May 3rd, 2011 §
There isn’t one right way to react to loss. And the thing about grief? It’ll sneak up on you precisely when you’re not looking.
This morning I attended a memorial service for a 38 year-old mother of two. She died of complications from leukemia, leaving a loving husband and two children behind. We were connected by a shared friend and a diagnosis of cancer.
When Kellie was diagnosed fifteen months ago and learned she needed to have chemotherapy I offered her my scarves. I had an extensive collection from my months spent without hair and had been serially loaning them out to friends after my hair grew back. After they’d covered my head, they’d gone to a friend’s sister in Colorado who had breast cancer. Then they went to a friend down the street who also had breast cancer. The fourth head they touched was Kellie’s.
During that time I had to deny others the use of the collection. I know too many women who’ve had cancer, I thought. There isn’t a break in between their tours of duty. The scarves don’t rest, they just keep traveling.
Perhaps some might find it icky to wear a scarf of someone else’s. That never seemed an issue for my friends. In fact, their softness from being washed so often was a bonus; heads are sensitive when hair comes out and the softer the cotton is, the better.
Kellie had those scarves for a long time. Her own fiery red hair was long gone; my scarves were a poor substitute for that ginger hair of hers. I like the thought of her having something comforting and cheery to cover her head during some of those difficult days though.
After the service today the guests stood talking over coffee and tea and far too many sandwiches and baked goods. Unprompted, our mutual friend assured me the scarves were safe and would be returned soon. I know when the stack comes back I’ll touch the scarves longingly, wishing Kellie were delivering them herself.
I’m overwhelmed today with emotions… sadness at the second Mother’s Day without my beloved mother-in-law, anger at cancer for claiming another young mother, frustration that oncology is often an art more than a science, worry that it will happen to me.
I just need to think. I just need to cry. I just need to remember. I just need to live.
May 1st, 2011 §
In the weeks before my surgery, I looked at pictures of double mastectomy patients on the Internet. I Googled “bilateral mastectomy images before and after” thinking I was doing research. I thought I was preparing myself for what was coming.
In reality I was trying to scare myself. I wanted to see if I could handle the worst; if I could, I would be ready. My reaction to those images would be my litmus test.
Some of the pictures were horrific. I sat transfixed. I looked. I sobbed. I saw scarred, bizarre, transformed bodies and couldn’t believe that was going to be my body.
Days later, when I met my surgeon for my pre-op appointment he said, “From now on, don’t look at pictures on the Internet. If you want to see before and after pictures, ask me– look at ones in my office. You can’t look at random pictures and think that’s necessarily what you are going to look like.”
All I could do was duck my head in an admission of guilt. How did he know what I’d done? I realized how he knew: other women must do this. Other women must have made this mistake.
The aftermath is terrible to me though not in the ways I’d anticipated. I have no sensation in most of my chest. I never will.
A major erogenous zone has been completely taken away from me. Yes, I have new nipples constructed, but they have no feeling in them; they are completely cosmetic. The entire reconstruction looks great but I can’t feel any of it. It does help me psychologically beyond measure to have had these procedures though.
Here I sit, two gel-filled silicone shells inside my body simulating the biologically feminine body parts I should have. And sometimes that thought is disturbing.
To be clear: I don’t regret having them put in. I’ve never regretted that. It was a decision I made, and made deliberately. I knew that reconstructing my breasts was the right decision for me. I’m getting used to them– I’m almost there.
I definitely don’t remember what my breasts looked like before. I only remember these.
I once asked my plastic surgeon to see my “before” pictures a year or two after my reconstruction was over. You know what? My “before” breasts didn’t look so great. In my mind they did.
In my mind, everything about my life before cancer was better.
But that’s not the truth.
My mind distorts the memory of my body before cancer. Then forgets it.
My mind distorts the memory of my life before cancer. Then forgets it.
With time, I can get used to a new self.
It’s like catching my reflection in the mirror: only lately do I recognize the person staring back at me.
For over a year the new hair threw me. It’s darker than I remember it being before it fell out. It’s shorter than it was before, too.
And the look in my eyes? That’s different also.
I just don’t recognize myself some days.
Sounds like a cliché if you haven’t lived it.
But it’s true.
April 15, 2009
April 30th, 2011 §
What does it mean to “be an inspiration”? A few people have said that to me recently: I am an inspiration. At first I laugh. I guess I’m an inspiration because I’m still alive. Maybe that’s enough.
What’s inspirational about me? Trust me, I’m not searching for platitudes here. I’m trying to get at “what makes someone an inspiration” and why do people think I and so many other breast cancer survivors qualify? There’s definitely more than one day’s blog in this question.
Is it being a mother and worrying about your children more than yourself? No. That’s what every mother does.
Is it summoning strength to confront chemo when it’s your greatest fear?
Is it putting a smile on your face when you are crumbling inside?
Is it speaking the words, “I have cancer” to your children, your friends, your husband, your parents, your in-laws, your brother, and all of the people in your life enough times that eventually it starts to sound normal?
Is “inspirational” when you offer to show your post-mastectomy body to women so that they will know the results just aren’t as scary as they are thinking they will be?
Is it answering everything and anything people want to know?
Is it putting words and feelings in black on white?
The essence of inspiration is being strong.
When you least want to be.
When you are faking it.
Strength.
When you lack it.
When you have to dig deep for it.
When your kids need dinner and you want to vomit from the chemo.
When you are too weak to climb the stairs.
And you don’t think you can get through another day.
Or hour.
Or minute.
Or second.
And you just want the pain to end.
Somehow.
Some way.
Any way.
Just have it go away.
When your pride is gone.
Dignity is gone.
All of it.
Being inspirational means being tough.
It means feeling rotten but not wanting others to.
It means wanting to put others at ease with how you are doing.
It means being a lightning rod for everything bad.
A catalyst for everything good.
A spark.
A resource.
A friend.
A wife.
A lover.
A mother.
A daughter.
It means telling your parents you feel okay when you don’t.
A little fib so they will go home and get some rest for the week.
Take some time off for themselves before they come back in 8 days and do it all over again.
A break so they don’t have to see their little girl suffer anymore
Because 6 days in a row is enough.
For anyone.
Because looking good makes others feel better about how you are doing.
So you put makeup on.
And dress well.
And put a big smile on your face.
So they will think you are feeling good.
And when you switch the topic of conversation, they will go along with it–
They will believe you when you say you are feeling better.
Okay, so maybe I am inspirational. I don’t call it inspirational. I can only admit to the smaller things. The micro things. Inspirational sounds big. Important. It’s hard to accept that one.
But I think I’m convinced.
The reason I’m going to finally concede is that I just realized something:
That was my goal.
Except I wasn’t calling it that.
I was just calling it doing it right.
I was calling it setting an example.
I was trying to show my family, especially my daughter, how you can tackle an obstacle– a big one.
I was just doing my job.
June 15, 2009
April 28th, 2011 §
I almost stole it: the tape measure with the purple finger prints.
After all, my surgeon had left it in my room by accident. After he had marked me with his purple pen and left my room on his way to get ready for my surgery, he left it sitting on the counter by the sink. In my nervousness and tranquilized haze I didn’t see it until after he’d left. I figured I shouldn’t hold onto it as I was wheeled in (“Who knows what germs lurk in tape measures!” I thought), and that if I gave it to a nurse it might get misplaced. So I shoved it in my bag of personal belongings knowing I’d be in for an office visit shortly after surgery.
I actually forgot about it during the days I was home after my two-day hospital stay. The drugs, the pain, the shock of my breasts gone and numb chest filled with temporary tissue expanders were all I could think about.
I forgot all about it as I was shuttled around for weeks unable to drive. I wasn’t living my normal life, my normal routine. I wasn’t carrying my purse and keys daily. I was living in pajamas and constantly trying to adjust to a new body once the drains were removed.
Then while I was looking for my keys a few weeks after my operation I saw it: the tape measure.
The yellow fabric one with the purple fingerprints up and down its sides.
The one.
The one that had measured and determined where my body was to be cut.
It was there in my bag.
There wasn’t anything particularly special about its practicality; it was just a tape measure.
Just like the ones I have sitting around with all of the odds and ends that inhabit kitchen drawers.
But that doesn’t capture the social meaning of it.
It wasn’t just any tape measure. It was mine.
But it wasn’t just mine, I argued with myself—it wasn’t a personal momento for me.
For a moment or two I wanted it.
I needed it,
as if to remind myself what had been,
of what I had been.
It wasn’t mine, I thought– it was his.
But more than that, it was theirs; it was ours… the other women who had needed it.
Now I was one of them. It was a shared history we had: strangers who had endured the same surgery, whose faces and names I would not know.
We were bound together by this object which had literally touched all of us.
And then I realized it was my responsibility to give it back.
Not for the obvious reason that it didn’t belong to me.
But as usual, I thought of the other women: the ones who didn’t even know they had cancer,
the ones who were going about their normal lives that day, and in the days ahead, only days or weeks or months from learning the life-altering news that would change their lives.
I felt giving back the tape measure would be my way of being bound to them, of saying “I know what you have ahead of you. I’ve come from there, and we are in it together.”
And so when I went to one of my office visits, I took it out of my bag and casually handed it to my surgeon. “You forgot this in my room when I had my surgery,” I said. He thanked me and said “I wondered where it had gone to.”
Little did he know the journey it had taken.
April 24th, 2011 §
I have a friend — a good friend. We’ve known each other for a long time. When I was going through chemotherapy for breast cancer, however, she wasn’t my most sympathetic friend. One of her typical reactions when I would talk about the bottomless fear of cancer recurrence that was swallowing me up was, “Well, I guess you’ll just have to get used to it.”
This was not really stellar support in my book; I think she could have done better. In my mind, because a close family member of hers had cancer in her past, she was not a stranger to its emotional component. Perhaps if no one in her life had ever had cancer I might have been more forgiving. Her relative was doing well, still in remission many years after her initial diagnosis. I mentally wrestled with myself: was I being too hard on a friend? After all, my emotions were on a rollercoaster. Things that didn’t bother me one day would infuriate me the next. Was I actually trying to let her off the hook for not emotionally supporting me? Was I excusing bad behavior? If those who have no experience with cancer shy away from those who are ill and those who have experience do so as well (if the memories are too painful to think about) then who is left to support you when needed? I couldn’t decide if I was expecting too much; maybe I was setting my friend up for failure.
Many times on the phone with her during my months on chemo as she proceeded to rant about the problems in her life and the ways in which things were not going her way, I wanted to point out to her how my life was “doing me wrong” in a bigger way.
Looking back, I wanted to trump her woe.
Lately, she has been having some medical issues of her own. Nothing permanent or relatively serious, but annoying and painful. For the last few weeks she has had some pain that is “excruciating.” She’s abroad this week, on vacation with her family. The pain, I guess, was not enough to keep her from that. While she has complained about her pain, her appointments, her problems for the last few weeks, I’ve really been holding back. I’ve really had to fight the part of me that wants to once again lash out.
“I guess you will just have to deal with it,” I want to say just like she did to me.
“I guess it’s not bad enough you can’t take your European vacation,” I want to say in a childish retort.
I want to trump her pain.
I want to wave the cancer card. Cancer trumps her issue, chemo trumps the discomfort she’s got.
Four years ago I found it almost intolerable that she should complain to me about the small things that were bugging her… the traffic on the way to school dropoff and how “inconvenient” her child’s schedules were. The way she had to take her child to the doctor twice in one week to check out an ear infection. How repairmen were keeping her waiting.
These things get sympathy from me under normal circumstances; these are things that bug me in my own daily life.
But not then.
While I kept silent then,
put it behind me then,
this latest round of friendship injustice just makes that time raw once more.
It brings that anger back.
My fear is that every time my friend has a hard time from now on, I am going to again have that feeling that she let me down when I needed her. I thought I had moved past it, but I guess not.
I don’t want it to get in the way of our friendship.
Maybe someone who wasn’t there for me then can’t really be a friend now.
Maybe some lessons can’t be learned until you go through them for yourself.
Maybe she can’t know how her responses hurt me unless she experiences it for herself someday.
The thing is: I don’t wish it on her.
People have different strengths.
We shouldn’t expect a person to be good at everything–
To fulfill all of our needs, all the time.
Extraordinary times call for extraordinary measures.
Maybe that’s true of forgiveness too.
April 13th, 2011 §
It seems like you can’t rank anguish. You shouldn’t be able to “out-suffer” someone. How do you quantify misery?
And yet, somehow we do.
“My problems are nowhere near as bad as yours.”
“I feel terrible complaining to you about it when you are going through so much yourself.”
I hear these types of comments all the time.
I make these types of comments all the time.
Placing ourselves in a hierarchy of pain and suffering serves to ground us; no matter how bad our situation is, there’s comfort in knowing there’s always someone who has it worse. Like being on a really, really long line at the movies or at the check-in at the airport, as long as there is someone behind you, it somehow seems better.
Hospitals use a pain rating scale: “On a scale of 1 to 10, how bad is your pain?” I was very intrigued when my son Colin was in the hospital for a week with a ruptured appendix and they asked him to rate his pain. At the time he was 5 years old and didn’t understand what they wanted him to do. He didn’t understand the concept of comparing one level of pain to another: it hurt… that’s all he knew. He used a binary scale to assess his pain: did it hurt or not? But as adults we know better: pain is not a yes-or-no question. Rather, there can be levels, ranking, quantification, and comparisons.
These mental exercises are necessary to keep us going through hard times, no matter what type. Before I got cancer, cancer was a “go-to” negative reference point. I mean, how many times have you thought “I’ve got health problems, but at least it’s not cancer”?
I did that. A benign lump needs to come out? At least it’s not cancer. A mole needs to be removed? At least it’s not cancer. My son has a cyst in his spinal column? At least it’s not cancer.
Then one day it was cancer.
So what could I pacify myself with?
At least it’s not terminal.
At least they can remove the body parts it’s in.
At least I have tools to fight it.
Then there was the big one: at least it’s happening to me and not my child.
I have a few friends with children who have had different types of cancer. These men and women (and their children, of course) are tough and have my utmost respect. I have thought many times, “That is harder. At least that’s not me. I don’t know what I would do.” When my son Tristan was diagnosed with deformities in his neck I thought “at least it’s something physical. At least it’s not something wrong with his brain. At least it’s not something that is fatal.” It’s cold comfort though. It’s still pain. It’s still grief. It is still hard.
I have often said I hate becoming anyone’s negative reference point. “At least I’m not her” someone might think of me. I always thought that meant they pitied me. I didn’t want that. But now I realize that it is okay for people to be glad they haven’t walked in my shoes– in reality, that’s what I want. I don’t want anyone to be where I have been; I’d like to be the lightning rod that keeps others I know safe. But, if it gives comfort to anyone to know that at least for today, their problems are not as big as mine, I think that’s good.
Because actually, at least for today, I’m doing just fine. I had laughs, and warmth, and hugs, and a day without pain—and I know that there are many people out there who can’t say the same.
Today I’m not the last one on line.
April 11th, 2011 §
 The months and years go by. Like all of you I mourn the quick passage of time. “Where did the fall/winter/year go?” I hear my friends asking.
The months and years go by. Like all of you I mourn the quick passage of time. “Where did the fall/winter/year go?” I hear my friends asking.
Projects we hoped would be accomplished — tasks we hoped would be done — sit unfinished. Organizing photos, cleaning out a closet or a room, reading that book a friend recommended; many things went undone in the dark and cold months of winter.
Maybe there were emergencies, maybe there were health issues, maybe you just couldn’t get the energy together to accomplish everything you wanted.
Regardless the reason, there can be a bit of disappointment when a season ends.
Growth happens in fits and spurts, not with smooth, sliding grace.
With each phase comes
pain,
discomfort,
unease,
restlessness,
sleeplessness,
yearning.
At the time of my mastectomies the reconstructive surgeon placed tissue expanders in my chest. These were temporary bags of saline that would be slowly filled to stretch out my skin to make room for the silicone implants that would eventually take their place. Each week, like clockwork, I returned to my surgeon’s office. He accessed a port in each expander with a needle and added saline to each side. Each time after a “fill” my chest would feel tight. The skin wasn’t big enough for the volume inside, and it would react to the increased pressure by stretching. Until the skin could replicate there was achiness, tightness, a slight ripping or tearing feeling.
A similar sensation happened to me during my pregnancies. The growth happened fast; I got stretch marks. I had visible proof my skin just couldn’t keep up; the growth was too rapid, too harsh, too vigorous.
I often wonder if mothers and fathers get psychological stretch marks when we are asked to accommodate changes we’re not quite ready for.
What can we do? What options do we have? None. We must “go with the flow” and do the best we can. Our children grow and change whether we like it or not. We do them no favors by trying to protect them, coddle them, and keep them young.
We give them wings to fly when we give them tools to be
confident
and caring
and inquisitive
and trusting
individuals.
I am often moved to tears as I watch my children grow.
I sit in wonder at the succession of infancy, childhood, and adolescence.
I know that as a mother I lack many skills, but I also know that the words I have written in my blogs and essays will one day be a gift to them too.
Not a gift to the children that they are, but instead a gift to the adults that I am raising them to be.
Each August as they go back to school I marvel that another school year has passed and yet another is here.
No matter how you measure time it always goes too fast.
The growth happens too fast.
The growing pains hurt.
The stretch marks might be invisible, but they are surely there.
April 7th, 2011 §
I’m cranky, I’m sad, I’m frustrated.
I don’t want to explain how I feel to family members. I don’t want to have to.
I want to yell, “If you’d had cancer you would understand!” But I know their ignorance is my prize… the prize I get for the fact that some of the people I treasure most haven’t had cancer.
I’ve seen a comaraderie that comes with this disease.
We may have had different types of cancer, different treatments, different prognoses… but… we are tied together.
When I was diagnosed one of the first things I was struck by was how vulnerable I felt. I worried about my family, especially my (then) seven-month old son Tristan who had his own medical problems. “Who will fight for him?” I thought. “No one will love him the way I do. No one will be his advocate the way that I will. I have to do it. I have to be here for him. I have to do what it takes to stay alive.” That became my mantra.
But once introduced, the worry could not be abolished. It could be dampened, minimized, controlled. But it could not be removed.
Two days ago a high school classmate died of brain cancer. Today I got word that a woman I know is in intensive care after complications from leukemia.
I ache for their families, for their children. I can’t explain the nuances of these feelings well. I have been here at the keyboard trying to find the words and repeatedly come up short.
And so, perhaps it is enough to say that I don’t always have the right words to convey what it is I am feeling.
But that doesn’t mean I feel it any less.
April 4th, 2011 §
I have a friend who says that “cancer has been her gift.”
She says that it’s been the best thing that’s ever happened to her.
That perspective doesn’t suit me. Despite being optimistic and determined, I am a realist. I see the ugly warts.
I don’t think it’s the best thing that’s ever happened to me; in fact, I wouldn’t wish it on anyone.
A gift is something you want to share.
Something you want to give to someone else.
Something you say “Next time I need to give a special gift to show someone I care, this is what I want to give.”
Cancer is not that thing.
Language matters.
The words we use to describe illness, death, and emotion are important– we should choose them carefully.
Cancer is not a gift:
It’s what you get.
It’s what I got.
It’s a twist of fate.
A happenstance.
A piece of bad luck.
But once you’ve got it, you have to decide what you’re going to do with it.
You can’t give it away, so you might as well make the best of it.
Fortunately, some good comes with it too.
And one of the best parts is the people you will meet.
Just because you don’t think it’s the best thing,
or a good thing,
doesn’t mean you are a negative person
or a bad person
or any particular kind of person.
In fact, it may mean you are a realistic person.
It may mean you are having a bad day.
Or a good day.
Or just a day.
And you will have those days:
Good
Bad
High
Low
Carefree
Despondent
Manic
Depressed
Terrified
Numb
Grateful
Spiteful
Bewildering
Confused
Overwhelmed
Sleepwalking
Drained
Energized
Proud
Embarrassed
And everything in between.
The days are gifts.
You can celebrate the days.
You should celebrate the days.
But don’t celebrate the disease.
Don’t treat it like a prize.
You are the prize.
You are doing the work.
You get the credit.
March 29th, 2011 §
I get asked a lot about health insurance claims. Having had many different diagnoses, surgeries, and procedures I have became all too familiar with interacting with insurance companies. In the last few years my diagnosis of breast cancer and the almost simultaneous diagnosis of our son Tristan with congenital spine and hand abnormalities has meant a level of paperwork, claims, and appeals I could never have imagined.
Navigating the maze of medical care and health insurance has become second nature to me. I think I’ve resisted writing this piece because initially I thought there wasn’t much to say. Having worked on this piece for weeks now, I realize the opposite is true: there is too much to say. Because each case is different it’s very hard to offer advice on what you, the reader, should do. But I’ve decided that’s the beauty of the blog format: I don’t have to cover all the bases. I don’t have to have all of the answers. I just need to do my best to help. And so today I’m starting to tackle this beast.
I’ve had many requests to write pieces about how to win against health insurance companies and many have suggested I go into this as a profession. I’m not sure about that one but I am definitely willing to share some of the insights I’ve learned throughout the past few years. I do think my upbringing in a medical household (my father was a cardiothoracic surgeon) helped familiarize me with medical terminology and how to correctly present a medical history. In addition to my tips you may be interested to read Wendell Potter’s recent advice in The New York Times: “A Health Insurance Insider Offers Words of Advice.”
Don’t take ‘no’ for an answer
The first piece of advice I have is simple: don’t take no for an answer. The fact your claim was denied is the starting point not the ending point. Insurance companies count on the fact that a large percentage of subscribers will receive a denial and either 1) forget about it, 2) intend to file an appeal but not follow through, or 3) incorrectly file the appeal paperwork (see Potter’s article, above). In any case, if they send you a claim denial and you don’t follow up for any reason, they win.
Always appeal
If you receive a rejection to a claim you feel you are entitled to always appeal. When I receive a claim denial I roll my eyes, roll up my sleeves, and say, “here we go again.” It’s what I expect, but it’s never the last word to me. Now, that is not to say that you always win– but it would take way more than one denial for me to accept that I’m not entitled to have a medical service covered. Persistence and determination are a large part of what it takes to win.
Physical (especially congenital) problems are easier to appeal than those related to developmental delays. I have little/no experience with appeals for diagnoses related solely to delays; while many of my general tips will still apply, more specific ideas will hopefully be available elsewhere online for those types of claims. I do know that when it comes to dealing with insurance companies those types of diagnoses are harder to quantify; this often leads to greater challenges with insurance appeals. In my experience, if the delays can be linked to anatomical problems, orthopedic issues, or diagnoses that can be validated with tests like MRIs or CTs, the case will be easier to justify.
Insurance companies must give you a reason whey they are denying a claim. Most often this reason is that 1) the treatment is experimental or investigational, 2) the treatment is not medically necessary, or 3) the treatment is not the standard of care.
In our case, initial denials have most often been because it wasn’t considered medically necessary.
Show the progression of the situation and how options have been exhausted
I always try to base appeals on the phrases “medical necessity” and “medically necessary.” When you document a surgery or service that you or your family member needs:
Be clear how it is necessary to daily functioning.
Describe what will happen if what you are asking for doesn’t happen.
Be sure to tell what you have tried already, and what has failed.
Show how your diagnosis and treatment history has brought you to this place–how there is no other reasonable option to what you are asking for (or how the alternative is not preferable).
Be complete but don’t ramble.
Be sure to include diagnosis codes and treatment codes (your medical professional will provide these).
Doctors’ offices don’t always have the final say
I should point out that a doctor’s office may tell you that you will have to pay out-of-pocket. They may tell you that they have tried to get your service covered, it was denied and therefore this is the last word. It’s not. For example, my neurologist’s office tried to get my Botox injections covered. Their office appealed the first rejection. They were again denied. They told me that there was “nothing else they could do”; I would have to pay.
Undeterred, I asked for copies of my medical records. I called my insurance company and asked what I needed to do. Despite what the doctor’s office told me, I learned that patients often have a separate appeals process available to them. While physicians’ offices can often get services covered and can be very helpful in knowing what’s been a successful method of appeal in the past, they are not the only way to get services approved. In a case like this there is actually a financial disincentive for them to have insurance cover it; therefore, they may not be as aggressive as you will. What does that mean? If I had paid out of pocket they would have received almost three times the amount of money that they receive when compensated by my insurance company directly.
When the office tried to get the injections covered, the insurance company denied the request on the basis that this was an experimental treatment– not FDA-approved for this use. I provided medical history sheets from my medical file. I documented every drug I had take until that point to try to prevent migraines and the dates I took them. I explained the medical condition/situation that resulted when I had migraines. I told them how the neurologist felt the Botox might help me. I included the original letter he had written to the insurance company. I explained that if they didn’t cover this treatment a more expensive, more medically damaging situation would result– this would mean more claims and more expense for the company. In the case of the migraines I documented how much my “rescue medications” were costing them per month and how a reduction in those would easily pay for the Botox I was asking for. I showed through my history with the numerous failed attempts with other drugs that the situation had not improved and in fact the side effects from those drugs had been debilitating. I also showed the literature about preliminary success in clinical trials with Botox and my neurologist’s observations about its efficacy in others and the potential efficacy in my case. I explained I had no other choice, and while it might be not-yet FDA approved, Botox was actually on the verge of receiving such approval (I was proved right when it did receive approval for this purpose less than one year after my request).
Include all relevant information and send appeal within the required time period
This letter of appeal doesn’t need to be 3 pages long. In fact, even in my most complicated appeals I didn’t write more than a page or two at most (plus the inclusion of the supporting documents). Be sure to appeal/respond within the time frame they dictate. In the letter be sure to include:
your contact information, subscriber number, and the doctor/hospital/treatment facility information
the case reference number that they provide
all relevant diagnosis and procedure codes
Ask doctors and staff for assistance, documents
Do not be afraid to ask your doctor and his/her staff for help: what tactics have they found useful? If there are multiple codes that apply which ones are the best to use? Do they have any sample letters for appealing? What has their experience been with your particular health insurance company?
Use the rejection letter as the foundation for your appeal
Take the rejection letter you received and read it carefully. Don’t just react with “it says no” and throw it away. It is vital; in it, the company must tell you why they are rejecting your claim (usually one of those three reasons I mentioned at the outset). This is the key to your appeal. You must address this issue. They’re telling you the basis, you need to fight based on that. Be thorough but don’t get off track.
Another good example of persistence in appeals came with a corrective band we used for Tristan’s quite-misshapen head (diagnoses of plagiocephaly and brachiocephaly). The facility we used for the DOC band told us that insurance claims were most often denied for this service. Indeed, the first claim was denied; they said the “helmet” to correct his misshapen head was for cosmetic reasons only. I appealed. I explained that because of his neck abnormalities the head deformity was an inevitable result of having his head fixed in one place. Because he was unable to move his head properly he had this inevitable result of a physical abnormality. I ended up having two helmets approved for coverage. Had I accepted the facility’s statement that “insurance companies usually don’t pay for this” or my first rejection letter from the company, we would have had to pay in full for both helmets. I should point out that I’ve seen success getting this particular service covered even when the plagiocephaly was not due to a unique condition like Tristan’s when the subscriber persisted with the appeal process.
You can appeal more than just a denied claim
– A facility that isn’t usually in-network may actually be considered in-network for some diagnoses. For example, Memorial Sloan Kettering Hospital in New York City is a hospital that specializes in treatment of cancer. Though it isn’t normally included in coverage by some health plans, insurance companies will often allow oncology treatments there under the Centers of Excellence program. Through this policy, hospitals that specialize in certain conditions are treated as participating centers (in-network). So, if you wish to have medical care at a facility that specializes in a certain medical condition be sure to check whether they are included in this special program.
-Prescription drug plans can be adapted. This is a big one. What do I mean by this? Just because your prescription drug plan says it will only cover a certain number of pills doesnt mean that’s the last word. My prescription drug plan said only 9 pills of my expensive migraine medication would be covered each month. The problem? I frequently needed more than that number. I decided to investigate. I called my insurance company and the administrators of the prescription plan and asked how I could get that number increased because it was medically necessary for me to have more than that number. They said my doctor could call and make a request. He called and they agreed to cover 18 pills. I received a temporary increase to 18 pills a month for one year, renewable each year by going through the same process. That saves me up to $2880 a year.
-Additionally, numbers of physical therapy/occupational therapy visits can be appealed. Our plan covers 30 PT visits for Tristan per year. He needs significantly more than that number. When the 30 are up, I write and document the medical necessity for him to receive more based on his anatomical defects. I state the skills he is getting with the visits and how they are necessary for his functioning. The physical therapist sometimes needs to include a letter and our pediatrician needs to write a prescription for the services.
Be organized. Take notes. Document everything
No matter what drug, service, surgery, or treatment you are appealing, you must be organized, take notes, and document everything. The key to my system is my medical binder. Have one for each family member. To see how to organize this essential tool, read my blogpost here.
Keep copies of your lab results, operative notes, and copies of all communication to/from your insurance company.
Be sure to have a fully documented medical history.
Save letters that were successful; if you need to repeat an appeal annually (like my migraine drugs and Tristan’s PT visits) then you will have a document that just needs minor tweaking.
Take notes on conversations (including dates and full name of the person you spoke with) at the company or doctor’s office. I learned that tip from my grandfather, a court stenographer for over 50 years: always keep track of the date, time, and name of the person you talked with. It may not be enough to prove your case, but if you can say “I spoke with (first and last name) on (date)” it lends credence to the fact that conversation took place.
Obviously, this post is not a comprehensive list of all types of conditions and how to win appeals for them. I know there are many readers who have had/will have experiences different from my own. I cannot tell you what will work for you; I can only tell you what has worked for me. I hope that by doing so and sharing some of these anecdotes you will learn something that you can apply in your own case. I realized while writing this piece over the past few weeks that there is so much to say about it. I’d like to consider this post an introduction to the topic; I will definitely revisit it again in the future.
March 18th, 2011 §
What if I hadn’t gone to the gynecologist on time for my 6 month post-partum visit?
What if, during the breast exam, when my left breast felt “different” (no lump, no real reason, just “different”) my doctor had dismissed it as post-nursing irregularity and told me to come back in 6 months for another exam?
What if, when I called to schedule the mammogram (only 18 months after a clear one) and they said it would be a few months for an appointment I had said, “Okay”?
What if I hadn’t called my doctor to tell her that’s how long it would take and ask if that was acceptable?
What if she’d said “yes”?
What if I hadn’t opted for a double mastectomy?
What if I hadn’t gone for a second opinion on chemotherapy? What if I hadn’t gotten a second pathologist to review my slides?
What if that didn’t happen and I didn’t find out with that second look that I actually had invasive ductal carcinoma in one breast, in my lymph node, and dysplastic cells in the other breast?
What if I had decided not to do those things? Where would I be now?
What if I hadn’t been assertive, perceptive, inquisitive, impatient, and willing to do what it took to get answers?
I probably wouldn’t be alive. Or if I were, I’d be spending my time treating an advanced cancer.
Not blowing bubbles with Tristan today,
Not praising Colin for his schoolwork,
Not planning Paige’s sleepover for tomorrow.
I wouldn’t be able to enjoy the things I enjoyed today.
But I am here.
I was able to be with my family.
I was able to help others.
I am able to look to the future with hope.
And for that, I am happy.
March 16th, 2011 §
 Perhaps the most common question I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a wonderful gift for someone who has just been diagnosed and is a necessity if you are the patient.
Perhaps the most common question I get asked by email is, “Someone I know has been diagnosed with cancer. What can I do?” Today I offer one suggestion. I believe this would make a wonderful gift for someone who has just been diagnosed and is a necessity if you are the patient.
Being organized is one of the best ways to help yourself once you’ve been diagnosed. When you first hear the words, “You have cancer” your head starts to swim. Everything gets foggy, you have to keep convincing yourself it’s true.
But almost immediately decisions need to be made — decisions about doctors, treatments, and surgeries. Often these choices must be made under time constraints. You may be seeing many different doctors for consultations. Medical oncologists, surgical oncologists, radiation oncologists, recontructive surgeons, internists— there are many different voices that you may hear, and they may be conflicting. It’s hard to keep it all straight in the midst of the emotional news. Not only are you likely to be scared, but also you are suddenly thrust into a world with a whole new vocabulary. By the time you are done with it, you will feel you have mastered a second language.
You can help your care and treatment by being organized. Especially if you are juggling different specialists and different medical facilities, you must remember that the common factor in all of this is you. It’s your health. It’s your life. I believe it’s important to travel with a binder of information about your medical history and treatment, as well as notes and questions.
This binder will mean that all of your information about your cancer will be in one place. This will be your resource guide. I cannot tell you how many times physicians have asked about my binder and said when I was able to produce test results, pathology reports, or other information they needed, “I wish every patient had one of those.”
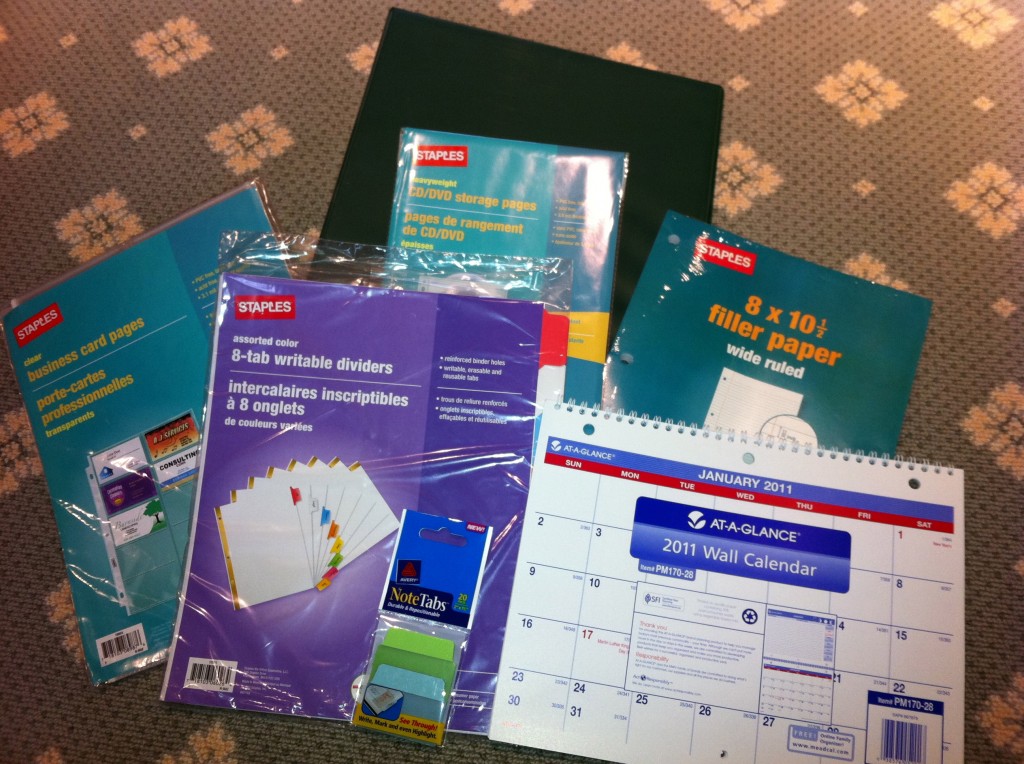
I suggest the following:
A heavy 3-ring binder
I think a 1.5″ binder is a good size to start. This size will allow you to easily access reports and pages and have room for the calendar. It will look big at first but you won’t believe how quickly you will fill it up.
Colored tab dividers
I like these to be erasable. I think 8 is the minimum number you will need. If you have a lot of specialists you will need more. The categories you think you will need at the outset may change. It’s easy to erase and reorganize them. Put the categories you will be accessing the most in the front so you aren’t always having to flip to the back. Once the binder is full it will make a difference.
Some starting categories:
- schedules (dates of appointments you have had, when the next ones are due, and how often you need certain tests done)
- test results/pathology (it’s very important to keep copies of MRI, CT, and pathology reports so that you correctly tell other doctors what your diagnosis is. For example, new patients often confuse “grade” with “stage” of cancer.)
- insurance (keep copies of all correspondence, denial of claims, appeal letters, explanations of benefits)
- articles and research (handouts, post-surgical information. Ask if there are any websites your doctor does approve of. My own oncologist said, “Do not read anything about cancer on the internet unless it comes from a source I’ve told you is okay. There’s a lot of misinformation out there.”) Keep your post-surgical instructions, any info given to you about aftercare.
- radiation/chemo (keep records of exactly what you had done, number of sessions, dates, drug names, etc. I also asked how my dose was calculated so I knew exactly how much of each drug I received in total)
- medications (drug names, dates you took them, dosage, side effects). I also keep a list of all of my current medications as a “note” in my iPhone. That way I can just copy it down and won’t forget anything on the list. You should always include any vitamins or supplements you take.
- medical history (write out your own medical history and keep it handy so that when you fill out forms asking for the information you won’t forget anything. As part of it, include any relatives that had cancer. Write out what type it was, how old they were at death, and their cause of death. Also in this section include genetic test results, if relevant)
Loose leaf paper
Perfect for note-taking at appointments, jotting down questions you have for each doctor. You can file them in the approporiate category so when you arrive at a doctor your questions are all in one place.
Business card pages
These are one of my best ideas. At every doctor’s office, ask for a business card. Keep a card from every doctor you visit even if you ultimately decide not to return to them. If you have had any consultation or bloodwork there, you should have a card. That way, you will always have contact information when filling out forms at each doctor’s office. For hospitals, get cards from the radiology department and medical records department so if you need to contact them you will have it. Also, you want contact information for all pathology departments that have seen slides from any biopsy you have had. You may need to contact them to have your slides sent out for a second opinion.
This is also a good place to keep your appointment reminder cards.
CD holders
At CT, MRI or other imaging tests, ask them to burn a CD for your records. Hospitals are used to making copies for patients these days and often don’t charge for it. Keep one copy for yourself of each test that you do not give away. If you need a copy to bring to a physician, get an extra made, don’t give yours up. If you need to get it from medical records from the hospital, do that. You want to know you always have a copy of these images.
Keep a copy of most recent bloodwork (especially during chemo), operative notes from your surgeries (you usually have to ask for these), pathology reports, and radiology reports of interpretations of any test (MRI, CT, mammogram, etc.) you may have had. Pathology reports are vital.
Calendar
I suggest a 3-hole calendar to keep in your binder. This will serve not only to keep all of your appointments in one place but also allow you to put reminders of when you need to have follow-up visits. Sometimes doctor’s offices do not have their schedules set 3, 6, or 12 months in advance. You can put a reminder notice to yourself in the appropriate month to call ahead to check/schedule the appointment.
Similarly you can document when you had certain tests (mammograms, bone density, bloodwork) so you will have the date available. I usually keep a piece of lined paper in the “scheduling” section of my binder that lists by month and year every test/appointment that is due and also every test I’ve had and when I had it.
Sticky note tabs
These can be used to easily identify important papers that you will refer to often, including diagnosis and pathology. These stick on the side of the page and can be removed easily. As your binder fills up, they can be very helpful to identify your most recent bloodwork, for example.
Plastic folder sleeves
These are clear plastic sleeves that you access from the top. They can be useful for storing prescriptions or small notes that your doctor may give you. The sleeves make them easy to see/find and you won’t lose the small slips of paper. Also a good place to store any lab orders that might be given to you ahead of time.
The above suggestions are a good working start to being organized during your cancer treatment. If you want to do something for a friend who is newly diagnosed, go out and buy the supplies, organize the binder and give it to your friend. He or she will most likely appreciate being given a ready-made tool to use in the difficult days ahead.
I also believe a modified version is equally useful for diagnoses other than cancer. When our youngest son was born with defects in his spine and hands it took many specialists and lots of tests to get a correct diagnosis. Having all of his tests and papers in a binder like this was instrumental in keeping his care coordinated. In fact, at his first surgery at The Children’s Hospital of Pennsylvania they gave us a binder to assist in this process. I know some hospitals do this for newly diagnosed patients already. Maybe my tips will help you or a friend know how to better use the one you already have. You may not need all of these elements depending on the complexity of your case, but I hope you will find some of these suggestions useful.
March 9th, 2011 §
Just because you know someone who died from cancer doesn’t mean I will.
Just because you know someone who:
felt sick,
felt great,
felt tired,
felt strong,
looked great,
looked awful,
lost her hair,
kept her hair,
ate healthy,
ate crap,
took vitamins,
ignored medical advice,
got acupuncture,
believed in holistic medicine,
ate no soy,
ate no sugar,
never laughed,
never cried,
had surgery,
had radiation,
received chemotherapy,
got silicone implants,
got saline implants,
had a great attitude,
had a terrible attitude…
Just because you know someone who did
one of these things,
many of these things,
some of these things…
doesn’t mean it will work for me.
It doesn’t mean it will kill me.
It doesn’t mean it will make me live.
Just because it worked for someone else doesn’t mean it will work for me.
It doesn’t mean it won’t.
Or can’t.
It might.
It might not.
Just because you know someone who died from cancer doesn’t mean I will.
February 23rd, 2011 §
When you (or a family member) are diagnosed with cancer people say a lot of insensitive things. It may be intentional or it may be just because they are caught off-guard and don’t know what to say to you. They ask bizarre questions, and often do bizarre things.
Sometimes you laugh.
Sometimes you just shake your head.
Sometimes you get angry.
But rarely do you forget.
So, today’s question is: what are the weirdest/craziest/most bizarre/most insensitive things people said to you/did to you while you or a family member or friend were going through treatment for cancer? Or died from it?
I have a few notable ones, but I’ll start with just one to kick things off. Someone asked me, “Is cancer what’s going to kill you? I mean, could you die from something else?”
February 22nd, 2011 §
I’m not really sure when I started #mondaypleads… I think it was about a year ago. On Twitter (@adamslisa), I got in the habit of nagging folks to go to doctors’ appointments. It started with mammograms. But soon I was sending out tweets gently nagging folks to take care of themselves and their families with a list of things I thought they should be doing. I had noticed that people were good at taking care of their children and their pets, but when it came to themselves– not so much.
At that time I had also become involved with a startup meme called #fridayreads. Now, I guess at this point I should assume that some of you are already wondering why I am writing with the number sign and why there were no spaces between those words. And what the heck is a meme? (that’s pronounced “meem” not “meemee” by the way)
For those who aren’t familiar with Twitter, here’s a brief explanation of hashtags. For a wonderful and humorous lengthier explanation of hashtags, please read Susan Orlean’s piece in her The New Yorker blog entitled “Hash”. The hashtag is that number sign (#), and one of the uses of hashtags is as a search tool. You can include a hashtagged term in your tweet (a tweet is a message of 140 characters) so that others can easily search for it. So you could hashtag #cancer or #snowpocalypse or #Egypt and then anyone with an interest in those topics could search for them and read tweets related to those things.
Now, one of the cool things about Twitter is that you can create a term; that is, you can make up a hashtag that will represent your idea. That’s a meme: a concept that spreads througout the internet. So… when my friend Bethanne Patrick (@thebookmaven) of The Book Studio wanted to start a meme to celeberate reading and have people share the book that they were reading with the Twitterverse each week, she started #fridayreads. Now with over 6,000 participants, the #Fridayreads team (through Twitter, an iPhone app and Facebook page) shares one of the things we love most: books.
Once I was involved with #fridayreads I wanted to create a meme to capture the nagging that I was doing and decided Monday was the day to do it. To try to be catchy, I created one to rhyme with #fridayreads: #mondaypleads. (By the way, I also created the #dailynag, a daily reminder for people to take their medications and vitamins. If you follow me on Twitter, you get a reminder each day.)
#mondaypleads has become what I consider to be an enormous success. I have received numerous messages from my followers that they appreciate the nagging, the gentle nudge it often takes to just do something you already know you should be doing. They tell me when they made the appointments, they tell me when they are going, they tell me how they went. It makes me feel good to know that people are listening, and doing.
I’ve even had a few cases where some of my 2000 followers didn’t know they should be going for some of these routine visits. One man read a tweet I made during #mondaypleads about going to the dermatologist for a skin check. He sent me an email: “I am in my 60s and have been a sailor for much of my life. Was there something I am supposed to be doing to monitor my skin?” I told him he should go to the dermatologist for a skin check to look for any suspicious moles and document the ones he has. He made the appointment. He went… and found he had two moles that were on their way to becoming malignant. They were removed before things got more serious. That’s exactly what you want: find things out while you can still deal with them relatively easily.
So… now you know the history. Now, on to the list.
Here’s what I do at home to organize my list: I have a binder of my medical records and reports with a piece of paper in it. The paper lists all of the doctors and specialists and tests I have had/need. I have the date and place that it was last performed and when I need a follow-up (6 months, a year, every 5 years, etc.) Every time I have a test, procedure, follow-up or appointment, I note it in this section. That way I never have to wonder “When was my last MRI and when am I due for another?” or “When did that doctor say I was supposed to come back?” If you have lots of tests, it’s a great way to keep track of what you had and where. If you only have a few appointments it’s easy to keep track of them if you keep them in a file or an iPhone note.
By the way, one of the best things you can do if you take a lot of daily medications is to put that list in an iPhone note (or similar memo). I have a note called daily medications that I update each time my dosage or cocktail changes. That way, when you go to a new doctor or are asked to update your medication list it’s easy to recreate– you just open this note on your phone and copy it. This has been an easy and useful tool for me, especially during the months when certain medications were changing. It’s also handy that a family member can easily access this information in case of an accident or emergency.
Here is a basic list of what I think people should be doing for themselves. Depending on your medical conditions you will need more than this. I’m not a doctor, these are just some suggestions of things I think people should be doing (at a minimum) to keep up to date.
— (For women) mammograms, PAP smears, and annual gynecological exams. Discuss the frequency of these with your doctors, based on your age and medical/family history.
—Dental visits every 6 months.
—Annual physical/internist visit, including vaccine boosters. Ask about tetanus and pertussis boosters; I needed those recently. If you are over the age of 50 ask your doctor about the shingles vacccine. May need to monitor kidney and liver function, blood pressure, and cholesterol. Men should have PSA screenings once they reach a certain age. Discuss the timing with your doctor. Here is a recent article about the guidelines for adult immunizations. There is a PDF for viewing the list in chart form by age.
—Depending on your age you may need a bone density test, especially if you are a post-menopausal woman, went through menopause at an early age, or have a history of breast cancer. Certain drugs and treatments may affect your bone strength. Talk to your oncologist or internist.
—Annual skin check at the dermatologist to document and monitor moles
—Annual eye exam
—Depending on your particular medical conditions, endocrinology visits to monitor bloodwork including thyroid and blood sugar issues, especially if you have weight issues.
—Colonoscopy. Check with your doctor when to start doing these; it will vary based on family history. No one wants to talk about them but they really are not bad, folks. Find any problems early and your outcome will be better. I’ve had two already and so I’m not telling you to do something I haven’t done.
—Make sure your will and end of life directive are up to date. No one wants to think about dying but knowing your wishes will be carried out can be a relief. Make sure someone knows where these papers are and a copy is accessible in case of emergency. Also, adequate life insurance is a must… and best arranged while you are still young and healthy.
— Finally, here is information from Yale on becoming an organ donor. You could save a life by becoming one. Please donate blood, platelets, and get tested with Bethematch.com to be part of the bone marrow registry.
Again, these are the basics. It takes a lot to keep on top of your health. There is no better investment you can make than in yourself. I hope this helps!
p.s. If you have a chronic medical condition have been recently diagnosed, or are a caregiver, my blogpost about organizing your medical records, test, and papers may be helpful. Go here to read “The Must-have Binder: my key to being an organized patient or caregiver.”
February 7th, 2011 §
I’ve written previously about my decision to have my ovaries removed two years ago in order to (hopefully) decrease the likelihood that my breast cancer will recur (“The Impetus of Fear”). Though I tested negative for the BRCA-1 and BRCA-2 genes, my hormone receptor positive cancer feeds off of the hormones that my ovaries produced. To significantly reduce the amount of those hormones circulating in my body (as a pre-menopausal woman of 38) I decided to have a salpingo-oophorectomy (surgical removal of my Fallopian tubes and ovaries). I recovered from the surgery itself within two weeks; the effects of plummeting into menopause overnight have been longer-lasting and in some cases, quite devastating.
As I do with almost any issue in my life, I have repeatedly talked to my mother, Dr. Rita Bonchek, about the ramifications of my decision. This angst has led to many talks about the difference between regret and guilt. As a psychologist specializing in issues of grief, loss, death, and dying for twenty years, she always has a keen ability to separate out what appear to be muddled feelings. She often has ways of explaining complicated topics in easy-to-understand terms and using real-life examples to illustrate her points. She and I have collaborated here to present some thoughts on these two emotions. The ideas on the differences between guilt and regret are hers; I have pushed her to explain things as fully as possible and helped with some of the re-writing.
We hope that they will help you to think more clearly about actions in your life and the emotions you have about them. We look forward to hearing your comments and any follow-up questions you have. Because my mom is not on Twitter, if you have any questions for her, it’s best to put them in a comment below; I’ll post her answers for everyone to read, too. This is meant as an introduction to these two emotions, not a comprehensive analysis of them.
………………………………….
People use the word “guilt” more often than is appropriate. Improperly using the word “guilt” can result in unnecessary emotional distress and harsh self-criticism. The word “guilt” refers to something you did, something which you feel you shouldn’t have done because it was morally or legally wrong. But what if the experience you feel guilty about was not something you caused or had control over? Then you would feel regret, not guilt.
Here is an actual situation: Ann was referred by her family doctor for grief counseling. She was unable to cope with her persistent feelings of guilt related to her husband’s death several months prior. Bob was diagnosed with a terminal illness and he was bed-ridden. He needed constant care and attention which was mainly provided for by his wife. Bob was hospitalized for three weeks prior to his death. Ann was with him throughout that time as well.
On the day of Bob’s death, his wife left the hospital room to use the bathroom. When she returned to the room, the nurse told her that Bob had died in her absence. Ann was overcome with feelings of what she termed “guilt” and punished herself for not having been with Bob at the time of his death. For months she could not function and was preoccupied with thinking how terrible she was in being absent when her husband died. She mentally punished herself for breaking the vow she had made to herself to be with him when he died. Instead of focusing on the 99% of the time she had cared for him while he was ill, she focused on the last minutes he lived.
Why shouldn’t Ann feel guilty? Because she did not do anything that caused her husband’s death; she was not there. If Ann had asked the nurse whether it was “safe” for her to leave for a few minutes and the nurse had cautioned her that Bob could die at any time, and then Ann chose to leave, then she could justly experience guilt because she ignored information indicating he could die during the time she was away. In this alternate scenario, Ann had the personal responsibility for making the decision to go, she had control of making the decision that resulted in her absence, and could therefore justly experience feelings of guilt. As a counselor, if someone is justifiably guilty for an action, I would advise them to make a confession, offer an apology, take responsbility, and — if possible– make reparations.
By disproportionately magnifying these few minutes to overshadow all of the months of care Ann had given Bob, the result was that she could not forgive herself. After discussing the difference between regret and guilt, Ann came to see that there was, in fact, nothing to forgive. She understood that she was only responsible for her own actions; Bob didn’t die because she left the room. By reframing the circumstances of Bob’s death, Ann was better able to properly grieve her loss and move on afterwards.
Though Ann did not experience guilt, she did have regret, a universal experience. Regret refers to circumstances beyond one’s personal control. An unidentified author defined regret as “distress over a desire unfulfilled.” Regrets can pertain to decisions made concerning: education (not getting a degree), career (working at a job that offered good income but no personal satisfaction), marriage (married too young), raising children (being too permissive), medical decisions (sterilization), etc. These and other decisions can be considered mistakes.
As an emotional response to a distressing experience, the sound of the word “guilt” is harsher and more of a self-reproach than the word “regret.” If you say, “I feel so guilty” you should make sure that the deed and circumstances surrounding it actually warrant your feeling of guilt rather than regret.
 Dr. Rita Bonchek has a Ph.D. in educational psychology. She spent twenty years in private practice.
Dr. Rita Bonchek has a Ph.D. in educational psychology. She spent twenty years in private practice.
February 2nd, 2011 §
 I remember distinctly sitting in movie theaters when I was pregnant. At various points throughout the film I’d tune out the words and images and get lost in my belly, feeling each of my children squirm and wriggle and stretch. “What if this is it?” I’d think to myself. “What if I go into labor right here, right now?” And then I’d think to myself, “In just a week or two I’ll be a mother, mother to a person whose body is inside mine but whose face I have not seen, whose voice I do not know, whose skin I have not touched. I’ll be mother to this person for his or her entire life, my life will be shaped by his, and his by mine.” And those thoughts seemed incomrehensible to me at the time. Too large, too vast.
I remember distinctly sitting in movie theaters when I was pregnant. At various points throughout the film I’d tune out the words and images and get lost in my belly, feeling each of my children squirm and wriggle and stretch. “What if this is it?” I’d think to myself. “What if I go into labor right here, right now?” And then I’d think to myself, “In just a week or two I’ll be a mother, mother to a person whose body is inside mine but whose face I have not seen, whose voice I do not know, whose skin I have not touched. I’ll be mother to this person for his or her entire life, my life will be shaped by his, and his by mine.” And those thoughts seemed incomrehensible to me at the time. Too large, too vast.
Then four years ago my little mental interludes changed form. “I have cancer,” became the thought that was too big to wrap my brain around. “Right now, while I am sitting here the cells are there. There is cancer in me. Right now,” I thought to myself. Eventually, after my double mastectomy, during my reconstruction, I could sit, arms crossed across my chest and feel the tissue expanders in me. And even now, I need only take a sharp, deep breath to feel the implants in there, reminding me of what has come to be.
Sometimes, when there is a lull in a movie, I still “check out.” Just for a few moments.
As if when I am sitting there,
in the theater,
away from everyday distractions,
lost in someone else’s life,
only then can I think about the larger things that haunt me.
The other night I found myself momentarily thinking about my body, and its cells. “Are there any cancer cells left?” I thought. “What if there are some still there, right now, dividing, multiplying, gathering momentum.”
I sat and wondered if they’re gone. If they’re not. I wonder what the plot will be, how it will end. My favorite movie endings are the ones where you get to see what happened to the characters– how things ended for them, what the final chapter was– an epilogue. I realize I can’t have that knowledge about myself. And I’m not really sure I’d even want to. I guess everyone likes a happy ending. That’s the only kind I really wish I could know about myself.
January 27th, 2011 §
I love this piece in the New York Times about the myth that a fighting spirit and good attitude make all the difference in how (and if) you recover from a life-threatening condition. I wrote a piece in 2009 about this and am reposting here since the topic has received attention this week.
…………………………………
“Having a good attitude makes all the difference.”
People say that to me all the time. I am sure every person who’s had cancer hears that. I think what people are saying is that there is something you can control in all of this mess. There is so much you can’t control, that you have no choice in. People say how you deal with it, how you choose to behave once these things are thrown your way, is up to you.
Here’s what I think:
I think what matters is good health insurance. I think what matters are friends and social support to get you through. I think what matters are children, or pets, or others who nurture your soul and remind you why you are going through all of this: there are others who care about and depend on you.
I think good medicines matter. I think caring and capable oncologists matter. I think talented surgeons matter. I think getting good advice matters.
Why am I resistant to the idea that attitude matters? Not because I don’t believe it. I reject this idea because it places the burden of healing on the individual patient. It places the weight of getting better in his/her hands. I think cancer patients have enough to deal with. We have enough to feel guilty about and responsible for. I think tossing our collective attitude into the mix is a lot of pressure. All eyes are on us anyway.
Now we have to watch how we treat the thing which is killing us.
Having a good attitude says:
the power is in you to survive.
The power is in you to heal.
The power is in you to do well.
But looking at the converse is troubling. The implication is that if you suffer, if you relapse, if you die– it is your fault.
If you had only had the right attitude,
you could have been better at keeping it away.
You could have been stronger.
You could have beaten it.
That may be flawed logic in the philosophical sense but I think it’s worth exploring. Even if that logic can’t be reversed so easily, I think the implication is there: you should have the right attitude because it makes a difference. Difference in what? Difference in your outcome. If it didn’t, then they would not say it.
Or would they?
There is an impetus to control, as I’ve talked about frequently in my writing. You just feel like you need to do something. I think that’s what people are grasping on to with their advice. They know you can’t do much, so they tell you to control the one thing you can: your mindset about what is happening to you.
Sometimes I just don’t want to have a good attitude.
I don’t necessarily think it makes a difference.
I don’t want to think positive thoughts all day
and see the good in what is happening to me.
I think that can be healthy too.
January 27th, 2011 §
This post was written at a time when I was feeling down, fatigued, weary. I started thinking of all of the things that I was looking forward to when I felt better, things I hoped for the future, things I was thankful for along the way. These would be my payments; these were things that I accepted for my struggle.
……………………………………
A currency of thanks,
a commodity of gratitude,
a medium of memories.
Hugs
smiles
laughs
tickles
sunny days
warm laundry
long baths
newly-mown grass
freshly-baked cookies
hot coffee
baby snuggles
happy endings
clean floors
baby shampoo
good blood counts
clear scans
easy blood draws
short waiting room waits
no side effects
no hidden costs
generous co-pays
quiet offices
pain-free mornings
guiltless decisions
days without regrets
unconditional love
fading scars
new friends
caring surgeons
information
honesty
openness
truth
validation
appreciation
understanding
sympathy
hope
research
progress
empty parking spaces.
someday, my hope:
no more cancer.
January 21st, 2011 §
Beautiful.
It’s not a word I have used to describe my body. Ever.
Even when I was young and lithe and strong I didn’t think of myself that way.
After three pregnancies that word was certainly gone from my vocabulary.
I loved and appreciated my body for what it had done, what it could do. However, that feeling was more a result of recognizing its practicality more than its aesthetic appeal.
When I was diagnosed with cancer everything changed.
One aspect: body parts became liabilities.
It doesn’t matter, people said, you are the same person inside.
Was I? Am I?
Ripples replaced smooth expanses of skin.
Rosy scars replaced creamy white flesh.
I didn’t mind them then– I don’t mind them now.
Or do I?
When the glass is half full it is still also half empty.
I can see both views by shifting focus.
I’d rather be scarred than dead…
…but I’d rather have been healthy than ill.
I miss the hormones. My life is not the same since the removal of my ovaries shut down almost all of my estrogen production. One of my doctors told me the change would not be radical. She was wrong. There isn’t a day that goes by that this decision doesn’t affect my life.
When we’re in the thick of it we are afraid. We think fear is bad, but in fact the fear is useful: fear causes us to be brave.
Fear allows us to do things we never thought we would have the strength to do. Chemo was my greatest fear; I literally made myself ill with fear about receiving chemotherapy. I wanted any excuse not to do it. Saying no to chemotherapy would have been the wrong decision for me to make based on my particular risks. My fears of metastasis, dying young, and leaving my children was greater. I needed to do everything I could: that was my mindset. Whatever it takes.
I have reminders every day that I am not who I used to be.
And so, when I think of the words you are still the same person I realize it’s not true.
I’m not the same person… and I think that’s okay.
In fact, I’m not sure it could be any other way.
I ordered the book The Scar Project in October and finally received it two weeks ago. Photographer David Jay has been photographing breast cancer patients who were diagnosed between the ages of 18 and 35. The images are stark, real, true. The book has statements from the subjects, a bit about their cancer experience in their own words. I realized when I looked at them how beautiful the women were. That’s the word that instantly came to mind: beautiful.
With scars, without breasts, without hair… whatever each picture showed I found myself thinking how powerful those images and words were. And then I realized something: I am one of them. If they are beautiful so am I. It isn’t just their bodies, it’s their strength. Maybe my definition of beauty has changed; I just see it as meaning more than it used to.
Now that I am older I see that resilience is beauty. Scars can be inspiring. Scars are the marks we have to show that we have lived, endured, survived. I need to be willing to say that if those women are beautiful, so am I. Why I still have a hard time saying that, I don’t know.
Of course I am sure that is what David Jay wants to happen with his project; he wants to show that the reality of life with cancer is one that can be empowering. I do draw strength from my past, but the mixed emotions inside continue to wrestle with one another. David Jay has succeeded: he has shown strength in beauty and beauty in strength.
I need to do the same.
January 19th, 2011 §
April 1, 2009
How can you be a good friend to someone with cancer? Doing the same things you do for any friend: show you care, express interest in her life, be sympathetic, and offer to help when she will let you. The best thing you can do is to be a good listener.
Being a good listener seems obvious, but it’s harder to do than it sounds. First, you need to remember that if you haven’t had cancer, you aren’t going to really understand what your friend is going through, what she is feeling. You might think you do, but you don’t. You can’t.
The fact that you don’t share the bond of cancer, though, doesn’t mean you can’t be helpful, supportive, and caring. You can be all of these by listening. Some of the most supportive people in my life have never had cancer. It doesn’t matter. They are good friends in part because they are good listeners.
Listening does not entail giving advice.
They are two totally different acts. One requires that you listen while your friends talks. One involves you giving your opinion about how your friend can change and what she can do differently/better.
In times of active crisis, the best thing you can do is keep your opinions to yourself. Unless you truly know what that crisis feels like (the death of a child or spouse, a serious medical diagnosis, or a divorce, for example), your advice will fall into the category “things people-who-don’t-understand say.” For me, others’ advice usually misses its mark. The result? I feel further misunderstood; therefore, I am more isolated.
My mother taught me the difference between these two acts. “Do you want me to just listen or do you want my advice?” she would ask. Sometimes I wasn’t sure. Sometimes I’d ask for the advice and not follow it. The fact that she gave me the choice, asking the question directly, gave me control. I was telling her how to be helpful– what I needed from her.
I know it’s not easy to just listen. But sometimes asking the specific question, “Do you want my advice or do you just want me to listen?” can help us be exactly the kind of people we want to be — better friends to those we care about.
January 18th, 2011 §
July 18, 2009
I went by my friend’s house today– the one who was just diagnosed with breast cancer. I wanted to put something in her mailbox. When I opened the mailbox it was full of mail already. She hadn’t taken in yesterday’s mail yet.
Of course she hadn’t. Why should she worry about mail when they are worrying about cancer and what it means for their family?
I left the bag in her mailbox on top of the day-old mail and went away, remembering:
Remembering that time in my life two years ago when I was diagnosed with cancer.
I managed to get the kids where they needed to go (I have no idea where that was).
I did the things I needed to do (I have no memory of what they were).
I went the places I needed to go (I can’t remember where they were).
There is no room for anything else in these days, these days in the beginning.
There is no room for anything else except to hear the words again and again,
as if you need to convince yourself that they are true: “You have cancer.”
There is no room to
do anything,
think anything,
say anything,
be anything,
fear anything,
hope anything,
dream anything,
live anything,
love anything,
breathe anything.
In these days there is no room for anything but cancer.
But these days will pass.
You don’t believe it.
Can’t believe it.
But it’s true:
these days will pass.
Your life will change.
You can make room for other things,
better things.
And once again,
there will be room in your mailbox.
You will remember to get the mail because you won’t be thinking about cancer.
You’ll be thinking about the things you should be thinking about,
that you deserve to be thinking about.
Each day.
Every day.
Today
January 17th, 2011 §
 July 26, 2009
July 26, 2009
The riders lined up along the narrow street, more of them this year than last. The streets were still damp. At the first corner of the course, a large puddle remained from the previous night’s storm. Volunteers handed out yellow balloons to cancer survivors; the balloons danced and tugged at their strings, waiting for release.
The cyclists waited along the street, some joking, some quiet. Some looked up at their balloons, remembering. Some looked at the backs of the jerseys of their fellow riders, mentally noting how many survivors there were among them. As the announcer droned on about the course, ensuring that the 75 and 100 mile riders had maps, we all breathed deep breaths, psyching ourselves for some of the emotional moments about to occur.
An 11 year-old girl sweetly and strongly sang the National Anthem. Then the announcement came to release the balloons. The announcer said this bike event was for us, that it was in our names the riders were going. We let the balloons go and watched as they floated into the sky. Everyone clapped, some tears were shed. If only we could erase the pain that we’d had as easily.
And then it was time for the Survivor’s Lap of Honor. Any cancer survivor who is riding in the Connecticut Challenge takes an honorary lap around the starting area to be recognized before the official start of the event. Some of the cyclists are riding during treatment, some of them during chemo. How they get on a bike and ride I do not know. At the front of that pack of Survivors is my friend Lucas Whittaker. At age 11, Luke is the youngest cancer survivor at the Challenge. As such, he receives special notice and leads the pack.
Luke has beaten leukemia twice. When they announced his name and he started off on his lap of honor before starting his 25 miles, his father Martin (about to start his grueling 100 mile course which he rides every year in Luke’s honor) turned around to me, his eyes full of tears, and we sobbed, holding each other for a minute. “Your beautiful boy,” I said. “Look at your beautiful boy.”
He knew I understood. What this disease had done. How it had challenged them — his family. When Luke relapsed, it was a bone marrow transplant from his younger sister Grace that saved his life.
Luke’s mom, my dear friend Brenda, made her way over from where she was standing with their other children. She and Martin hugged and then she and I did too. We don’t even say anything anymore. We just hug. And sometimes we do the thing where our bodies just shake together as we silently sob.
And then we parted, and looked at each other.
And we knew: you can’t let yourself grieve or feel or cry anymore after that.
You’re going to have to take an IOU on loss for now, because there’s work to be done.
There’s business to be done — the business of living.
We turned back to the children. Back to Luke. And Martin. Back to my own children who had come to send off the riders. And the race got started. We wiped our tears and we cheered. We watched as every last rider pulled away. And then Brenda and everyone else walked toward the tents. And I stood for a moment, and cried a bit more. And then I realized the kids needed me. Again, the feelings would have to wait.
We made signs for the people we know who have had cancer. Volunteers take these posters and attach sticks to them; then other volunteers post them along the course for the riders to see as they make their way home. The list of people we know who have been touched by cancer was long. We made a sign for my friend who just got diagnosed with cancer ten days ago. One for our next door neighbor Catherine who is in remission from leukemia. My beautiful brave girlfriends who are in remission from breast cancer. My spectacular mother (also in remission from breast cancer) who is my continuing role model on how to charm the world with a smile. Paige made a special sign for Luke. Colin made one just for me that said In honor of Mom on it.
There was a cyclist who had MOM written in Sharpie pen on his leg. I couldn’t figure out why he had written it in the precise manner and location he had. All day I was thinking about it, and I couldn’t figure it out.
Last night after I drove the babysitter home, I was pulling into my driveway and it hit me:
he’d written it where he could see it when he was on the bike.
He wanted to see her name when he looked down.
When he got tired and looked down and needed strength on a hill or along the route,
he would see “Mom” written on his leg in this neat block font and think of his mother.
I don’t know if she’s living with cancer or if she died from it, but that image will stay with me.
That son, riding his bike 100 miles yesterday, thinking of his mother when he was pushing his body to the limit.
The business of living: that’s what yesterday was all about.
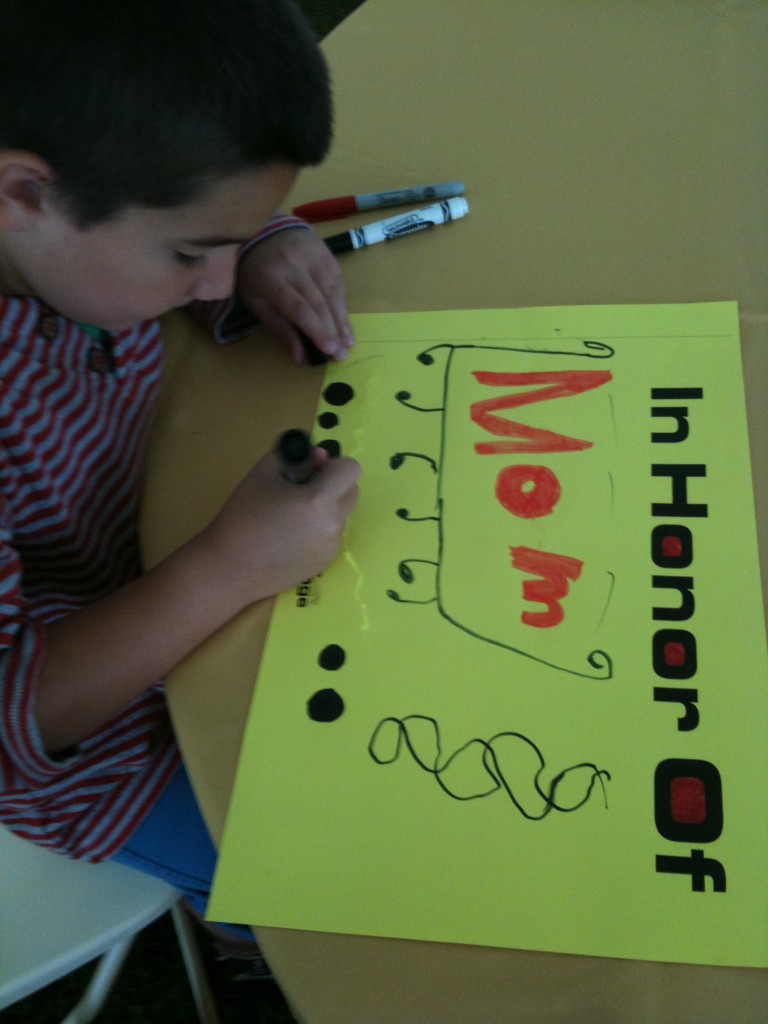
January 16th, 2011 §
A previous discussion about inspiration and setting an example provoked my friend Laura to write to me, “If something ever happens to me where I have to dig deep to find that strength that you have found (and shown), I will think of you. Often. And re-read your blog. Often.”
This was the highest compliment and I appreciated those words immensely. Her words got me thinking.
So many of my friends have mothers who’ve had cancer. In college, my two closest friends, Alex and Deb, both had mothers who had breast cancer. Somewhere in that experience was an expectation for them that someday, inevitably, they would have it too.
It was many years before my own mother did. And then right on her heels, so did I. Before Alex and Deb did. And so, like my mother was for me (see “Everyone Needs a Trailbreaker”), I suddenly became the trailbreaker for my best friends.
I’ve gone through some cancer scares with friends and acquaintances over the past three years. I’ve sat in waiting rooms, taken phone calls, written emails, met with women in person. I’ve helped friends, strangers, and friends of friends.
When I was young someone teasingly called me a walking encyclopedia. Somehow it still seems true. My husband only half-jokingly shakes his head when he hears some of the questions people ask me. He sometimes says, “They do know you’re not a doctor, right?”
I know that I’m the first of my friends to have breast cancer. And have it “bad.” The whole nine yards. That experience comes with responsibility. I know that having cancer at 37 means that I will be that resource, that friend, that support system.
In the future, others will need me. Friends will ask me how to help, what to do, what things mean.
There is a lot of pressure coming my way and I think about it already: what if I let them down?
That’s the kind of person I am.
I am already worried not only about getting through my own experience; I’m worried how I can help my friends if their time comes.
And statistically it will.
I’m worried who will be next.
I’m angry someone will be next.
I want to be the lightning rod.
I want to take in on for them.
I want to protect them.
Laura, I want to protect you:
I don’t want you to have to read my blog for strength.
I want you to read it because you want a window into a world you never have experienced. And never will.
That is my greatest hope, my greatest dream.
If I could sleep, that would be my dream:
To keep you all safe.
January 16th, 2011 §
I never want people to feel sorry for me– I don’t feel sorry for myself. I feel lucky. I live a great life now; I’ve had a great life so far. I’ve learned a lot along the way and gotten stronger and stretched myself in ways I could not have predicted.
Sometimes I wake up in the middle of the night panicked. The other night my worries about Tristan came to the surface. This week I have been working to get him additional physical and occupational therapy sessions from our town in preparation for kindergarten next year (if you don’t know about Tristan’s physical problems you can read about them here).
At 1:47 I lay in the dark wondering, “Who will care for this boy if something happened to me? What if I die — can anyone be his advocate the way I am?” I pondered that question for some time. I thought of the family in a documentary I watched two weeks ago called Monica and David. The film’s subjects have Down’s Syndrome and recently got married. They live in Florida with Monica’s parents in a condominium. Monica’s parents should be retired by now, enjoying their golden years. Instead, they have a full-time job caring for their adult daughter and her husband.
When I was watching the film I kept thinking about the same issue: who would help Monica and David if something catastrophic happened to Monica’s parents?
I realized that her parents have somehow come to terms with uncertainty, as we all must.
In graduate school my Ph.D. proposal dealt with management consultants and their claims of expertise. How did this group of professionals carve out a niche in the business market and claim that only they were qualified to objectively advise companies on what they should do to not only survive, but thrive? The certification of knowledge intrigued me. I never finished my dissertation, but many themes of study from years ago have stayed with me.
I never could have predicted that I’d be thinking about uncertainty in terms of cancer. I never could have known that those advising me on decisions would be oncologists and surgeons.
But just as Monica’s parents have learned to deal with that uncertainty, so must I.
Betty Rollin wrote that having cancer means being a little bit afraid at least some of the time. I know that’s true. But learning to manage uncertainty is a part of everyone’s life.
I think of individuals with obsessive-compulsive disorder that I talked about in a blogpost on the shows Hoarders and Obsessed. The specific type of therapy used in Obsessed (cognitive behavioral therapy) has been a great mental tool for me. Psychologists force affected individuals to “sit with their anxiety” until it reduces by half. In a nutshell, repeated exposures to the panic-inducing event prove to the patient that (the world will not end, they will not die, their loved one will not be harmed) if they do not give in to their compulsions.
The lesson? The body cannot exist in a heightened state of anxiety indefinitely. To cope, to survive, the level must (and therefore will) come down.
I take that insight and the examples I’ve seen and incorporate them into my life. I know that at each stage of my diagnosis and treatment for cancer I panicked. When we found out Tristan had physical problems I was terrified at the possible outcomes for what his disabilities could be (most of them thankfully not realized). But that seems to be a comfortable pattern for me: get new information, freak out for 24 hours, wake up and get to work learning, dealing, living. Taking our fears, whatever they may be, and learning how to better work through them can only help us… for uncertainty is a given.
October 27, 2010
January 16th, 2011 §
November 8, 2010
One of the phrases I heard often during the emotional events of the past few years is “Things happen for a reason.” The other night while Clarke and I were watching a reality show one of the contestants spoke the same phrase as she predicted elimination from the show.
“I think everything happens for a reason,” she said.
“No they don’t!” I reflexively argued with the screen.
“Why does that make you so upset?” Clarke asked.
“Because it’s just a way that this woman is rationalizing why this bad thing— elimination from a contest she’s competing in— is okay. She’s trying to tell herself that things really aren’t as bad as they are. She’s trying to console herself that there is a purpose in her suffering… that it will lead to something bigger and better, and that is just not necessarily the case.” I said.
I don’t think things happen for a reason and I find it unsettling when people want to tell me that cancer, or my mother-in-law’s death, or anything that has been a challenge has happened as part of some grand plan for something better.
I just don’t believe it. And I don’t want you to believe it about my life, either.
I think things just happen — and when they do, you have to decide how you are going to handle them. Those actions, those responses, can teach you lessons, but they are lessons you teach yourself. You can grow, get stronger, do something that you otherwise never would have. Alternatively, you might learn that you made a mistake and should deal with a situation differently the next time it comes up.
My attitude?
Don’t give away the credit.
Don’t minimize the hurt or disappointment.
Don’t rationalize why it isn’t as a big a deal as it is.
There isn’t necessarily a purpose in suffering; it’s not part of a causal narrative that “passing the test” will get you to the next step. You make your own tests, you find your own lessons. But using the word reason implies that it was given to you, designed for you.
And I just don’t believe that.
January 14th, 2011 §
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.
January 13th, 2011 §
There are ways in which I will never make you as readers understand what it’s like to have cancer if you haven’t. However, part of the reason I write this blog is to try to explain some of the cancer patient “mentality” (if you’ll accept such a generalization) to those of you who haven’t had cancer. To that end, you can hopefully be better friends, partners, spouses, sons, and daughters. There are things I didn’t know before I had cancer that I wish I had understood.
It’s not that I am special. It’s not that I am so smart. It’s that I have been there. Hopefully sooner than you have. And so I am reporting back from the field. To try to help you. Prepare you. Because if there is one thing I know, one thing I know for sure: you will know someone. It might be your friend. Your parent. Your child. Or even yourself. Maybe you already know someone. But one thing is for sure: you will know someone who gets cancer. And you know what? You already know me.
One of the ways your life changes when you have had cancer is that you begin to understand the phrase “It’s never over” in a whole new way.
As soon as you hear the three words, “You have cancer” your life changes. From the time you hear those words everything is different. You now have a history of cancer — even if it’s a cancer that can be removed and you don’t need any other treatment. It is now a history that puts you at risk. Now every medical problem, every medical history you give, every question mark, every medical mystery must be filtered through the lens of a history of cancer.
A woman I know from college was writing a brief note to me by email to thank me for something nice I’d done. The last part said, “Hope you’re feeling on top of the world (or close to it).”
My reaction? First I burst out in laughter.
Ah, the naiveté of the healthy!
On top of the world! Ha!
Then it actually got me riled up.
Angry.
How dare she think it was over.
Then I got angry at myself for lashing out.
I became contrite.
Why should she know better?
How could she know better?
It isn’t fair to expect people to know better.
Only once you know better can you do better.
If she only knew.
What was I going to do?
Write back and explain to her the error in her thinking?
Should I write back and say:
I counted every day, every hour, every minute, every second to be “done.” But when each thing was “done” there was always something else I was counting toward. Always something else looming. I’m never “done.” It’s never “done.” It’s never “over.”
The language we use reveals a lot.
When someone says,
“You must be on top of the world,”
that means:
“You should be”
“You ought to be”
or
“I expect you to be.”
For someone like me, if I don’t feel like that it’s hard.
I get angry. I want to say all of the reasons why that’s not realistic– why that’s wrong. Why that’s precisely what I’m not feeling.
But then, when my anger cools, I take that and turn it inward. And all I feel is disappointment. Disappointment in myself. Maybe I should feel like that. Maybe I really should feel on top of the world. The fact that I don’t means I’m not as far through this thing as I thought. It reminds me I’ve still got a lot of work to do.
Maybe the battle is not really with cancer. Maybe it’s with myself.
But I think the point remains: just surviving cancer isn’t necessarily enough. It’s not enough to make you feel on top of the world.
You can help those who have had cancer by not making the leap that just because they have lived through this round that they have “won”; don’t assume that they will necessarily be ecstatic, “done,” and ready to move on.
Rather than telling people what they “must” feel, we all can be better friends and listeners by asking questions rather than making statements.
Rather than saying “you must feel on top of the world” think of the difference it would have made if my friend had said, “Now that your treatment and surgeries are over, how do you feel?”
An open-ended question is always a safe conversation starter. I’m going to try it more often in my everyday life; I hope you will too. My wish is that it begins some good conversations between you and someone you care about.
January 12th, 2011 §
That chair you’re sitting in?
I’ve sat in it too:
In waiting rooms. Chemo rooms. Prep rooms. For tests. Surgeries. Procedures. Inpatient. Outpatient. Emergency visits. Routine visits. Urgent visits. To see generalists. Specialists. Surgeons. Alone. With friends. With family members. As a new patient. Established patient. Good news. Bad news. I’ve left with new scars. Prescriptions. Appointments. Words of wisdom. Theories. Guesses. Opinions. Statistics. Charts. Plans. Tests. Words of assurance. More bloodwork. Nothing new. Nothing gained. Nothing but a bill.
That feeling you’re having?
I’ve had it too:
Shock. Disbelief. Denial. Grief. Anger. Frustration. Numbness. Sadness. Resignation. Confusion. Consternation. Curiosity. Determination. Dread. Anxiety. Guilt. Regret. Loss. Pain. Emptiness. Embarrassment. Shame. Loneliness.
That day you’re dreading?
I’ve dreaded it too:
The first time you speak the words, “I have cancer.” The first time you hear “Mommy has cancer.” The day you wear a pink shirt instead of a white shirt. Anniversary day. Chemo day. Surgery day. Scan day. Decision day. Baldness day. The day the options run out.
Those reactions you’re getting?
I’ve had them too:
Stares. Questions. Pity. Blank looks. Insensitivity. Jaw-dropping comments.
Those side effects you dread?
I’ve dreaded them too:
Nausea. Vomiting. Pain. Broken bones. Weakened heart. Baldness. Hair loss. Everywhere. Unrelenting runny nose. Fatigue. Depression. Hot flashes. Insomnia. Night sweats. Migraines. Loss of appetite. Loss of libido. Loss of breasts. Phantom pain. Infection. Fluid accumulation. Bone pain. Neuropathy. Numbness. Joint pain. Taste changes. Weight gain. Weight loss. Some of them happen. Some don’t. Eventually, though? You name it. It changes. Temporarily anyway.
That embarrassment you’re feeling?
I’ve felt it too:
Buying a swimsuit. Getting a tight-fitting shirt stuck on my body in the dressing room. Having a child say “You don’t have any eyebrows, do you?” Wearing a scarf. Day after day. Wondering about wearing a wig because it’s windy outside and it might not stay on.
That fear you’re suppressing?
I’ve squelched it too:
Will this kill me? How bad is chemo going to be? How am I going to manage 3 kids and get through it? Will my cancer come back and take me away from my life? Will it make the quality of life I have left so bad I won’t want to be here anymore? Is this pain in my back a recurrence? Do I need to call a doctor? If it comes back would I do any more chemo or is this as much fight as I’ve got in me? What is worse: the disease or the treatment?
That day you’re yearning for?
I’ve celebrated it too:
“Your counts are good” day. “Your x-ray is clear” day. “Now you can go longer between appointments” day. “See you in a year”day. First-sign-of-hair day. First-day-without-covering-your-head day. First taste of food day. First Monday chemo-isn’t-in-the-calendar day. Expanders-out, implants-in day. First walk-without-being-tired day. First game-of-catch-with-the-kids day. First day out for lunch with friends day. First haircut day. “Hey, I went a whole day without thinking about cancer” day. “Someone asked me how I’m doing, I said ‘fine’ and I meant it” day.
That hope you have?
I have it too:
No more cancer.
Don’t you think that would be amazing?
I think so too.
January 10, 2010
January 11th, 2011 §
June 18, 2010
There. I did it.
This picture shows me one month after I finished chemo. Peach fuzz growing. Eyebrows gone. Eyelashes gone. Both pencilled in to hide their absence.
 This is the only picture I have of myself bald. When I was a shiny cue ball it never occurred to me to document it. If you look closely at my left eye, you’ll see a tear resting on my lower lid. I had just stopped crying. Long enough to put on makeup and flash that killer smile. I was just about to get my tissue expanders out and have my silicone implants put in. It was right before my 38th birthday. That’s what I told my plastic surgeon I wanted for my birthday– to be done with that next phase of my reconstruction.
This is the only picture I have of myself bald. When I was a shiny cue ball it never occurred to me to document it. If you look closely at my left eye, you’ll see a tear resting on my lower lid. I had just stopped crying. Long enough to put on makeup and flash that killer smile. I was just about to get my tissue expanders out and have my silicone implants put in. It was right before my 38th birthday. That’s what I told my plastic surgeon I wanted for my birthday– to be done with that next phase of my reconstruction.
It was hard to go in for that particular surgery at that particular time in my treatment regimen. When the staff came to wheel me in I had to remove my scarf. My surgeon hadn’t seen me bald. The nurses, my father, my doctor… all of them saw my head then. Of course it was run of the mill for them. They saw cancer patients all the time. But for me it was another way my dignity, my identity, my humanity were being stripped from me. I donned the fabric shower cap gladly, happy to have something (albeit flimsy) to conceal my naked head.
Only moments before, I stood in the bathroom with my plastic surgeon while he marked my body once more with his ubiquitous purple Sharpie pen. We talked again about final details of my breasts. I realized how these conversations had become so routine between us. While the subject of my breasts was no longer one that even caused a pause in chatter for us, I didn’t want him to see my head. Somehow it was more personal, more private, more embarrassing to me than the fact that he not only saw, but touched, drew on, and even photographed my breasts on a regular basis during reconstruction. Those interactions were scripted. Defined. But my head? I hadn’t realized he was going to see that. And there was embarrassment there. It wasn’t happening on my terms.
So today I am taking control and doing it on my terms. When Melissa Etheridge performed bald at the Grammys in 2005 (before I was even diagnosed) I remember thinking, “She is strong. She is real. She is brave. She is beautiful.” What she did in that moment was important. I bet it was liberating to her. So I’m going to try it. It’s too late for me to try it in reality (and I don’t want to pull a Britney Spears and shave my new hair off to be bald again).
Today is the 2 year anniversary of the day I finished chemo. So, in celebration, I’m taking off my metaphorical scarf. I’m going bald here today. I want to see how it feels.
January 10th, 2011 §
January 30, 2009
I had two surgeons that day:
one just wasn’t enough for the job.
The surgical oncologist would take away,
the reconstructive surgeon would begin to put back.
Before I headed off into my slumber,
I stood as one marked me with purple marker.
He drew,
he checked,
he measured.
And then a laugh,
always a laugh to break the tension:
Surgeons must initial the body part to be removed to ensure
they remove the correct one.
But what if you are removing both?
How silly to sign twice,
we agreed.
And yet he did,
initialing my breasts with his unwelcome autograph.
The edges of the yellow fabric measuring tape he used
had purple fingerprints up and down their sides;
use after use had changed their hue.
And now it was my turn to go under the knife–
a few more purple prints on the tape.
I got marked many a time by him that year.
Endless rounds of
purple dots,
dashes,
and lines
punctuating my body
with their strange, secret blueprint
only those wearing blue understood.
We stood in front of mirrors
making decisions in tandem
as to how my body should and would take new shape.
Two years today and counting.
Moving forward.
Sometimes crawling,
sometimes marching,
and sometimes just stopping to rest
and take note of my location.
Numb inside and out,
but determined.
Grateful,
hopeful,
often melancholy.
Here comes another year
to put more distance
between
it and me.
Let’s go.
January 7th, 2011 §
I’ve referred to Judy Clement Wall’s blog a few times… on Fridays she does a wrap-up of things she’s read and seen and thought about during the week. This week she found a YouTube video clip on “11 Words for 2011” and gave her own. I have many serious topics to write about soon, but first I decided to join Judy in doing my 11 words. I would love to hear yours: it literally only takes a minute or two. A while ago I did an alphabet and loved doing that exercise too. I bet it will be interesting to look back on them at the end of the year.
Not sure if these are supposed to be wishes, or hopes, or the first thing that pops to mind.
1. cancer
2. hope
3. health
4. love
5. friends
6. Twitter
7. books
8. blog
9. family
10. coffee
11. smiles
That’s what came to mind… how about you?
January 6th, 2011 §
Some days I say to myself, “Enough with cancer.”
Some days I say, “That’s enough. No more.”
No more thinking about it.
No more doing.
No more helping.
No more advocating.
No more educating.
No more communicating.
But then I say, “There’s still so much to do.”
There’s still so much to say.
There’s still so much to hope for.
There are still so many who suffer.
And so I am pulled back in,
Writing, talking, sharing.
Some days I want to talk about anything but cancer.
But I remember this is the new me,
This is my new life.
This is who I am.
And as long as there are others who come after me,
I will do what I can…
to hear,
to help,
to hope.
December 30th, 2010 §
One of my favorite romantic movie moments occurs between Denys (Robert Redford) and Karen (Meryl Streep) in the movie Out of Africa. The two lovers are out in the African desert at a fireside camp. Karen leans her head back into Denys’s hands. He washes her hair gently, then cradles her head in one hand and pours water from a pitcher, slowly and gently rinsing the soap from her hair after he’s done washing it. It’s a tender moment, to me utterly soft and sensual.
Before I left the hospital after I had a double mastectomy, the staff told me I might not be able to lift my arms over my head. With both sides affected, they said, I’d likely be unable to wash my own hair.
Recovery is slow in the week after surgery. A clear thin tube (like aquarium tubing) is literally sewn into a small hole in the skin under each arm. It carries excess fluid away from the mastectomy site as it heals. Fluid is collected into a small “bulb” and measured every few hours. After certain medical criteria are met, the drains are removed, the incisions sewn up, and then you can finally take that longed-for shower. Eight days after the surgery I received the all-clear. As any mastectomy patient will tell you, the day you get your drain(s) out is a great day.
Only then did I try to lift my arms. And hurt it did. I tried to shrink down into my body. I tried to be a tortoise withdrawing my head back inside my shell, shortening my height so I wouldn’t have to lift my hands so high to reach my hair. It was a painful challenge. I worked up a sweat trying to get my fingers to touch my scalp. I knew it was a questionable proposition. But I thought I could do it.
I thought about that scene— that romantic tender scene from Out of Africa. And I started laughing. I laughed and I laughed and tears came down my face. That cry hurt. It was one of those “I’m laughing and I’m crying and I’m not sure if it’s funny or sad or both and I don’t want to think about it so I’ll just go with it and I hope I’m not on Candid Camera right now…”
I was laughing at the absurdity of it. Here I was. It was my chance to get Clarke to wash my hair. My big fantasy moment. I was going to be Meryl Streep and he was going to be Robert Redford and he was going to wash my hair. Except I couldn’t move without pain. And I certainly wasn’t feeling romantic. I had just had my breasts removed. And I had these weird temporary breasts (tissue expanders) in their place. And my chest was numb. And my underarms hurt from having tubes in them for a week.
Because I hadn’t properly showered I still had purple Sharpie hieroglyphics all over my chest. And I had no nipples. And I had big scars and stitches in place of each breast. And a small angry scar with stitches under each armpit where the drain had just been removed. Let me tell you… this was clearly not how I envisioned beckoning my loving husband to come make my little movie scene a reality.
Now, don’t get me wrong. Had I called him from the other room, he would have done it in a second. He would have been there for me, washed my hair, and not made me feel the bizarre, odiferous (!) freak I felt at that moment. And I would have loved him for it. But I did not want him to see me like that.
In that moment I had a dilemma. What kind of woman was I going to be?
What kind of person was I going to be with this disease from that moment going forward?
I was going to push myself. Do it myself.
I wasn’t going to be taken care of if I could help it. I knew I was going to have trouble asking for help, have trouble accepting help. I knew these things were going to be necessary. But I also knew they were going to cause me problems. That’s the kind of person I am.
I knew asking for and accepting help were actually going to make me feel weaker than I was already feeling. And it was only the beginning. I knew these actions were going to make me feel weaker than I knew I was going to get. I wanted to do everything myself for as long as I could. That was what was going to make me feel alive: doing it myself.
I am not sure I did the best job washing my hair. I probably missed a spot or two. But I did it. And I didn’t ask for help.
Granted, it was something small.
But in that particular moment, on that particular day, that particular act gave me a feeling of pride as big as anything else I could have possibly accomplished.
a postscript: I wish I had been more accepting of help in the early days. I wish I had not seen it as a personal “weakness” the way that I express here. I don’t want to change what I wrote then, but I do want to say that I don’t think I was right to push myself so hard. If I had it to do over again I would accept help more often; maybe not for the hair-washing, but definitely for other tasks that I should have outsourced. I have learned from my experience.
December 24th, 2010 §
Originally written December 25, 2008
(three weeks after my salpingo-oophorectomy and two years after my diagnosis of breast cancer. This was actually the first blogpost I ever wrote.)
I’ve only cried once today. That’s not too bad. But the day is not yet done. Today, again, I’m thinking of the things that cancer has taken from me. First, let me say that I am well aware of the blessings I have. I remember them each and every minute of every day. They are what keeps me going, keeps me fighting. But today, again, I’m pulled into what’s gone, what’s irretrievable, what’s changed.
The body parts are gone, of course. My feeling of immortality. Of safety, of security. I’m vulnerable now. And I feel it. Part of me wants to blaze down I-95 at 100 miles an hour because I’ve stared down cancer, so what can touch me now? Taking risks is a popular grief reaction. On the other hand, a part of me wants to curl up in bed and not come out.
Today, on Christmas, when the childlike wonder is all around, I feel like I am watching it from high above me, as it happens TO ME, around me. I smile, I do what I am supposed to do, I play the “Santa game” with my children. I eat delicious food. I gather up the gift wrap strewn about the living room. I pile the presents in the kids’ rooms. I pack their suitcases for their 3:30 a.m. wakeup for their winter vacation. Half my family is leaving me tomorrow. They’ll be back, of course, but they are leaving. And while they are gone I will ponder the sadness that has settled like a cloud since my latest surgery almost a month ago.
I know I’ll be fine… everyone tells me so, as if to will it to be that way. Even in my darkest moments I know it is only temporary. But I am angry at cancer. Angry at the bad twist of fate that makes me unable to travel this year, unable to be myself, unable to shake this feeling that the dark cloud just seems to keep following me, like those creepy paintings in the museum whose eyes seem to follow your every move.
And knowing the other people who are similarly sad today, those who are remembering loved ones lost, and those who are suffering in pain, and those who will head in for more chemo and surgery and therapies before the year is out are also forever changed by the great equalizer of cancer.
To anyone who reads this and thinks it sounds so odd, so foreign– something that happens to “someone else”… I am so happy for you. I am jealous of you. I remember that feeling, but I am almost getting to the point where I am unable to remember it. I never thought it would be me thinking this way, feeling this way. But it is me. And it’s taking a long time to grieve for that life I thought I would have.
Maybe that’s what it is.
I’m in mourning.
I’m mourning the life I thought I would have.
And only time can help that.
December 22nd, 2010 §
If you knew me, you would know I am resilient. Tough, even in the face of the worst news. You would know I rise to the occasion every time. I might break down before, I might break down after– certainly after. But I will meet the challenges at each and every turn.
If you knew me you would know I smiled my way through many of my hard times, lied and smiled and said “fine” when many a person asked, “How are you?”
If you knew me you would know I am not a negative person, that I am not a pity-seeker, nor a martyr. You would know that I just do the best I can, and want to be dignified and strong, but am not in denial.
If you knew me you would know I love to do things for others, moreso than myself. You would know that in this turbulent portion of my life I have done what I can to show others what they mean to me, and how much I appreciate the kindness of strangers… how the smallest encounters can stay with me forever.
If you knew me you would know that I tried my best to make others feel at ease with my cancer. I always took pride in looking the best I could with what I had left. I created outfits around my scarves, and learned how to draw in eyebrows so that it wouldn’t be too obvious I had none. I tried to set a good example for my children, being honest with them about what was happening, loving them as much as I could, and asking the others who loved them to help them feel special and safe.
If you knew me you would know I care for others. When fellow cancer patients have asked to see what reconstruction looks like, I place my pride and embarrassment aside to honor their needs, their fears, their emotions. While some might (and do) hide their illnesses, I cannot. I have chosen for myself, and for my children, to be open about what cancer is, what it does, what price it demands. I believe that being this way will reduce the shame, the fear, and the confusion for them. Nothing has been more important to me than making sure my children understand what is happening and what the scientific reasons are. That honesty does not come at the expense of hope. Of optimism. Of sheer will. To remain mum about these feelings, these thoughts, these explanations of my experience, is to deny my life for the past four years. To do so says the suffering, confusion, and fear were ill-placed. To avoid talking about the reality of the dangers, the problems, the down-times is to not only be in denial but also to assert that my fears are irrational.
If you knew me you would know that I write not because I wallow in darkness, or think negative thoughts all the time. If you knew me you would know I write so that the emotions can be explored, pushed, pulled, twisted, and shared in order for me to be positive, optimistic, and strong for the rest of the world to see. It is the sharing of these ideas on paper, and sometimes reaching the hoped-for connection to people who read them (whether because they resonate with you, move you, educate you, or make you thankful that you have no idea what the cancer experience is) that keeps my words flowing.
If you knew me you would know I’m just a person, doing the best I can with what I’ve got.
Maybe it’s a bum rap, but it’s my bum rap.
It’s my chance to show what I can do:
Just watch me.
December 20th, 2010 §
Four is just a word. So is three. But once again today I will change one word on the welcome page of my website.
“It has been three years since hearing the words ‘You have cancer,'” the first sentence says.
And now, today, it becomes four.
I think about days like the one four years ago — days that start innocently, normally, benignly. In the hours leading up to the mammogram I wasn’t worried about anything.
I think about the sentence that changed my life.
I think of where I’ve been, where I am, where I am going.
I think of those I’ve met along the way: new friends, doctors, nurses, strangers.
I think of those who have died from cancer and other causes since I was diagnosed.
I think of the progress we’ve made and the distance we have yet to go.
I think of what today might bring, and tomorrow.
And then, in a sudden reversal, I stop myself from thinking too much.
“It’s time to go live my life,” I tell myself. Thinking is good, but only so much.
“It’s time to go live my life,” I tell myself…
Right after I change that one word.

To read about the chronology of my diagnosis, go here.
December 17th, 2010 §
originally published September 12, 2009
My friend Andrea found out she needs to have chemo. I cried a lot the day I found that out. Last night she emailed me that she was thinking about the whole “losing her hair” thing. She has gorgeous hair. Thick. Straight. Reddish-brown, in the sun I’d say it has a honey shine in it. She usually wears it back in a ponytail, as she says, “taking it for granted.”
I started writing her back to tell her that focusing on her hair wasn’t silly. There are many things about cancer that are real worries. One of them is going bald. Especially for a woman. And as I typed to her I realized the words were flowing fast and furious.
I realized all the things people had said to me when I was worried about losing my hair and all of the things people had said to me after it eventually happened.
Everyone wants to reassure you that it isn’t as bad as you think it is.
Some days you convince yourself it isn’t that bad.
Some days you are sure they are all lying to you.
Either way, you get through the days.
The day you take that hat or wig or scarf off and wear your newly-grown stubble or “mouse fur” out in public is a great day (My first hair was so fine and soft and thin that it didn’t resemble hair at all… I called it mouse fur because while it blissfully covered my head and was dark, it couldn’t be cut or styled).
So, for my friend, and for other women who are getting ready to start chemo (and those who bravely walk through the world every day without hair because of alopecia and other conditions), no matter what, it matters.
No matter what anyone says…
all the things they will say:
It’s only hair.
It’ll grow back.
You’ll look so pretty anyway.
With a face like yours it won’t matter.
We’ll get you a cute wig.
We’ll get great scarves.
It’ll grow back in no time.
Maybe it’ll be better after it grows in.
It might be curly.
It might be straight.
I know someone whose hair came in gray.
I know someone whose hair came in red.
I know someone whose hair came in black.
I know someone whose hair came in white.
Hers came in curly.
Hers came in straight.
Did you see hers?
It looks great.
Did you see hers?
It looks awful.
I like her better with short hair.
I liked her better with long hair.
You’re gonna look great.
I don’t know what I’d do.
I don’t know how you do it.
I don’t know how you’re gonna do it.
You are so brave.
You are so strong.
You can do it.
You can beat this.
No matter what anyone says–
It is just going to suck.
Bigtime.
You may shed many tears over this one.
It may be harder than you thought.
I’ve heard brave women say it was harder than the actual chemo.
Reports show women actually turn down the chemotherapy they need because they don’t want to go bald.
It’s real.
It’s hard.
If it weren’t,
Women wouldn’t cover their heads.
They would just walk around bald.
They wouldn’t care.
But hair matters.
To us,
To our kids,
To our husbands,
To our friends.
My hair has never been the same since chemo.
I’m not alone in that.
In fact,
My hair now grows “the other way”…
My part is on the opposite side of my head than it used to be.
I think that’s kind of neat.
There’s the way my hair was B.C. (before cancer)
And the way it is now.
It is a big deal.
Don’t let anyone minimize it.
If they do, make them go shave their heads.
Not just clipper cut.
Straight razor shave it until there’s nothing left.
Then the eyebrows.
Then the eyelashes.
And then the stuff they might not think about.
Every piece of body hair.
Of course there are jokes.
And giggles.
The Brazilian wax done for you.
It’s funny.
But not so funny.
Then when your nose hairs fall out you suddenly realize how
Much you needed them.
Your nose runs constantly.
And it’s embarrassing.
Mine dripped clear liquid constantly.
I was so embarrassed.
No one had told me about that part.
I had a tissue stuffed in every pocket.
Because there were no hairs to stop the drip.
Chemo drip.
You try to imagine what it will be like.
You try to picture what you will look like bald.
You pull your hair back,
Slick it back,
Try a wig on to see what it might look like.
But nothing can prepare you.
For that crappy day,
Two weeks in.
When you scratch an itch
Or touch your head
And take away a handful of hair
Or find it on your pillow.
And the sight of it is so sad,
But so disgusting
So repulsive,
That you need it gone.
And then if you need me
You will call me.
And I will come.
And I will cut it.
Or maybe I will just come and cry with you.
And remember what it felt like.
No matter what anyone says,
It isn’t nothing.
It is something.
And even in the scheme of all of the things to be afraid of with cancer,
How you feel about losing your hair is real.
It matters.
And I remember.
December 15th, 2010 §
5.2.2009
He caught me before I could put on my bright smile, restore the gleam in my eye, the flirt in my face.
He caught me lost in my disconnect, my swimming, floating, drowning.
“Are you okay?” he asked gently.
So gently I almost didn’t hear.
So gently it didn’t rouse me.
I stayed in that liminal state, half awake, half asleep.
Dozing in daylight.
Autopilot.
“I’m fine, thank you. Just tired,” I covered.
“I just wondered,” he said. “You don’t seem like yourself.”
“Thank you. Thank you for worrying. That’s so kind.”
Am I so transparent, I wondered. So transparent that this man who doesn’t even know my name can tell without a word when I’m not feeling well?
I turned my attention back to him.
“How can I help you?” he asked as someone approached and interrupted our conversation.
“Muenster cheese, please,” I requested of him. “A half pound.”
December 8th, 2010 §
Today I was interviewed in The Washington Post about my perspective on the news of Elizabeth Edwards’s death. Melissa Bell’s article is entitled “Elizabeth Edwards and the cancer question.” Click on the title to read the piece on the Post website.
Thanks so much to all of you who read the two pieces I wrote about Ms. Edwards and passed them on to friends:
On Resilience and Why I’m Crying.
Your comments mean so much.

December 7th, 2010 §
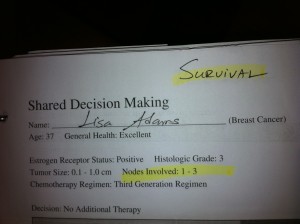 Doctors diagnosed my mother with breast cancer the exact same day Elizabeth Edwards heard those words in November, 2004.
Doctors diagnosed my mother with breast cancer the exact same day Elizabeth Edwards heard those words in November, 2004.
Two years later, I too received a diagnosis of breast cancer.
After my diagnosis I went for consultations with two oncologists. Each doctor handed me two pieces of paper displaying bar graphs of the risk of my cancer returning and the risk that I would die from my cancer. These risks were broken down and calculated for four separate conditions: 1) if I did nothing, 2) if I received chemotherapy, 3) if I received hormonal therapy, and 4) if I received “combined” therapy (chemotherapy + hormonal therapy). On the top of the stark white pieces of paper in my doctor’s writing it says “Survival” on one and “Recurrence” on the other.
I made my decision rather easily: to treat my Stage II cancer I opted for a double mastectomy, chemotherapy, and adjuvant hormonal therapy. I had a husband and three young children; I wasn’t taking any chances– I would do whatever it took to get me into remission and give me the best possible chance of survival.
My mother, because of the particulars of her Stage III cancer opted for a lumpectomy, radiation, and chemotherapy.
And so, my mother and I had different treatment plans. But while our treatment protocols differed, we both required the same character trait to get us through: resilience. Appropriately, this is also the title of Elizabeth Edwards’s book.
Resilience has carried me through my mother’s diagnosis and mine. My son Tristan’s surgeries and treatments for congenital spine and hand deformities. The sudden death of my beloved mother-in-law in a car crash one year ago.
Resilience is the ability to bounce back, the ability to find strength and reserves when you think there are none, the guts to wake up each morning and, knowing something else might be just around the corner, say, “Okay, world, bring it on. I can take it.”
It’s also the manner in which you take it. Do you feel defeated? Resigned? Depressed? Angry? Do you channel those negative emotions into something positive?
Some people believe that negative things like cancer and grief are gifts. Books I’ve seen preach that you should change your thinking: these events are not traumas or tragedies; they are gifts, positive intrusions into your life.
I don’t think so.
I don’t think cancer is a gift.
I don’t think grief is an opportunity.
I think these things suck.
I think they hurt.
There’s a difference between thought and action: what you do with those feelings is what counts.
People don’t need to have the same beliefs or think the same way to feel a magnetic pull to one another.
Resilience is like a magnetic pull to life, a force that keeps me coming back for more
with grit,
determination,
heart,
hope.
Resilience whispers in my ear,
“You can do it.
Just keep going.
One foot in front of the other.
It will get better.
And, if it doesn’t, well…
you can take it.
Bring it on.”
Elizabeth Edwards reached many people because she was in the public eye, but inspirational people also live quiet lives. We can be inspired by Edwards’s grace and courage as she dealt with the challenging parts of her life in the same way we can find inspirational people around us each and every day. These are all people we can connect with and learn from. In doing so, we better ourselves. In doing that, we honor their struggle.
My mother is alive, and in remission. And the joy that I feel about having my own mother here is shared in equal measure by the sorrow I feel for Ms. Edwards’s three living children, Catharine, Emma Claire, and Jack, over the loss of their mother.
December 7th, 2010 §
I didn’t know Elizabeth Edwards. In fact, I wrote a piece critical of her when she initially stood by John after his affair. I was disappointed when she gave an interview on CNN in May of 2009 and spoke only of John’s “imperfection” rather than calling him the cheater he was and kicking him to the curb. I was angry she hadn’t used her interview time to talk about herself, her cancer, her life: the topics I wanted to hear about. I was angry at her for not claiming her remaining years of life as her own.
So why am I sitting with tears in my eyes because she has died?
I cry because it makes me feel vulnerable and scared of what this disease can do to me: what it did to her.
Yes, I know… there are plenty of men and women who get cancer, have treatment, and stay in remission for the rest of their lives. And, in essence, isn’t that what every cancer patient hopes for, as Betty Rollins wrote, “to die of something else”?
I don’t think it makes me pessimistic, depressing, or negative to think that I am vulnerable.
It’s the truth. It’s my truth.
Anyone who hasn’t been to the oncologist with me to see my risk-of-recurrence charts, my mortality charts, my decision-making discussions along the way can’t say to me “Oh, don’t worry, that won’t be you.” No one, including me, knows how it will go.
People tell me: stay strong, just think positive, you can’t generalize from her situation.
I respond: I am strong, I hope for the best. I don’t think positive thinking is going to save me if there are remaining cancer cells still in me.
I hope that people won’t say to someone who has been diagnosed with cancer, “Don’t worry, what happened to Elizabeth Edwards won’t happen to you.” Because while we do everything we can to ensure we die of something else, it just isn’t always the case. In 2006 her oncologist told her that there were many things going on in her life, “but cancer was not one of them.” Things change quickly, cancer can recur when you least expect it.
I have sympathy for her family. I cry for her children. I am saddened about the years she spent with a man who didn’t deserve her. I am angry about the time she wasted on him. I hoped she would be an example of someone who would keep cancer at bay.
I grieve for that hope, now gone.
December 2nd, 2010 §
In August, the editors at Cancer Bone Health asked me to write a blogpost for their launch. Today it went up on their new website.

click here to read it:
Standing straight: Words of welcome from a survivor
The profile piece they wrote about me and posted a few days ago appears here.
December 1st, 2010 §
 August 18, 2009
August 18, 2009
Summers bring change. The end of the summer signals the start of school for children, and for some it’s their first day of school ever. My youngest child, Tristan, will start nursery school in a few weeks. This month has brought the inevitable developmental milestones of potty training and sleeping in a big bed. My oldest child, Paige, will start middle school. She went to sleepaway camp for the first time this summer (and loved it). My middle child lost his first two teeth.
As I sit and watch and listen to the waves on our beach vacation I know the summer is drawing to a close. Some of you reading this are already sending your children back to school.
The months and years go by. Like all of you I mourn the quick passage of time. “Where did the summer go?” I hear my friends asking. Projects we hoped would be accomplished — tasks we hoped would be done — sit unfinished. Organizing photos, cleaning out a closet or a room, or reading that book a friend recommended; many things went undone in the last eight weeks.
Maybe you were lazy, maybe other things came up, maybe you were preoccupied with family obligations. Maybe you had an unexpected cancer diagnosis, maybe you got the flu, maybe your parents’ health was sub-par.
Regardless the reason, there can be a bit of disappointment when summer ends. The children we send back are taller, older, more mature. They’ve had lots of experiences to tell their friends about. Maybe they’re in a new school, maybe they’re now the oldest in school, maybe they’re now the youngest. New bus routes, new starting times, new friends, new backpacks, new teachers.
Some children will be starting back with a new experience to tell their teacher and friends: “This summer my mommy got cancer.” That one will not be an isolated instance, unfortunately; women around the country will be sending children to school with that summer report.
Growth happens in fits and spurts, not with smooth sliding grace.
With each phase comes
pain,
discomfort,
unease.
Restlessness,
sleeplessness,
yearning.
When I had the tissue expanders in my chest to make room for the implants that would replace my breasts after the mastectomies, every week my plastic surgeon would add to them. And each time after a “fill” they would feel tight. The skin would not be big enough for the volume inside, and it would react. The skin would feel the pressure and grow, that was the point of the process. Until the skin could replicate there was achiness, tightness, a ripping or tearing feeling.
A similar sensation happens during the days during pregnancy when you feel your belly just can’t accommodate the growing baby inside it. And yet it does. If it happens too fast you get a stretch mark, a sign your skin just couldn’t keep up. The growth was too rapid, too harsh, too vigorous.
I often wonder if mothers and fathers get psychological stretch marks when we are asked to accommodate changes we’re not quite ready for.
What can we do? What options do we have? None. We must “go with the flow” and do the best we can. Our children grow and change whether we like it or not. We do them no favors by trying to protect them, coddle them, and keep them young. We give them wings to fly when we give them tools to be
confident
and caring
and inquisitive
and trusting
individuals.
I am moved to tears as I watch my children grow.
I am moved by the succession of infancy, childhood, and adolescence.
I know that as a mother I lack many skills I wish I had.
But I also know that the words I have written in my blogs and essays will one day be a gift to them too.
Not a gift to the children that they are, but instead a gift to the adults that I am raising them to be.
Each August or September as they go back to school I marvel that another school year has passed and yet another is here.
I mark time differently now. I mark anniversaries not of weddings, but since diagnosis, since mastectomies, since chemotherapy began and since it ended, since implants, since Tamoxifen, since Arimidex, since oophorectomy. They are not just dates; they have meaning. They are meaningful for doctor visits and tests I must have done and dates I can stop taking drugs and dates I must know for other treatments.
No matter how you measure time it always goes too fast.
The growth happens too fast.
And the growing pains hurt for me.
The stretch marks might be invisible this fall, but they are surely there.
November 30th, 2010 §
I spent this afternoon at Sloan Kettering meeting with my consulting breast oncologist. I learned a lot of new information about estrogen loss after my surgical menopause two years ago. I’ll write more about what I learned at that meeting in future days.
I had a long trip home from New York City after there was an engine fire on the train I was riding on. Once home, however, I was happy to discover that an interview I gave for a new website on bone health after cancer was published!
 Click here to read the piece.
Click here to read the piece.
November 23rd, 2010 §
Originally published June 24, 2010
There comes a point in your life when you realize that your parents are people too. Not just chaffeurs, laundresses, baseball-catchers, etc.– but people. And when that happens, it is a lightbulb moment, a moment in which a parent’s humanity, flaws, and individuality come into focus.
If you are lucky, like I am, you get a window into that world via an adult relationship with your parents. In this domain you start to learn more about them; you see them through the eyes of their friends, their employer, their spouse, and their other children.
Yesterday I sat transfixed reading Katherine Rosman’s book If You Knew Suzy: A Mother, A Daughter, A Reporter’s Notebook cover to cover. The book arrived at noon and at 11:00 last night I shut the back cover and went to sleep. But by the middle of the night I was up again, thinking about it.
I had read an excerpt of the book in a magazine and had already been following Katie on Twitter. I knew this was going to be a powerful book for me, and I was right. Katie is a columnist for The Wall Street Journal and went on a mission to learn about her mother after her mother died (on today’s very date in 2005) from lung cancer. In an attempt to construct a completed puzzle of who her mother was, Katie travels around the country to talk with those who knew her mother: a golf caddy, some of her Pilates students, her doctors, and even people who interacted with Suzy via Ebay when she started buying up decorative glass after her diagnosis.
Katie learns a lot about her mother; she is able to round out the picture of who her mother was as a friend, an inspiration, a wife, a mother, a strong and humorous woman with an intense, fighting spirit. These revelations sit amidst the narrative of Katie’s experience watching her mother going through treatment in both Arizona and New York, ultimately dying at home one night while Katie and some family members are asleep in another room.
I teared up many times during my afternoon getting to know not only Suzy, but also Katie and her sister Lizzie. There were so many parts of the book that affected me. The main themes that really had the mental gears going were those of fear, regret, control, and wonder.
I fear that what happened to Suzy will happen to me:
my cancer will return.
I will have to leave the ones I love.
I will go “unknown.”
My children and my spouse will have to care for me.
My needs will impinge on their worlds.
The day-to-day caretaking will overshadow my life, and who I was.
I will die before I have done all that I want to do, see all that I want to see.
As I read the book I realized the tribute Katie has created to her mother. As a mother of three children myself, I am so sad that Suzy did not live to see this accomplishment (of course, it was Suzy’s death that spurred the project, so it is an inherent Catch-22). Suzy loved to brag about Katie’s accomplishments; I can only imagine if she could have walked around her daily life bragging that her daughter had written a book about her… and a loving one at that.
Rosman has not been without critics as she went on this fact-finding mission in true reporter-style. One dinner party guest she talked with said, ” … you really have no way of knowing what, if anything, any of your discoveries signify.” True: I wondered as others have, where Suzy’s dearest friends were… but where is the mystery in that? To me, Rosman’s book is “significant” (in the words of the guest) because it shows how it is often those with whom we are only tangentially connected, those with whom we may have a unidimensional relationship (a golf caddy, an Ebay seller, a Pilates student) may be the ones we confide in the most. For example, while Katie was researching, she found that her mother had talked with relative strangers about her fear of dying, but rarely (if ever) had extended conversations about the topic with her own children.
It’s precisely the fact that some people find it easier to tell the stranger next to them on the airplane things that they conceal from their own family that makes Katie’s story so accessible. What do her discoveries signify? For me it was less about the details Katie learned about her mother. For me, the story of her mother’s death, the process of dying, the resilient spirit that refuses to give in, the ways in which our health care system and doctors think about and react to patients’ physical and emotional needs– all of these are significant. The things left unsaid as a woman dies of cancer, the people she leaves behind who mourn her loss, the way one person can affect the lives of others in a unique way… these are things that are “significant.”
I woke up in the middle of the night thinking about the book. My head spun with all of the emotions it raised in me. I think that part of the reason writing has become so important to me is precisely because I do realize that we can die at any moment. And if you don’t have an author in the family who might undertake an enormous project as Katie did, where will that explanation of who you were — what you thought — come from?
Is my writing an extension of my desire to control things when cancer has taken away so much of this ability?
Is part of the reason I write an attempt to document my thoughts, my perspective for after I am gone… am I, in a smaller way, trying to do for myself what Katie did for her mother?
If I don’t do it, who will do it for me?
And in my odd way of thinking, am I trying to save anyone the considerable effort of having to work to figure out who I was– deep down?
My blog has the title “You’d Never Know”: I am telling you things about myself, my worldview, and my life, that you would otherwise have no knowledge of. One of the things people say to me all the time is, “You’d never know to look at you that you had cancer.” After hearing this comment repeatedly I realized that much of our lives are like that:
If we don’t tell someone — share our feelings and experiences — are our lives the proverbial trees falling (unheard) in the forest?
What if you die without being truly understood?
Would that be a life wasted?
If you don’t say things for yourself can you count on others to express them for you?
Further, can anyone really know anyone else in her entirety?
After a loved one dies, there always seems to be at least one mystery person: an individual contacts the family by email, phone, or in person to say, “I knew your loved one: this is how I knew her, this is what I remember about her, and this is what she meant to me.” I know that this happened when Barbara (my beloved mother-in-law) died suddenly last fall. There are stories to be told, memories to be shared. The living gain knowledge about their loved one. Most often, I think families find these insights comforting and informative.
Katie did the work: she’s made a tribute to her mother that will endure not only in its documentation of the person her mother was (and she was quite a character!) but also in sharing her with all of us. Even after her death, Suzy has the lovely ability to inspire, to entertain, to be present.
I could talk more about the book, Katie’s wonderful writing, and cancer, but I would rather you read it for yourself. I’m still processing it all, making sense of this disease and how it affects families, and being sad that Katie’s children didn’t get to know their grandmother. Katie did have the joy of telling her mother she was pregnant with her first child, but Suzy did not live long enough to see her grandson born. In a heartwarming gesture, Katie names her son Ariel, derived from Suzy’s Hebrew name Ariella Chaya.
I thank Katie for sharing her mother with me, with us. As a writer I learned a lot from reading this book. I’ve said many times recently that “we don’t need another memoir.” I was wrong. That’s like saying, “I don’t need to meet anyone new. I don’t need another friend.” Truth is, there are many special people. Katie and Suzy Rosman are two of them.
January 14th, 2010 §
I wish I had the energy of my youth.
I wish I had the body.
I wish I had the fearlessness, the spunk, the drive.
I wish I could have a conversation with that young girl,
bright-eyed and full of wonder.
I wish I could tell her what lay ahead.
I wish I could tell her to gather strength, and wisdom, and patience like a squirrel gathering acorns for the winter.
“Save those things up,” I’d say, “you are going to need them… every last bit.”
I wish I could share the perspective I’ve gained along with all of the love.
But I can’t go back to that time,
I can’t go back to that place.
I can’t rewrite what’s happened,
I can’t do it all again.
I guess I must have done something right along the way for when it came time to fight I did,
and I did it well.
But that struggle took its toll on me and I am quite sure I will never, ever be the same.
You tell yourself “they’re only breasts.”
You say, “I don’t need ovaries, I’m done having children.”
But that obscures the truth.
The truth is that it does matter,
they do matter.
They say my uterus is atrophied.
It almost sounds funny when you say it.
“Who cares? What does that matter?”
It does. It does. It does.
To get rid of all hormones gives me a better chance at avoiding a recurrence, but there is a price to be paid.
No estrogen matters more than I ever thought it could.
It feels worse than taking injections to suppress my ovaries, worse than taking Tamoxifen. Those were easy. I had no clue what was ahead.
I wear the skirt, I put the makeup on, I walk the walk.
But I do not feel like a woman anymore.
I’m proud of what this body has done for me:
3 beautiful children,
surviving cancer,
healing the broken bones, the infections, the autoimmune diseases.
There is no week without migraines,
no cold winter day without icy implants.
Beneath the pretty lies ugly,
the ugly truth of cancer
and what it has taken from me.
While some may be able to go on,
move on,
forget,
I cannot.
My body will not let me.
These things are not tied with a pink ribbon.
These things last longer than a month.
This is part of awareness.
This is part of what breast cancer can do.
This is what it has done to me.


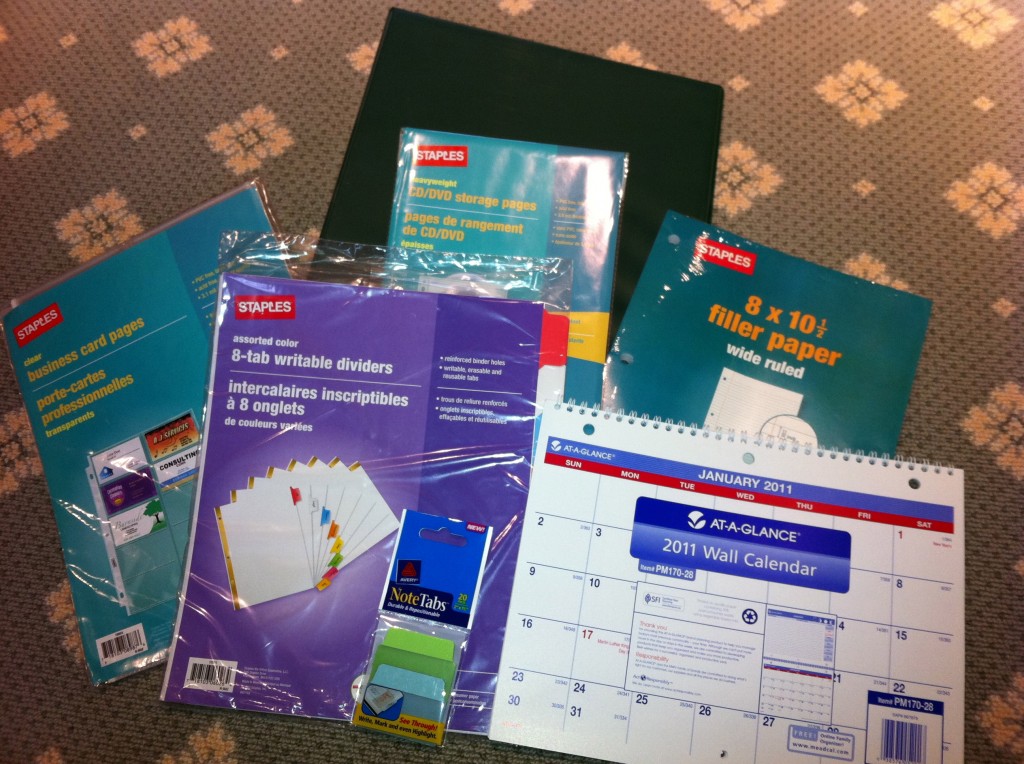

 I remember distinctly sitting in movie theaters when I was pregnant. At various points throughout the film I’d tune out the words and images and get lost in my belly, feeling each of my children squirm and wriggle and stretch. “What if this is it?” I’d think to myself. “What if I go into labor right here, right now?” And then I’d think to myself, “In just a week or two I’ll be a mother, mother to a person whose body is inside mine but whose face I have not seen, whose voice I do not know, whose skin I have not touched. I’ll be mother to this person for his or her entire life, my life will be shaped by his, and his by mine.” And those thoughts seemed incomrehensible to me at the time. Too large, too vast.
I remember distinctly sitting in movie theaters when I was pregnant. At various points throughout the film I’d tune out the words and images and get lost in my belly, feeling each of my children squirm and wriggle and stretch. “What if this is it?” I’d think to myself. “What if I go into labor right here, right now?” And then I’d think to myself, “In just a week or two I’ll be a mother, mother to a person whose body is inside mine but whose face I have not seen, whose voice I do not know, whose skin I have not touched. I’ll be mother to this person for his or her entire life, my life will be shaped by his, and his by mine.” And those thoughts seemed incomrehensible to me at the time. Too large, too vast.
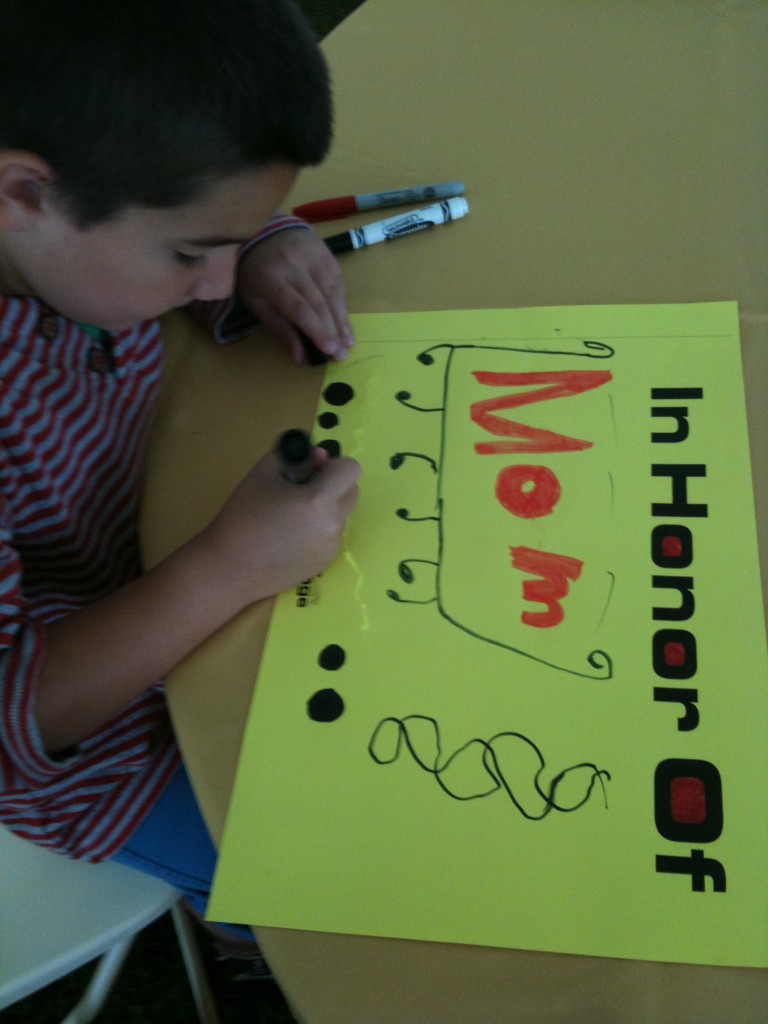



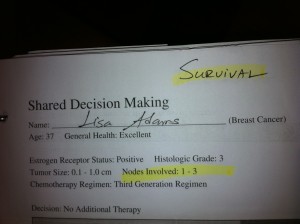



 Link to Twitter
Link to Twitter