 “This one has to work,” she says, “It just has to.”
“This one has to work,” she says, “It just has to.”
These are the words my phlebotomist says to me every time I see her. She says it strongly, willing it to be so.
I wish it were that easy. If wanting it could make it so… all of the people who send their support in prayers, thoughts, hopes, vibes, whatever it is they hope will help… all of those would work. And yet, here we are. Through no fault of theirs, or mine.
It is important to see the larger picture here, aside from my own life. It is important for everyone reading this blogpost to know that despite all of the hype and exclamation points and strong language about a cure or the promise of successful long-term targeted agents for metastatic breast cancer so that it can be more like a “chronic disease,” we are not there yet. The number who can live like that are the minority. Most live in this life and death game of Whack-a-Mole that I do now: metastases (“mets”) pop up, and you try to bash them back down but as you do they pop up somewhere else.
The state of metastatic breast cancer care is that you can’t just test your breast cancer, look on a chart to find the drug that will work and always shut it down. Metastatic breast cancer has eluded this formula so far. We don’t have drugs yet to even target every mutation. And we don’t know which inhibitors work. Most work best in combination with other treatments and we have to have clinical trials to test all of those options. All of those things take something those of us living with MBC don’t necessarily have: the luxury of time. In my case, I have a type of mutation called Pi3k-alpha in my cancer. I took an investigational drug that was a Pi3k-alpha inhibitor (along with another drug). On paper it should have worked. It was the most advanced type of targeted treatment I could get for that mutation.
Cancer is complicated. It has multiple pathways to get fuel. Block one? It finds another. And even when you have a drug that shows results in mice or in a few other people, you don’t know if it will work for you. There are too many variables, too many drivers of cancer in complicated feedback loops.
You can see where this is going. I have come out on the wrong end of the equation yet again. The trial drug combination did not work.
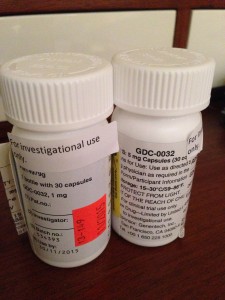
I’m no longer continuing on the clinical trial of GDC-0032 and Faslodex that I’ve been on for 8 weeks. The trial is required to drop me and we (my team and I) agree it’s not wise to stay anyway.
My CT scan showed stability in my disease in the bones, lymph nodes and lung nodules. That’s good.
But we have other more serious concerns now. The breathing problems I was having we knew were due to a pleural effusion which initially worsened 6-8 weeks ago and then seemed to improve about a month ago. I have still been aware of breathing issues throughout the day but it hasn’t had too much impact on daily functioning so I have just pushed through.
We now have confirmation that the pleural effusion is larger than in the last scan. The fluid that is causing the trouble is from metastases to the pleura (not to be confused with metastases to the actual lungs, the pleura is the sac that the lungs sit in. They usually have a trace amount of fluid present. This amount is a lot more. The fluid associated with the cancer has settled in the left lower lobe and has displaced the lung upward). In plain terms, there is cancer in the pleura that is producing fluid that builds up in that normally thin sac beyond what can be drained by the normal body process.
Additionally, my liver is now affected as well, unfortunately. There are mulitiple lesions that are metastases as well. This is obviously something I was hoping to avoid for a while longer.
The nature of metastatic breast cancer is that you don’t know how fast things will move or where the cancer cells will settle and thrive. They like the environment of soft tissues (liver, brain, etc.) so these developments are not surprising nor what I want to be hearing.
We need to get aggressive in a new way now. Anti-hormonal agents and inhibitors have not been working for me even though on paper they “should.” Treatments that logically should work might not. And that’s why I get angry when some very visible people in breast cancer care want to keep talking about how “close” we are to personalized treatments and even cures. The research has yet to support that idea. In fact, the latest research has repeatedly shown how complex the interactions are. We now know there are more than 30 subtypes of breast cancer. And even those subtypes don’t always respond alike to treatments.
Cancer is wily. And I hope I’m wrong about how far away we are from true leaps and bounds in MBC care. But I know I won’t see it in my lifetime. For how many decades now have we been hearing about those “breakthroughs” and “miracle drugs”? Yes, they’ve come in some cancers. But not MBC. Reporters and health care professionals in the public eye need to monitor how they spin info about the current state of metastatic breast cancer treatments. Let’s not send the message out about how “close” we are to a cure when there isn’t research to back it up. Let’s not send a falsely reassuring message out there that metastatic breast cancer doesn’t need much attention because soon we’ll be able to make it like a chronic disease anyway. Until we have actually done that, we must push full steam ahead and not encourage complacency in research.
Stepping off my soapbox to come back down to my life, what does that mean for me now? We must choose a new game plan. The one we talked about only days ago doesn’t seem the best option anymore (that’s one reason I don’t take the time to go into my plan B here when it’s still a hypothetical. You always have to be ready to adjust based on new information). We’re huddling and tossing around some options. I should know by Friday when I go back to my last clinic appointment on the trial. In all likelihood I’ll be going to traditional chemotherapy.
For now, it’s hard news to hear, especially at the holidays. I was originally diagnosed with early breast cancer on December 20, 2006. That anniversary approaches. I search for the beauty each day. I make myself find it. I won’t give up these days even when they are so hard. Today as I drove the kids to school the full moon sat above the horizon. It was beautiful in the blue sky after our gray day of snow and rain yesterday. We all looked at it. And I was glad to be able to see it with them.
As many of you already know, my first tweet of each day is a mantra I’ve written: “Find a bit of beauty in the world today. Share it. If you can’t find it, create it. Some days this may be hard to do. Persevere.” I love to start my day with that saying each morning. It centers me. And so many have responded that they like it too.
This news is not good. But as always, I go forward. As I’ve written elsewhere:
Cellular biology is King,
But paired to that fateful ruler I shall be a rebellious, argumentative Queen.
……………………..
One side note: with the popularity of my Twitter feed and the New York Times feature, my volume of email has soared in the past few months. I get so much mail, often with long stories and also requests for advice and guidance about cancer treatment and coping. I am so sorry to say that I cannot always respond to these letters. I hope everyone understands this. I am flattered but the time it takes to fully respond would be like writing a blogpost to each person. If the requests are easy, I try to answer as many as I can. I read every email that comes in and every comment on the blogposts. Any answers to emails come only from me. So I just am hoping that everyone understands that during these turbulent times, I won’t be able to reply to individual requests for advice and care. Thank you for understanding.


 Link to Twitter
Link to Twitter