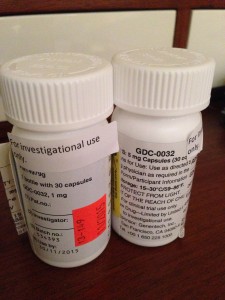 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.
December 12th, 2013 §
 Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Monday morning was an icy, rainy mess. I left the house before dawn, hitching a ride into NYC with Clarke as he drove to work. He dropped me right at the hospital because the weather was so nasty. I only had a short wait until the offices opened at 7:30 and started my first meeting around 8:00.
Before each meeting with the Principal Investigator on the trial (an oncologist) I usually meet with a research nurse. On Monday I had the added pleasure of meeting with the Fellow assigned to this trial. She is a fabulous doctor: thorough, curious, caring. We spent more than 45 minutes going over a checklist of symptoms we must review at each appointment. I need to answer if I am having any of those symptoms, describe them in detail, and rate if they are better or worse than at the last visit. Then we discuss what to do to help alleviate the symptoms. Certain medications are allowed and others are not because they could conflict with the investigational drug.
At this visit my main issues were muscle pain in my back, fatigue, occasional bone pain in my collarbone, continued loss of appetite (though my weight has stabilized), occasional shortness of breath, dry skin and cracked heels, and some minor GI issues. My blood pressure and heart rate are elevated. My pleural effusion has stayed at the reduced level, fluid continues just in the lower left lung lobe.
In general, I feel quite good on the combination of GDC-0032 and Fulvestrant. I’m quite happy with my current quality of life on the combo especially compared to other options like IV chemo. I hope that it will continue. I have historically tolerated targeted therapies very well. I have not had any issues so far with mouth sores, rashes, or serious GI issues which are some of the more common side effects with the investigational drug.
I was able to ask all of my questions, most having to do with the coming two weeks. Next week is a big milestone: I will have my first CT scan and that will be the basis for determining if I can continue in this clinical trial. At least two radiologists will examine the CT. One radiologist from the hospital will read the images, while a second, separate radiologist assigned to the trial will make his/her own determination as to how much disease there is compared to the baseline CT 7 weeks ago. If the cancer metastases are considered stable or decreased, I will continue in the trial. If the cancer has progressed (grown) by 20% or more, I will need to stop taking the drugs and be removed from this trial. There are defined days that are the days I must have this scan done so that all of us taking part in the trial are assessed at comparable points in treatment.
Next I met with the Principal Investigator on the trial. This is the oncologist who is the point person for the trial and supervises all of the patients in the trial at Memorial Sloan-Kettering. We reviewed how I am doing in general, what the plan is for the coming 2 weeks, and discussed bloodwork. I told her that am anxious to hear how the other people enrolled in the study nationally are doing. Because we all started within a few weeks of each other, there aren’t many reports yet.
Because I have completed my loading doses of Fulvestrant (an extra dose of the drug is required in the first month of treatment), I did not have to get those injections this week. That was a treat. I will now receive the two injections monthly.
My medication diary documenting the time I stop eating each night and the time I take my medication in the morning was checked as were my pill quantities. I scheduled my next visit (adjusted a few days earlier because of holiday schedules there, I have a +/- 3 day window for the appointments now) and headed up to the third floor to have my blood drawn.
My port incisions are healing beautifully. I’ve toyed with posting a photo of what it looks like but haven’t decided about that yet. The nurse and I donned the requisite masks for port access and the blood draw was easy. I was then allowed to take my GDC pills and start the clock on the 60 minutes until I could eat and drink (I must always wait one hour after taking them). I left the hospital about 3 hours after I arrived.
We’ve been watching my tumor markers and aren’t quite sure what to make of them. They’ve been rising a lot in the past month but I am also getting varied results from my two testing sites. Of course, the key piece of data to look at is the scan. But it’s been a challenging few weeks emotionally as I see where the markers are, watch them rise, and wait for the scan to tell me what’s truly going on inside by body. In a few days I’ll have answers. And then I’ll either be continuing on the trial for another two months or moving on to plan B (which my team and I have already identified).
I continually try to bring my focus back to the distinction between worrying and planning. Worrying is anticipatory. The way I look at it is that worrying is spending time thinking about things that may or may not be/come true. Planning is taking strategic action to set things in place and control things that I can control in the midst of so much uncertainty.
Having a backup plan or a next step if the scan brings bad news next week is planning. It means if this trial isn’t working I know what I will do next and make sure those steps are in place so I’m not suddenly reeling and trying to cobble together a plan. But worrying about the results next week won’t do me any good. The cancer is doing what it is doing. These drugs are either working or they are not. And my sadness or frustration about that won’t change the reality of the cellular processes.
And so I have been quieter this week, choosing carefully how to spend my time. I’m searching for joy each and every day and finding beauty in the small moments: our dog Lucy playing in the first snowfall of the season, Christmas shopping with Paige last weekend, puzzling through math homework with Tristan, Colin and I getting haircuts together and going Lego shopping.
We hug a lot.
We say “I love you” a lot.
We always have done this.
But now I hold on for an extra second each time and I squeeze just a little tighter.
………………………………….
For those readers new to my posts about this clinical trial, you can see my reports about Cycle 1, Day 1 here and Cycle 1, Day 16 here and my port placement and Cycle 2, Day 1 here.
























































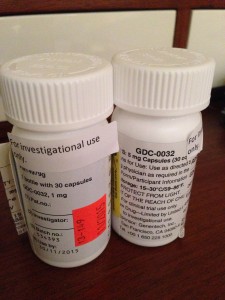

 Link to Twitter
Link to Twitter